Abstract
Introduction:
Non epileptic seizures (NES) are little reported in our country.
Case report:
We report 2 observations of 4 years old girls, with normal psychomotor development, and frequent paroxystic seizures, characterized by stereotyped movements of the members, occurring during sleep onset or deep sleep. Electroencephalogram Sleep records showed brief discharges of spikes and spikes-waves. Magnetic Resonance Imaging was normal.
Suspicion of NES associated with epilepsy was based on the following arguments:
mild regression of the seizures frequency after using antiepileptic drug
video records of the seizures strongly suggestive of masturbation seizures,
masturbation seizures are triggered by the girls and stopped on order,
best regression of the seizures frequency after adjunction of trihexiphenidyl.
Moreover, the authors make a review of literature on the NES.
Conclusion:
The early diagnosis of the NES allows to avoid the inadequate treatments and an improvement of the prognosis.
Author Contributions
Academic Editor: Prabhat singh, Assistant Professor, MGM Navi Mumbai, India
Checked for plagiarism: Yes
Review by: Single-blind
Copyright © 2017 MARIAM DOUMBIA-OUATTARA, et al.
 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Competing interests
The authors have declared that no competing interests exist.
Citation:
Introduction
Non-epileptic seizures (NES) is a descriptive term for a diverse group of disorders that refer to paroxysmal events that can be mistaken for epilepsy, but are not due to an epileptic disorder. “Non-epileptic seizure” is the preferred term. These include “hysterical seizures, pseudo-seizures, pseudo-epileptic seizures, non-epileptic pseudo-seizure, non-epileptic attack disorder, dissociative episodes” 1. In all cases, ‘seizures’ were also replaced by ‘fits’ and ‘attacks’” 2. This phenomenon is a frequent disorder, but late diagnosed with an average diagnostic of 7 years, what shows of the ignorance of this pathology. This diagnostic delay has several consequences on the patients and on the health system. A comorbid epilepsy is present in 15 in 20 % of the cases 3.
Few publications concern the management of these long term invalidating paroxysmal events 4. NES are little reported in our country. We report 2 observations of 4 years old girls, presented frequent paroxystic seizures, characterized by stereotyped movements of the members, occurring during sleep onset or deep sleep 3.
Observations
