Abstract
Introduction
The extra dural hematoma is a blood collection between the cranial vault and the dura mater. It is a neurosurgical emergency whose statistical data are poorly known in the Republic of Benin.
Objective
The aims of this study are to assess epidemiology, therapeutic and outcome of traumatic extra dural hematomas for children admitted to the surgical department of CHUD-B/A from 2012 to 2017.
Methods
This was a cross-sectional, descriptive and retrospective study over a period from January 1st, 2012 to December 31st, 2017.
Results
One hundred and seventy-eight cases of children aged between 0-15 years were examined for brain traumatic injury. Twenty-seven 27 (15.2%) cases of extra dural hematomas were retained. The most represented age group was between 11-15 years with a frequency of 42.1%. The male sex was more represented (78.9%). Road traffic accidents were the main aetiology (57.9%). 52.6% had a mild head injury, 26.3% had a moderate head injury and 21.1% had a severe head injury. On brain scan the frequently observed location was temporo-parietal (31.6%). Acute anemia was observed in 16 children. Seventeen children were operated on. The operation involved evacuation of extra dural hematoma by cranial bone flap with suspension of the dura mater. There were no deaths.
Conclusion
The availability of brain CT makes the diagnosis of extra dural hematoma easier. Its management is neurosurgical with a favourable post-operative evolution in all cases in this series.
Author Contributions
Academic Editor: Sasho Stoleski, Institute of Occupational Health of R. Macedonia, WHO CC and Ga2len CC, Macedonia.
Checked for plagiarism: Yes
Review by: Single-blind
Copyright © 2020 Quenum K, et al.
 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Competing interests
The authors have declared that no competing interests exist.
Citation:
Introduction
The extra dural hematoma (EDH) is a accumulation of blood located between the inner table of the skull and the dura mater and predominantly consists of venous blood in infants 1, 2. The main cause remains road traffic accidents 1, 2, 3, 4, 17. In developing countries such as the Republic of Benin, the difficulty of access to CT scans delays the diagnosis of EDH in children. The clinical nonspecific symptoms of this disease does not show its severity, and it is only when the neurological state deteriorates or when a brain CT scan is performed that the diagnosis is made 5, 14, 19. It is in order to highlight the realities of the management of extra dural hematomas in children in Benin, in particular at the University Hospital and Departmental Center of Parakou, that we initiated this study. It aims to study the epidemiological and therapeutic aspects of extra dural hematomas in children with traumatic brain injuries admitted to the neurosurgical department of University Hospital Center from 2012 to 2017 and to evaluate the beneficial behaviours for a favourable evolution.
Patients and Methods
This was a retrospective and cross-sectional study, performed from January 2012 to December 2017 in the neurosurgery unit of the Parakou University Hospital. All records of traumatic brain injuries concerning patients aged from 1 to 15 years were recorded. Cases of extra dural hematoma were retained. On their cerebral scanner, they had hyperdense lesions in a biconvex lens, located between the cranial vault and the dura mater.
The variables studied were socio-demographic variables (age, sex, level of education of the child, circumstances of occurrence of the accident, time of admission, medical history), data from the physical examination (sign of vital distress, neurological examination). At the end of the general examination, the head trauma patient was classified according to the MASTERS criteria; the paraclinical aspects used were: brain scan without injection of contrast agent and its results, Blood Formula Count (CBC), blood ionogram, therapeutic decision and finally the immediate postoperative follow-up (over a period of seven days).
Results
During the study period, 820 cases of brain injury were recorded in the department. These head injuries involved 178 children (21.7%), of whom 27 (15.2%) were diagnosed with an extra-dural hematoma. Out of the 27 cases of extradural hematoma, 19 cases (70.4%) satisfy our inclusion criteria. The annual distribution of pediatric EHD cases was reported in Table 1.
Table 1. Annual distribution of extradural hematoma cases in children| Brain injury in Child (n) | EHD in Child n(%) | |
| 2012 | 36 | 01 (02.8) |
| 2013 | 44 | 03 (06.8) |
| 2014 | 28 | 05 (17.9) |
| 2015 | 23 | 06 (26.1) |
| 2016 | 16 | 05 (31.3) |
| 2017 | 31 | 07 (22.6) |
| Total | 178 | 27 (15.2) |
The distribution by gender gives us the following distribution: Male children were more victims with 15 boys (78.9%) for every 04 girls (21.1%). The sex ratio of boys to girls was 3.7. As for the distribution by age group, the most represented was 11-15 with a frequency of 42.1%. The cumulative number of children aged 0-11 years was 57.9%. The mean age was 8±1.4 years with extremes of 1-15 years. Among these children, none had a pathological past history. Road traffic accidents accounted for 57.9% of cases (n=11).
