Abstract
Objective:
The objective of this study was to evaluate the efficacy of patent haemostasis in avoiding radial artery occlusion after transradial catheterization.
Background:
Radial artery occlusion is an infrequent but discouraging complication of transradial access. It is related to factors such as sheath to artery ratio and is less common in patients receiving heparin. Despite being clinically silent in most cases, it limits future transradial access.
Patients and Methods:
130 patients undergoing transradial catheterization were prospectively enrolled in the study. 65 patients were randomized to group I, and underwent conventional pressure application for haemostasis. 65 were randomized to group II and underwent pressure application confirming radial artery patency using Barbeau’s test. Radial artery patency was studied at 24 hr and 30 days using Barbeau’s test.
Results:
There was Statistically significant difference found in rate of radial artery occlusion of both the groups at 24 hours (24.61% vs. 4.61% ,X2(1)=4.44, P<0.05) and at 30 days(20% vs. 3%,X2(1) =4.03, P < 0.05). Patients with
Higher age and smaller radial artery diameter were at significantly higher risk of radial artery occlusion. No other procedural variables were found to be associated with radial artery occlusion.
Conclusion:
Patent haemostasis is highly effective in reducing radial artery occlusion after radial access and guided compression should be performed to maintain radial artery patency at the time of haemostasis, to prevent future radial artery occlusion.
Author Contributions
Academic Editor: Sanjiv Sharma, Chairman, Dept of Medicine Director, Research and Education Chairman, Health Education and CME Committee Interventional Cardiologist
Checked for plagiarism: Yes
Review by: Single-blind
Copyright © 2016 Arpan P. Desai, et al.
 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Competing interests
The authors have declared that no competing interests exist.
Citation:
Introduction
Since the first successful diagnostic transradial coronary catheterization by Campeau in 1989 and the first transradial percutaneous coronary intervention (PCI) by Kiemeneij in 1993 , the radial artery has been increasingly used as an access site for coronary procedures, because of lower rate of access site complications, shorter hospital stay, improved patient comfort, and safe haemostasis compared with transfemoral access. Radial artery occlusion is one of the few post procedural complications of Trans Radial Angiography (TRA) 1. Though it does not harm the patient but subsequesent same site TRA is not possible. Repeated cannulations predispose to occlusion 2. There are many other factors associated with radial artery occlusion (RAO) in previous observational study mainly the size of the introducer sheath 3, 4, the ratio of the arterial diameter to the sheath 5, and heparinization 6. Physicians try to prevent and treat radial artery occlusion by antithrombotic but still around 7-12% patients developed plethysmography documented RAO which is higher than the clinically documented rate. This difference between clinically documented rate and plethysmography documented rate is due to the fact that the occluded radial artery distal stump may have up to 70% of mean arterial pressure because of macro collateral circulation from the palmer arches 7, leading to a palpable pulse. Hence palpation of radial pulse does not imply radial artery patency. Barbeau’s test uses Plethysmographic method to evaluate radial artery patency. It has extremely high correlation with duplex Doppler ultrasonography and hence is very accurate. For prevention of RAO there are many improvements done in the hardware like use of Hydrophilic introducers and lower profile equipment. But the most important measure to prevent RAO lies in its pathophysiology. It has been shown that at the time of haemostasis if the flow at the site of puncture is interrupted it will lead to formation of thrombotic plug. So maintaining flow at the puncture site at the time of haemostasis known as a patent haemostasis may decrease RAO 8, 9, 10. Hence a randomized control study was conducted with the following objective.
Hypothesis
Patency documented haemostasis causes less radial artery occlusion than the traditional haemostasis in Trans radial angiography cases.
Objectives
Primary objective is to assess the difference in number of cases who developed radial artery occlusion among the patency documented haemostasis group and traditional haemostasis group after Trans radial catheterization at 24 hours and 30 days.
Methods
Patient Population
This hospital based randomized interventional study was conducted at department of Cardiology, SMS hospital, Jaipur.
Inclusion criteria; consecutive patients presenting for elective outpatient diagnostic cardiac catheterization were enrolled in the study.