Case 1:The first girl, premature baby of 34 weeks of amenorrhea, 2nd child of a sibling of two children. Her psychomotor development was normal, without personal or family neurological histories. She presented since September 2014, brief episodes occurring several times a day during the sleep, of tonic contraction of lower limbs, with friction of hands on the public region. She remained aware during these episodes, because she answers the requests of her mother. The somatic neurological examination was normal. Electroencephalograms (EEG) Sleep records showed brief discharges of generalized slow spikes or spike waves (Figure 1), not been modified by photic stimulation. Brain Magnetic Resonance Imaging (MRI) was normal. The current treatment includes Trihexiphenidyl, Clonazepam and Carbamazepine results a notable regression of seizures.
Figure 1.Electroencephalograms (EEG) Sleep records showed brief discharges of generalized slow spikes or spike waves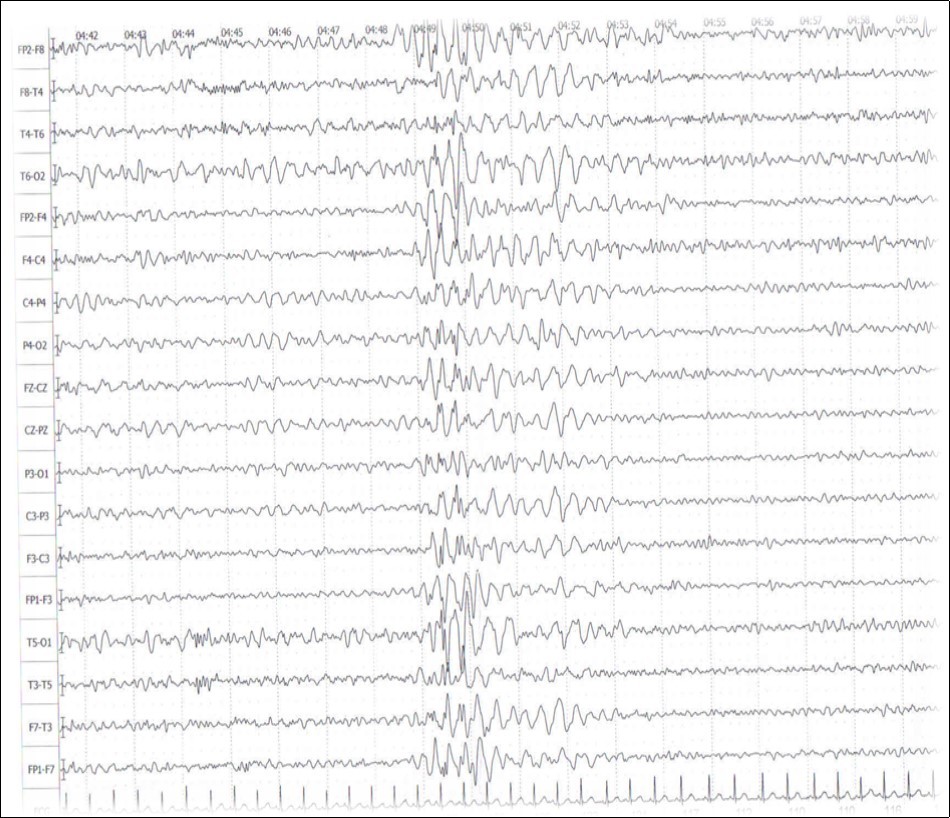
Case 2:The second girl, outcome of gemellary pregnancy, had a normal psychomotor development. Her twin sister presents a focal idiopathic epilepsy. She presented also brief episodes of tonic contractions of lower limbs during the sleepiness, accompanied with antero- and retropulsion movements of the pelvis. She feels coming the seizures which she indicates to her mother "Mom, I want to pull". The somatic neurological examination was normal. EEG Sleep records showed brief discharges of generalized slow waves and spikes (Figure 2), not been modified by photic stimulation. Brain MRI was normal. The current treatment includes Trihexiphenidyl and Carbamazepine, results a notable regression of crisis.
Figure 2.EEG Sleep records showed brief discharges of generalized slow waves and spikes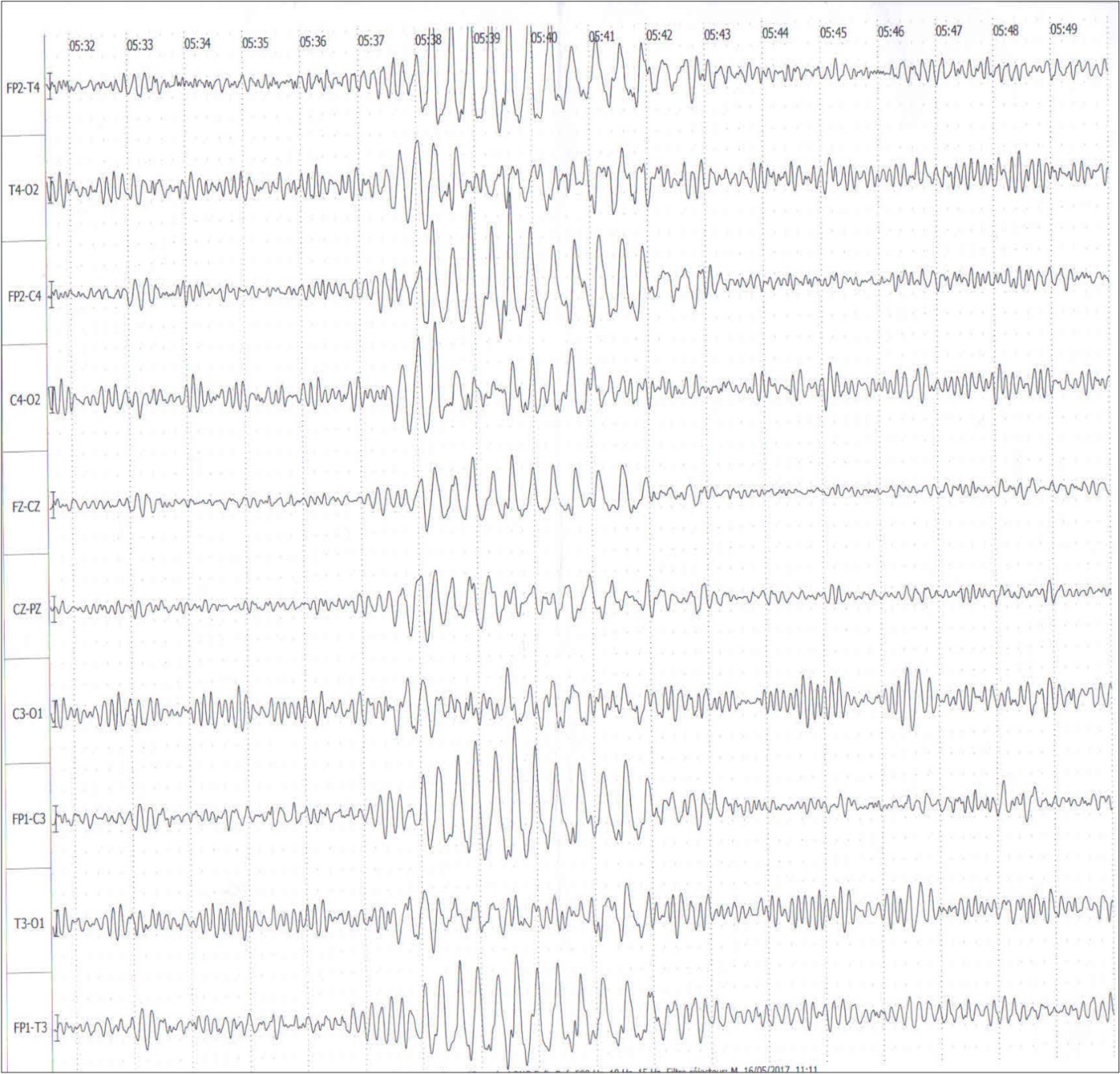
In the two cases, suspicion of NES associated with epilepsy was based on the following arguments:
- masturbation seizures are triggered by the girls and stopped on order,
- mild regression of the seizures frequency after using antiepileptic drug
- presence of epileptiform EEG abnormalities critical or intercritical
- video records of the seizures strongly suggestive of masturbation seizures,
- best regression of the seizures frequency after adjunction of trihexiphenidyl.
Commentaries