The distribution of aetiologies of extra dural hematomas in children was reported in Table 2.
Table 2. Distribution of children admitted to HED, between 2012 and 2017, by aetiology| Number | Frequency (%) | |
| AVP | 11 | 57.9 |
| Games | 5 | 26.03 |
| Fall | 2 | 10.5 |
| PSE Accidents* | 1 | 5.3 |
| Total | 19 | 100 |
Out of the eleven patient’s victims by road accidents, two were pedestrians and the remaining nine were either towed or bicycles. Eight were without helmets and six cases were in the age range of] 10-15] years old. The gender distribution of children involved in a traffic accident showed that there were 10 boys for every 01 girl. Five children were admitted to the emergency room within the first 06 hours after the trauma and six were admitted between the 6th and 24th hours. The objective clinical signs are shown in Table 3.
Table 3. Distribution of EHD cases by functional and physical signs| Clinical feature | Number | Frequency (%) |
| Headache | 10 | 52.6 |
| Initial loss of consciousness | 9 | 47.4 |
| Irritability/agitation | 8 | 42.1 |
| Vomiting | 5 | 26.3 |
| Sleepiness | 4 | 21 |
| Constant crying | 3 | 15.8 |
| Loss of secondary consciousness | 2 | 10.5 |
| Distribution of objectified physical signs | ||
| Scalp wounds | 12 | 63.7 |
| Scalp deformation | 11 | 57.9 |
| Pupillary change | 4 | 21.1 |
| Hemiparesis | 4 | 21.1 |
| Epistaxis | 2 | 10.5 |
| Otorrhagia | 1 | 5.3 |
| Peri-orbital ecchymosis | 1 | 5.3 |
| Respiratory status | ||
| Stable | 17 | 89.5 |
| Unstable | 2 | 10.5 |
| Hemodynamic status | ||
| Stable | 19 | 100 |
| Unstable | 0 | 0 |
| Distribution of associated extracranial lesions | ||
| Facial trauma | 5 | 26.31 |
| Leg trauma | 4 | 21.05 |
| Pelvic trauma | 1 | 5.26 |
In this series, there were 21.0% severe head injury (n=04), 26.3% moderate head injury and 52.6% mild head injury.
Non-injection brain CT scan revealed eleven cases (57.9%) of left hemispheric extra dural hematoma. The most frequent observed location was temporo parietal with 06 cases (31.6%). The different locations were summarized in Table 4.
Table 4. Distribution of EHD cases by location and associated lesions| location | Number | Frequency (%) |
| Temporo-parietal | 6 | 31.6 |
| Frontal | 3 | 15.8 |
| Temporal | 3 | 15.8 |
| Fronto-parietal | 3 | 10.5 |
| Parietal | 2 | 10.5 |
| Parieto-occipital | 2 | 10.5 |
| Total | 19 | 100 |
| Objected associated injuries | ||
|---|---|---|
| Single fracture | 10 | 52.6 |
| Contusion | 5 | 26.3 |
| Mass effect | 5 | 26.3 |
| Skull depressed fracture | 3 | 15.8 |
From the point of view of care, two (n=2) (10.52%) children received medical treatment compared to 17 (89.48%) children who received medical-surgical treatment. Neurosurgical treatment consisted of evacuation of the extra dural hematoma. This involved making a skin incision, trepanation (Figure 3 a), a preserved cranial bone flap, evacuation of the extra-dural haematoma (Figure 3 b), haemostasis either of the bone using bone wax or venous or arterial haemostasis by bipolar coagulation as appropriate, suspension of the dura mater (Figure 3 c), replacement of the bone flap (Figure 3 d) and finally suturing of the scalp in two planes. Figure 1, Figure 2, Figure 3.
Figure 1.Image of a brain CT scan without contrast, in a parenchymal window, axial view showing a right parietal extra dural hematoma associated with diffuse cerebral oedema, and subfalcorial brain schift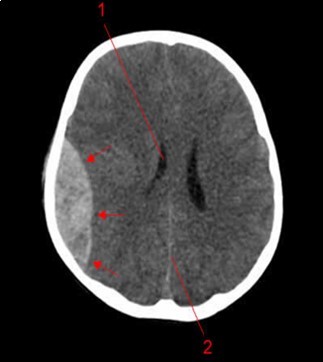
Figure 2.Image of a brain CT scan without contrast agent injection in a bone window, axial section showing a right parieto-occipital fracture (a), coronal section showing a left parietal skull depressed fracture (b)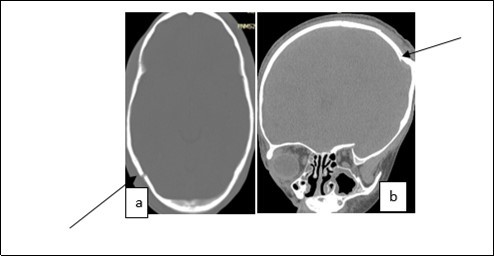
Figure 3.Operating times for an extra dural hematoma: a) making a cranial bone flap with three drill holes (the black arrows); b) extra dural hematoma after craniotomy (by the blue arrows); c) image showing the dura mater then suspension of the dura mater (the green arrows) and d) image after handing over the bone flap.