Exclusion criteria; Patients on Coumadin therapy, thrombocytopenia (because both the groups are at higher risk for bleeding complications), patients presented with acute coronary syndrome, patients planned for PTCA (because in both groups amount of anticoagulant varies and anticoagulant is one of the factor which can affect the outcome), abnormal Barbeau’s test (at risk for ischemic complication of hand) and those for an a-priori transfemoral approach.
Sample Size Calculation:
The previous year observation in our setup revealed 25% cases (61 out of 240 cases) of trans radial angiography with traditional haemostasis method developed Radial artery occlusion, we expect 4 times reduction (i.e. 6%) in occlusion rate with patency documented haemostasis method (in PROPHET study RAO rate were 7% vs. 1.8% in respective groups) (8), to verify this hypothesis at 95% confidence interval and 80% power, the required sample size would be 62 in each group. This was rounded up to 65 for our study. 130 eligible trans radial angiography cases who met the inclusion criteria were considered for study on first cum first basis. They were randomly allocated to traditional and Patency Documented Haemostasis method using ‘Envelop method’. Randomization and intervention were done by the physician other than investigator. Patients were unaware about the type of haemostasis method to which they were randomized. The first case was enrolled on 2nd April 2012, last case was enrolled on 26th February 2013, first follow up was taken on 3rd April 2012 and last follow up was taken on 28th March 2013. A Barbeau’s test was performed at baseline for presence of dual circulation and patency of palmer arch. All enrolled patients had patent dual circulation and palmer arch. Twenty-four-hour and 30-day follow-up was completed in both groups. Analysis of the outcome of all the participants was done as per their original assigned group. The techniques for traditional and ‘‘patent haemostasis’’ are described later. All patients provided informed consent. All the patients were available for complete planned follow up (30 days).
Transradial Catheterization Procedure
After sterile preparation and injection of 2% lidocaine at the puncture site, a 20-gauge Teflon catheter was used to enter the radial artery using Seldinger technique, with through-and-through puncture. The stylet was removed and the system was gradually withdrawn. Upon appearance of pulsatile flow Terumo 0.02100 guidewire was placed in the hub of the cannula, the guide wire was advanced into the radial artery lumen. The radio focus glide sheath was then advanced over the guidewire into the radial artery. A ‘‘radial cocktail’’ consisting of 200 mcg of nitroglycerin, 2.5 mg of Diltiazem, and 2500 units of unfractionated heparin was administered intraarterially. The procedure was completed using diagnostic coronary catheters.
Conventional Haemostasis Procedure
All introducer sheaths were immediately removed. The sheath was pulled out 4–5 cm and a HemobandTM plastic band was placed around the wrist. The band was tightened after which the sheath was pulled out. The band was left in place till haemostasis, then slowly removed, and a light dressing was applied to the site. After removal of hemoband, Barbeau’s test was performed to assess radial artery patency status at 24 hours & 30 days . Patients in this group who had interruption of radial artery flow after haemostatic compression were recorded to have ‘‘occlusive hold.’’ The operators were blinded to these data at that time and hence no alterations were made.
‘‘Patent Haemostasis’’ Procedure
The sheath was pulled out 4, 5 cm and a plastic band ‘‘hemoband’’ was placed around the forearm at the site of entry. A pulse oximeter sensor was placed over the index finger, the hemoband was tightened, and the sheath was removed. Ipsilateral ulnar artery was occluded and the hemoband was loosened till plethysmographic signal returned (confirming radial artery patency) or bleeding occurred. If bleeding occurred at the pressure required to maintain patency, manual compression was used.
Assessment of Radial Artery Patency
Radial artery patency was assessed using Barbeau’s test. A pulse oximeter sensor was placed over the index finger. A plethysmographic signal was observed and both radial and ulnar arteries were compressed to observe loss of plethysmographic signal. Then the radial artery was released and the return of plethysmographic signal was observed. Return of signal confirmed radial artery flow and hence patency. Absence of return of signal was interpreted as radial artery occlusion. The ulnar artery was then released to observe return of signal, confirming proper functioning of the equipment. This test was performed at 24 hr. and 1 month after the procedure.