There are two sub-categories of non-epileptic seizures: “physiologic” and “psychogenic.” The physiologic group includes a broad spectrum of disorders, such as syncope, paroxysms of acute neurological insults, paroxysmal toxic phenomena, non-toxic organic hallucinosis, non-epileptic myoclonus, sleep disorders, paroxysmal movement disorders and paroxysmal endocrine disturbances. The psychogenic non-epileptic seizure (PNES) group includes a number of DSM-IV diagnostic categories, including the reinforced behaviour pattern, which is not DSM-IV identifiable, and relates to cognitively challenged patients who, paradoxically, have been reinforced for their PNES because of a simple, secondary gain in terms of controlling their environment 1. PNES are defined as paroxystic, transitory, clinical manifestations being able to contain motor, sensory, vegetative, psychological and/or cognitive signs, but which, contrary to the seizures, are not associated with a concomitant excessive cortical neuronal discharge. The semiological closeness of PNES with seizures and their possible entanglement with these makes sometimes the diagnosis complex. The average diagnosis delay of 7.2 years reflect particularly the diagnostic difficulties 5.
Epidemiology of Non-epileptic Seizures
The prevalence of PNES in the general population ranges from 2 to 33 cases per 100.000 persons 6. However data from epilepsy centers estimate a much higher incidence rate. In 25–30% of the patients referred to tertiary epilepsy centers for refractory epilepsy a diagnosis of PNES is obtained 2. Women comprise between 75 and 85 percent of PNES cases 6. In the pediatric population, a 2:1 female:male ratio appears to exist--under the age of ten, the ratio is probably more of a 1:1 1.
Importantly, the NES population is quite heterogeneous, and very importantly, the economic impact of the disorder is likely to be very costly to society. Many of these patients have repeated visits to emergency rooms or they are inappropriately treated with antiepileptic medications. Until definitive EEG monitoring in a multidisciplinary team approach setting transpires, effectively determining 1.
Diagnosis of NES
The PNES take most of the time the appearance of tonic-clonic seizures, blind eyes and resistance in eyes opening, symmetric movements of limbs, antero- and retropulsion movements of pelvis, head movements from one side to the other, vocalisations, missing of post-critical phase 7. Certain clinical signs of the seizures were reported as suggestive of PNES: long duration, fluctuations in clinical signs which attenuate then reappear during the same seizure, asynchronous character of the movements when they are bilateral, flexion and extension movements of pelvis, denial movements of the head, eye closure, critical tears, taking of posture in opisthotonos 3.