With regard to the distribution of the children according to the haemoglobin level, we were able to subdivide into four groups:
Group 1: haemoglobin level less than 8g/dl in 6 cases (31.57%)
Group 2: haemoglobin level between 8 and 10g/dl in 7 cases (36.84%)
Group 3: haemoglobin level between 10 and 12g/dl in 3 cases (15.79%)
Group 4: haemoglobin level greater than 12g/dl in 3 cases (15.79%)
With respect to the blood ionogram: 16 children (84.21%) had a normal ionogram and 3 (15.79%) had hyponatremia, one of which was associated with hyperkalemia.
In the group of those who underwent surgery, 15 (n=15, 78.9%) benefited from blood transfusion for the following reasons: pre-existing anemia prior to surgical treatment and intra operative bleeding which was estimated by the major neurosurgical team. Six (n=6) children had received a 350 ml bag of completed blood cells prior to surgery. Transfusion was performed either intra operatively or immediately postoperatively, depending on the availability of blood products. Three children (n=3 or 15.8%) benefited from functional rehabilitation due to the presence of hemi-corporeal deficit. The evolution is very satisfactory and without complications in 16 cases. Only one case of delayed awakening was noted and required a cerebral CT scan without injection of contrast agent, which did not show any particularity, especially no blood recollection or areas of contusion. It was a situation of hypothermia. Two cases have temporally neurologic disorder. This is a case who had received conservative treatment and who retained dysarthria and intermittent headaches. There were no deaths in this series. The mortality rate was 0 %. The average length of hospitalization is 7±2 days with average of 05 days to 27 days.
Discussion
The prevalence of EHD varies according to authors and countries. This difference reflects the variations that may exist within the samples studied. Indeed, the prevalence of 15.2% in the present study is slightly lower, compared to the results obtained by Hodé et al 11 in Cotonou, in southern Benin (20%) and Gaye et al 1 in Senegal. Because of the higher density, traffic accidents involving two-person vehicles are more frequent, hence the increase in frequency. Hassen et al 10 in 2012 in Tunis and Enicker et al21 in South Africa reported lower prevalences: 10.4% and 08% respectively. The modernization of transport systems, in this case school buses, could be the main reason 2, 3, 4. The main circumstance for the occurrence of EHD in children in this study was a road traffic accident. The same finding was made by Emejulu in Nigeria 20. The school children group was the most concerned in the present study, the hours of return from classes constitute situations of vulnerability of children in front of the state of degradation of our traffic roads, the speeding of motorcyclists and the non-respect of signals at the approach of schools. Falling from trees and game accidents are the main causes of head injury in countries that have passed this milestone. Mild brain injury was commonest with a frequency of 52.6%, a finding made by several authors. Far from being a good factor, this condition worsens the prognosis of the child. Indeed, after trauma involving adult and child, the children appears to be unharmed while adults are seriously injured, diverting attention to the latter. It is the installation of secondary neurological disorder that call for attention, and sometimes it is already too late 8, 9, 12, 13, 14. Hence the interest of performing a CT scans in any child victim of head trauma regardless of his clinical condition. However, it should be noted that the frequency of mild head and brain injuries is not as high in the general population as in children 15, 16, 17, 22. This was found by Khattak et al 32 and Khaled et al 23 in a study of patients with head injuries where mild injury and accounted for 49.5% 24, 26, 27.
Anemia is a cause of death in children with EHD. Indeed the hematoma is easily formed, facilitated by the structure of the child's head. In addition, the circulating blood volume of the child being low, a situation simulating an internal haemorrhage occurs very early. It is to remedy this situation that 15 of the 17 children operated received at least one complet blood transfusion (350 ml). Ijaz et al32 reported 100% blood transfusion. Tascu et al29 found acute post-operative anemia in 36% of children operated for EHD required an emergency transfusion. So transfusion is the key element in the management of extra-dural hematomas in children. This transfusion improves the pre-, per- and post-operative resuscitation conditions of these children. And all this contributes to a good management of children operated for EHD.