Statistical analysis:
Quantitative data were summarized in the form of Mean & SD. The difference in the Means were analyzed using student’s ‘t’ test. Qualitative data were summarized in the form of proportions. Difference in the proportions was analyzed using chi square test. Multivariate analysis using logistic regression was done to predict radial artery occlusion at 24 hours & 30 days. Wald statistics, Negelkerke R2, Odds ratio were computed. The variables used for analysis were sex, age, weight, height, s. creatinine, DM, HTN, smoker, sheath size, radial artery diameter, and method of haemostasis. The level of siassagnificance was kept 95% for all statistical analysis. SPSS version 16 was used for statistical analysis.
Results
Clinical Data
Baseline clinical data for group I and group II are presented in Table 1. Both the groups were comparable for the distribution of age, gender, height, weight, creatinine, sheath size as well as prevalence of diabetes mellitus, hypertension, smoker and radial artery diameter (p>0.05).
Table 1. Demographic and Procedural Data| VARIABLE | Group I (traditional hold) ( NO=65) | Group II (patent hold) ( NO=65) | P Value |
| Age (years) | 54.86 ±10.98 | 56.32 ± 10.95 | >0.05 |
| Height (cm) | 162.89 ± 7.54 | 158.30 ± 7.54 | >0.05 |
| Weight (kg) | 60.03 ± 8.47 | 61.55 ± 8.44 | >0.05 |
| Creatinine (mg/dl) | 0.998 ± 0.211 | 1.012 ± 0.212 | >0.05 |
| Cigarette smoking | 32 | 44 | >0.05 |
| Diabetes Mellitus | 16 | 13 | >0.05 |
| Gender (females ) | 3 | 6 | >0.05 |
| Hypertension | 40 | 40 | >0.05 |
| 5 F SHEATH | 16 | 17 | >0.05 |
| Radial artery diameter (mm) (no = 35 in each) | 2.39 ± 0.28 | 2.51 ± 0.28 | >0.05 |
Radial Artery Occlusion Data
The difference in the RAO rate at 24 hours and at 30 days of both the groups was analysed using chi-square test. 16(24.61%) patients in group I developed plethysmographic evidence of radial artery occlusion at 24-hr follow-up, compared with 3 (4.61%) in group II. This was statistically significant. (24.61% vs. 4.61%,X2(1)=4.44,P<0.05). 13(20%) patients in group I developed plethysmographic evidence of radial artery occlusion at 30 days follow-up, compared with 2 (3%) in group II. This was statistically significant (20% vs. 3%, X2(1) =4.03, P < 0.05). These results are shown in Figure 1.
Figure 1.Patent haemostasis leads to a significant decrease in the incidence of radial artery occlusion at 24-hr and 30-day follow-up.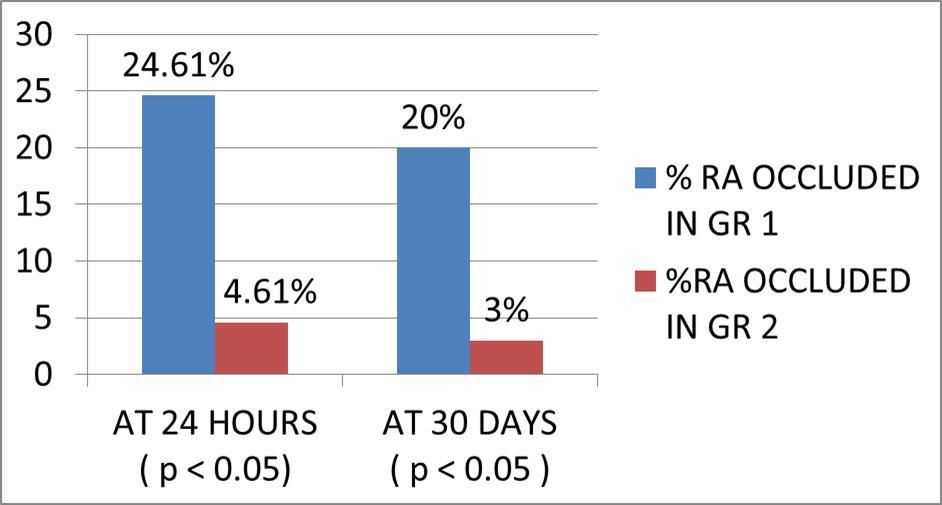
A separate analysis was performed on patients by dividing the population into those who developed radial artery occlusion at 24 hours versus those who did not. This was done to evaluate associations between commonly available demographic and procedural variables and radial artery occlusion. Bivariate analysis was performed on all variables for the entire population. There was statistically significant difference found in the age of the patients whose radial artery were occluded vs. not occluded (66.05 ± 11.11years vs. 55.68 ± 10.94years,’t’statistics(128)=3.8292,P<0.01).similarly there was statistically significant difference found in the radial artery diameter of the patients whose radial artery were occluded vs not occluded(2.05 ± 0.232mm vs. 2.49 ± 0.278mm t(68)=4.7413,P< 0.001).No statistically significant difference was found in the distribution of diabetes mellitus, hypertension, gender, smoking, height, weight, sheath size or creatinine. These findings are shown in Table 2.