The diagnosis of NES is a diagnosis of elimination which requires to have excluded a somatic, epileptic or psychiatric origin. No clinical criterion is enough discriminating to differentiate epilepsy and NES 3. Although diagnosis can be difficult, the differential diagnosis between NES and epilepsy has improved in the last 30 years, especially since the introduction of simultaneous video-EEG monitoring. Diagnosing NES is important because of the potential iatrogenic hazards such as potentially serious side effects of antiepileptic drugs and failure to recognize pseudo status epilepticus with a potential hazard of intubation.
A working definition, based on the aforementioned elements could be: a PNES is an observable abrupt paroxysmal change in behaviour or consciousness, that resembles an epileptic seizure, but that is not accompanied by the electrophysiological changes that accompany an epileptic seizure or clinical evidence for epilepsy, for which no other evidence is found for other somatic causes for the seizures, whereas there is positive evidence or a strong suspicion for psychogenic factors that may have caused the seizure 2.
The diagnosis and instituting an appropriate course of therapy is, or course, problematic 1. In the current day practice, video-electroencephalogram (v-EEG) is the gold standard in differentiating PNES from epilepsy. However, v-EEG is expensive and time-consuming. Routine inter-ictal EEG findings are generally not considered effective enough to establish an accurate diagnosis of PNES 6.
The coincidence of PNES and epilepsy is a further confounding variable for definitive diagnosis and treatment. 30% of patients admitted to tertiary care epilepsy units have co-incidence disorders. Ictal characteristics of PNES have been studied and there are some bedside parameters that can be of use to assist the clinician in determining whether an event is likely to be non-epileptic or epileptic. For tonic-clonic resembling events, a high degree of confidence can be gained by observing out-of-phase upper extremity and lower extremity movements or vocalization at the start of the event, as opposed to 20-second into the event, when a true tonic-clonic seizure makes the tonic-clonic transformation. Ictal duration can also be of utility for assessing tonic-clonic resembling-events; a tonic-clonic seizure generally lasts 70 seconds, plus or minus 20- seconds. Any tonic-clonic resembling-event going beyond this point should raise the suspicion of possible non-epileptic seizures, though obvious care needs to be taken that a true status epilepticus scenario is not transpiring.
The significant number of patients (30% on average) having mixed epileptic and non-epileptic seizure disorders, reduction of medication and further recording to exclude an underlying epileptic diathesis is important. In addition, for those unusual events that do not demonstrate surface EEG correlates predominantly consisting of electro-decremental epileptiform fast ictal patterns, repeated recordings of the ictal event to tease out any stereotypic is critical. Epileptic seizures have a clear threat of stereotypic, whereas the non-epileptic events are much more likely to have significant variation between them 1.
Treatment of Non-epileptic Seizures
A decision can then be made to either discontinue antiepileptic drugs for pure non-epileptic seizures or to continue only one antiepileptic drug because of co-existent epilepsy.
Treatment for NES takes time 1. The prognosis of this pathology is reserved but of as much better than an adapted care is organized, namely the association of a psychotherapy and a psychotropic treatment 3. Aftercare needs must be arranged with an identified therapeutist who clearly understands the diagnosis; and a smooth transition must be organized. The patient must be given aegis. Patients and their families must be advised that non-epileptic events may continue for a time, but once a more effective and culturally acceptable coping strategy has been initiated, they will eventually disappear 1.
Conclusion
Non-epileptic seizures are common, though the actual prevalence is unknown. Patients comprise a heterogenous population. This disorder is very costly to society. The diagnosis of PNES is sometimes difficult and complex. The diagnosis standard gold is the video-EEG, but it is not always accessible or informative. The possible entanglement with epilepsy makes sometimes the diagnosis complex.
References
- 1.Gates J R. (2002) Non-epileptic Seizures: Classification Co-existence with Epilepsy: Diagnosis, Therapeutic Approaches and Consensus. , Epilepsy & Behavior 3, 28-33.
- 2.NMG Bodde, Brooks J L, Baker G A, PAJM Boon, JGM Hendriksen. (2009) Psychogenic non-epileptic seizures—Definition, aetiology, treatment and prognostic issues: A critical review. , Seizure 18, 543-53.
- 3.Rahmouni C. (2016) Crises Psychogènes Non Épileptiques (à propos de 32 cas). Thèse Med; Université Sidi Mohammed Ben Abdellah FES:N°269/16.
- 5.Hingray C, Cohn A, Jonas J, Mignot T, Vignal J P. (2014) Comment poser le diagnostic de CPNE? Une approche syndromique, un diagnostic positif. , Neurologies Novembre 17(172), 335-43.