The postoperative outcome was favourable in 100% of cases. This result is the same to Ijazet and al32 findings, who transfused peri operatively as in our series. On the other hand, in the literature the mortality rate for extra-dural hematomas in the general population is 14% in Nigeria according to Mezue et al 18, 18% in Madagascar according to Rokotondraide et al19, 13.4% according to Kabré et al5, in Burkina Faso and Togo 04.8% in the adult population. According to Asif et al28, the rate of 04% of the paediatric population died after surgery, but the cause of death could not be identified. Shahenn et al33found the same frequency but in Roka serie this mortality rate reach 09%34.
We concluded that blood transfusion as part of the management of EDH would be one of the items for a favourable outcome in children. Thus, the preservation of blood mass in peri operative care it is a determining element for a good anaesthesia and resuscitation of these children, this associated with a good neurosurgical technique of haematoma evacuation.
Conclusion
Extra dural hematomas are relatively common in children. The most incriminated aetiology in Benin is road traffic accident. The high rate of mild head injury trauma with no clinical findings in children contrasts with the severity of the condition. This delays extra dural haematoma diagnosis made after brain CT scan. Efficient management of blood loss is one of the keys to successful management associated with good neurosurgical practices.
References
- 1.Gaye M, Diatta B, Ndoye N, Ba M C, Thiam A B et al. (2010) Prise en charge de l’hématome extradural à Dakar. à propos de 40 cas. , African Journal Neurological sciences 29(1), 47-56.
- 2.Fatigba O H, KM Savi de Tove, Allode S A, Babio R, Padonou J. (2011) Prise en charge neurochirurgicale des traumatismes crâniens à Parakou, Benin : apport de la radiographie standard. Mali Médical.; tome XXVI. (2) :. 4-7.
- 3.Djientcheu V P, Bisso A N, Njamnshi A K, Ongolo-Zogo P, Hell-Medjo E et al. (2005) Les hématomes extra-duraux post traumatiques : prise en charge médico-chirurgicale. African Journal Neurological sciences. 24(2), 33-9.
- 4.Thiam A B, Mudekereza P S, Ndoye N, Kachungunu M C, Ba M C et al. (2013) Hématome extra-dural: étude épidémiologique à propos de 35 cas. , Journal 18, 13-20.
- 5.Kabré A, Zabsonré S, Haro H, Sanou A. (2013) Les hématomes extraduraux post-traumatiques : aspect cliniques et pronostiques : à propos de 164 cas. , Journal 18, 21-6.
- 6.Alliez J R, Hilal N. (2005) L’hématome extra-dural. African Journal Neurological sciences. 24(2), 62-9.
- 7.Rasolonjatovo C, Tsiaremby M G, RAkotovao K T, Ratovondrainy W, Rabarijaona M et al. (2015) L’hématome extradural opéré au. , CHU Joseph Ravoahangy, Andrianavalona Antananarivo, Madagascar. African Journal of Neurological Sciences.; 33(2), 26-31.
- 8.Bissonnette B, Vinchon M. (2002) Les différentes lésions cérébrales traumatiques du nourrisson et du petit enfant : mécanismes et clinique. Ann Fr AnesthReanim. 21, 133-40.
- 9.Fatigba H O, MK Savi de Tove, Tchaou B A, Mensah E, Allode A S et al. (2013) Surgical management of head trauma: Problems, results, and perspectives at the departmental teaching hospital of Borgou. , Benin.World Neurosurg.80(3-4): 246-250.
- 10.Hassen A F, Zayani M C, Friaa M, Trifa M, Ben Khalifa S. (2012) Épidémiologie du Traumatisme Crânien à l’Hôpital d’Enfants de Tunis au cours de l’année 2007. Tunisie Médicale. 90(1) : 25-30.
- 11.Hode L, DHO Sogbo, Hounnou M G, Houessou G F, AKA Voyeme et al. (2015) prise en charge des traumatismes crânio-encéphaliques chez les enfants à Cotonou. , African Journal of Neurological 33(2), 55-65.
- 12.Figaji A A. (2017) Anatomical and Physiological Differences between Children and Adults Relevant to Traumatic Brain Injury and the Implications for Clinical Assessment and Care. 8, 1-15.
- 13.Trabold F, Meyer P, Orliaguet G. (2001) Les traumatismes crâniens du nourrisson et du petit enfant : prise en charge initiale. Ann Fr réanim. 20, 64-70.