Table 2. Results of Bivariate Comparison of Patients With or Without Radial Artery Occlusion at 24 hours| VARIABLE | Occluded Radial artery Group (no=19) | Patent Radial artery Group(no=111) | P Value |
| Age (years) | 66.05 ± 11.11 | 55.68 ± 10.94 | <0.01 |
| Height (cm) | 159.9 ± 7.50 | 160.4 ± 8.44 | >0.05 |
| Weight (kg) | 62.90 ± 8.34 | 63.15 ± 8.44 | >0.05 |
| Creatinine (mg/dl) | 1.164 ± 0.211 | 1.020 ± 0.211 | >0.05 |
| Cigarette smoking | 14 | 62 | >0.05 |
| Diabetes | 2 | 27 | >0.05 |
| Gender (females ) | 2 | 7 | >0.05 |
| Hypertension | 12 | 68 | >0.05 |
| 5 F SHEATH | 3 | 30 | >0.05 |
| Radial artery diameter (mm) | 2.05 ± 0.232(n=10) | 2.49 ± 0.278(n=60) | <0.001 |
Predictors of Radial Artery Occlusion
A test of the full model in multiple logistic regression was statistically significant (for prediction at 24 hours and 30 days) (p<0.001). Negelkerke R2 of 0.419 at 24 hours prediction model and 0.415 at 30 days indicated moderate relationship between predictors and grouping. The overall success rate of prediction for this model is 87.7% at 24 hours & 90% at 30 days.
The Wald criterion demonstrated that age and type of method of haemostasis had significant effects. The odds ratio for age was 1.135 at 24 hours (P= 0.001) & 1.140 at 30 days (p=0.002). The odds ratio for type of method of haemostasis employed is 4.468 at 24 hours (P=0.021), & 5.421 at 30 days (p=0.027).
Haemostatic Efficacy
Bleeding complication was defined as blood loss from the access site leading to hemodynamic instability, transfusion, or death.
None of the patients developed a bleeding complication or any other complication.
Discussion
Trans radial approach is becoming the most preferred approach on both the patients and physician part for intervention because of several advantages over transfemoral approach like decrease in the bleeding complication, decrease in pseudo aneurysm or AV malformation, decrease in mortality 11, 12. In the present study the RAO rate was 4.6% in patency documented group against 24.6% in traditional group. This observation is consistent with the land mark PROPHET STUDY (8). The lower rate of RAO is explained by the fact that at the time of pressure haemostasis, flow at the puncture site was maintained in patency documented group which has prevented formation of the thrombotic plug. In current study RAO rate is very high in traditional group as compare to that in PROPHET study group both at 24 hours and at 30 days. This is because PROPHET study involved 3 different countries population (India, USA, PA) while in our study only Indian patients were involved. Western people have on an average higher body surface area as compared to Indians, hence they have larger radial artery diameter as compared to Indian. Apart from the variables used in PROPHET study, in present study we found that radial artery diameter is one of the important predictor of RAO.
Present study also observed that only age, method of haemostasis and the radial artery diameter are the predictors of RAO. And among them the method of haemostasis is the best predictor (The odds ratio for type of method of haemostasis employed is 4.468 at 24 hours (P=0.021), & 5.421 at 30 days (p=0.027).)
All those cases that did not develop RAO at 24 hours also did not develop occlusion at 30 days. It indicates that occlusion develops in early post operative period.
At 30 days, out of total 19 cases that had occluded radial artery at 24 hours, only 4 cases subsequently resumed patency in current study. It indicates that maintaining the patency at the time of the haemostasis is the most vital factor to prevent RAO. So for the prevention of RAO, screening of at risk patients should be done preprocedurely like advanced age and those who have smaller radial artery diameter. But once the procedure has been done the only variable which can prevent the RAO is the method of haemostasis. Not only this but also it is a very safe, most universally applicable method, not limited by any other systemic co morbidity, as none of the patients in our study developed any complication.
Limitations
The only limitation of this study is that the radial artery diameter was available in 70 patients, but still the difference in the radial artery diameter was statistically significant in between two groups (who developed RAO versus who did not developed RAO).
As most patients with coronary artery disease will need more than one catheter-based procedure in their lifetime, harmless strategies to prevent occlusion at the occasional expense of extra staff time appear to be worthwhile, to repeatedly enjoy the safety and comfort of TRA.
Conclusions
Patent haemostasis is successful in significantly lowering the incidence of radial artery occlusion after TRA, without compromising haemostatic efficacy.
Supplementary data
References
- 1.Stella P R, Kiemeneij F, Laarman G J, Odekerken D, Slagboom T et al.Incidence and outcome of radial artery occlusion following transradial artery coronary angioplasty. Cathet Cardiovasc Diagn 1997;40:. 156-158.
- 2.Sakai H, Ikeda S, Harada T, Yonashiro S, Ozumi K et al. (2004) Limitations of successive transradial approach in the same arm: The Japanese experience. , Catheter Cardiovasc Interv; 54, 204-208.
- 3.Dahm J B, Vogelgesang D, Hummel A, Staudt A, Volzke H et al. (2002) A randomized trial of 5 vs. 6 French transradial percutaneous coronary interventions. Catheter Cardiovasc Interv. 57, 172-176.
- 4.Wu S S, Galani R J, Bahro A, Moore J A, Burket M W et al. (2002) 8 French transradial coronary interventions: clinical outcome and late effects on the radial artery and hand function. , J Invasive Cardiol; 12, 605-609.
- 5.Saito S, Ikei H, Hosokawa G, Tanaka S.Influence of the ratio between radial artery inner diameter and sheath outer diameter on radial artery flow after transradial coronary intervention. Catheter Cardiovasc Interv 1999;46:. 173-178.
- 6.Lefevre T, Thebault B, Spaulding C, Funck F, Chaveau M et al. (1995) Radial artery patency after percutaneous left radial artery approach for coronary angiography. The role of heparin. , Eur Heart J; 16, 293.
- 7.Kerawala C J, Martin I C. (2003) Palmar arch backflow following radial forearm free flap harvest. , Br J Oral Maxillofac Surg ; 41, 157-160.
- 8. (2008) Prevention of Radial Artery Occlusion—Patent Hemostasis Evaluation Trial (PROPHET Study): Samir PancholyI. , John Coppola, Tejas Patel, and Marie Roke-Thomas.Catheterization and Cardiovascular Interventions 72, 335-340.
- 9.Pancholy S B. (2007) Transradial access in an occluded radial artery: New technique. , J Invasive Cardiol; 19, 541-544.
- 10.Sanmartin M, Gomez M, Ramon J R. (2007) Interruption of blood flow during compression and radial artery occlusion after transradial catheterization. , Catheter Cardiovasc Inter; 70, 185-189.