- 14.Mh Touré, Diop A D, Ly M, Kikwaka J, Kasereka D H et al. (2017) Traumatisme cranio- encéphalique (TCE) de l’enfant aspects tomodensitométriques à propos de 298 cas au CHNU FANN (Dakar). , Journal africain d’Imagerie Médicale 9(4), 140-7.
- 15.Bouchakour M, Bellebna B, Dermeche A, Kahli K. (2005) Traitement non Chirurgical de l’hématome extra dural : étude prospective de 58 cas. , Journal de neurochirurgie.; 2, 14-8.
- 16.Dubey A, Pillai S V, SVR Kolluri. (2004) . Does Volume of Extradural Hematoma Influence Management Strategy and Outcome? NeurolIndia 52(4), 443-5.
- 17.Fatigba O H, Adédémy J D, Mensah E D, KM Savi de Tové, YarouYérima S et al. (2011) Les traumatismes crânio-encéphaliques de l’enfant dans un centre hospitalier au Nord-Est du Bénin. , Rev. Cames-Série A, Sciences et 12(2), 176-80.
- 18.Mezue W C, Ndubuisi C A, Chikani M C, Achebe D S.Ohaegbulam SC. Traumatic Extradural Hematoma in Enugu. , Nigeria, Nigerian Journal of Surgery 18(2), 80-4.
- 19.Rakotondraibe W F, Rakotoniaina F, Bemora S, Rajaonera A T, Ratovondrainy W et al.Approches diagnostiques et prise en charge des hématomes extraduraux opérés dans le service de Neurochirurgie du CHU-JRA. , Antananarivo. Rev. Anesth.-Réanim. Med. Urg. Toxicol 8(2), 8-12.
- 20.JKC Emejulu, Uche E O, Nwankwo E U. (2014) The Challenges of Managing Acute Extradural Hematoma in a Nigerian Neurosurgical Center—Still a Long Way to Go. World Neurosurg.82(6):. 969-73.
- 21.Enicker B, Louw H, Madiba T. (2016) Acute extradural haematomas in children A 12-year experience from a single neurosurgery unit. , S Afr J 54(4), 28-33.
- 22.Jung S, Kim D. (2012) Our Experience with Surgically Treated Epidural Hematomas in Children. , J Korean Neurosurg Soc 51, 215-8.
- 23.SMN KhaledChowdhury, TarIkul Islam KM, Mahmood E, HossaIn S S. (2012) Extradural Haematoma in Children Surgical Experiences and Prospective Extradural Haematoma in Children Surgical Experiences and Prospective Analysis of 170 Cases. , Turkish Neurosurgery 22(1), 39-43.
- 24.JLV Araujo, UDP Aguiar, Todeschini A B, Saade N, JCE Veiga. (2012) Epidemiological analysis of 210 cases of surgically treated traumatic extradural hematoma. 39(4), 268-71.
- 25.Khaled S, Hanif A, KMT Islam, Mahmood E, Hossain S S. (2010) Extradural haematoma in children surgical experiences and prospective analysis of 138 cases.Journal of Paediatric Surgeons of Bangladesh. 1(1), 19-24.
- 26.Rocchi G, Caroli E, Raco A, Salvati M, Delfini R. (2010) Traumatic Epidural Hematoma in Children. , Journal of Child Neurology 20(7), 569-71.
- 27.Aurangzeb A, EAK Afridi, Ali Khan S, Muhammad G, Ihsan A et al. (2015) Frequency of extradural haematoma in patients with linear skull fracture. J Ayub Med Col Abbottabad. 27(2), 314-7.
- 28.Asif M. (2017) A Life Threatening Problem in Children Extra Dural Hematomas; Analysis of 65 Cases. , Pak J. of Neurol. Surg 21(4), 205-209.
- 29.Tascu A, Pascal C, Iencean S M, Gorgan M R. (2014) Aggressive or conservative management in extradural hematomas in children – a challenging neurosurgical choice. Romanian Neurosurgery. 21(4), 385-94.
- 30.Teichert J H, Rosales P R, Lopes P B, Enéas L V, T Sica da Rocha. (2012) . Extradural Hematoma in Children Case Series of 33 Patients. PediatrNeurosurg; 48, 216-220.
- 31.Khattak A U, Iftikhar-ul-haq M, Azam F. (2012) Frequency of Extra-dural Hematoma in Patients with Head Injury. , Pak J. of Neurol. Surg 16(2), 83-6.
- 32.Ijaz L, Nadeem M M. (2016) Minimal Invasive Burr – Hole Management of Traumatic EDH. , Pak J. of Neurol. Surg 20(3), 149-53.
