Abstract
Many lay people along with some so called “key opinion leaders” have a common slogan “There's no answer for cancer”. Again, mistake delays proper treatment and make situation worse, more often. Compliance is crucial to obtain optimal health outcomes, such as cure or improvement in QoL. Patients may delay treatment or fail to seek care because of high out-of- pocket expenditures. Despite phenomenal development, conventional therapy falls short in cancer management. There are two major hurdles in anticancer drug development: dose-limiting toxic side effects that reduce either drug effectiveness or the QoL of patients and complicated drug development processes that are costly and time consuming. Cancer patients are increasingly seeking out alternative medicine and might be reluctant to disclose its use to their oncology treatment physicians. But there is limited available information on patterns of utilization and efficacy of alternative medicine for patients with cancer. As adjuvant therapy, many traditional medicines shown efficacy against brain, head and neck, skin, breast, liver, pancreas, kidney, bladder, prostate, colon and blood cancers. The literature reviews non-pharmacological interventions used against cancer, published trials, systematic reviews and meta-analyses.
Author Contributions
Academic Editor: Wei Wu, Nanjing Medical University, China
Checked for plagiarism: Yes
Review by: Single-blind
Copyright © 2019 Abdul Kader Mohiuddin
 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Competing interests
The authors have declared that no competing interests exist.
Citation:
Introduction
In 2019, 1.8 million new cancer cases and 0.6 cancer deaths are projected to occur in the USA 3. Globally, cancer responsible for at least 20% of all mortality 4, 18.1 million new cancer (9.5 million cases were in men and 8.6 million in women, according to AICR), 9.5 million death in 2018 5, 6, 5- year prevalence 43.8 million (a nearly 67% of total cancer patients) 7, 8, is predicted to rise by 61.4% to 27.5 million in 2040 9. Cancer is the second most common cause of death in the USA and rest of the world 10, 11. It is estimated that there will be 18 million new cases of cancer and 9.6 million cancer deaths in 2018 (GLOBOCAN 2018). Mortality rates in LMICs were 2-fold higher for cervical cancer and 40% higher for male lung and liver cancers during 2012-2016 3, with around 70% of deaths from cancer reported in LMICs 12, 13. Asia, Africa, and Latin America are home of 50% of cancer patients collectively; with more than half of global cancer-associated mortalities occurring in Asia alone 13. Lung cancer is the leading cause of cancer death (nearly 1 in 5 of all cancer death) 14, stomach cancer is the 3rd15 and pancreatic cancer is the 7th16 leading cause of cancer-related deaths worldwide. Prostate cancer is the second most frequent cancer diagnosis made in men and the fifth leading cause of cancer deaths for males 17. Asia and Europe are the home of more than 60% prostate cancer patients 18. Breast cancer is prevalent in 12% of women in the USA more than 2.5 million new cases of breast cancer were diagnosed in 2017 19. The rate for breast cancer declined by 35% in last 3 decades but number of deaths remain same 20. The 3 most prevalent cancers in 2019 are prostate, colorectal and skin melanoma among males, and breast, uterine corpus, and colorectal among females 21. Overall cancer death rates declined faster in blacks than whites in US, although rates for cancers of the breast, uterine corpus, and pancreas are increasing in black people 22. Also, black men have a 70% higher prostate cancer and a more than 2-fold higher mortality rate compared with white men 23. The cost of delivering cancer treatment is estimated to rise globally with a projected total spending of $458 billion by 2030 24. However, the financial burden stems from employment loss, cost of care even when patients don't require chemotherapy, out of pocket costs' opportunity costs of informal care time and can continue long after the death of the patient 25, 26. Studies say 46 billion in productivity lost in major emerging economies due to cancer 27 and economic costs of tobacco-related cancers exceed USD 200 billion each year 28. Also, cancer causes 2.6 times more likely to file for bankruptcy than the non-cancer people 29. Cancer trends in young adults, reflect recent changes in carcinogenic exposures, which could foreshadow the future overall disease burden 30. Cancer cachexia (anorexia, weight loss, loss of adipose tissue and skeletal muscle) is reported in 30%-80% cancer patients and causes 20% of all cancer deaths 31. Worldwide, some 60%-80% people depend on alternative medicines 32, 33, 34, which is also true for nearly 40% to 70% European 35, 36, 50% Italian, 40% Korean, 30% British 37 and up to 87% of Australian cancer patients 38. Use of unapproved/unlabeled/wrong herbal treatment is not uncommon 39, 40 and also drug interactions reported phyto-therapeutics in oncology 41. So, Proper and up-to-date knowledge is necessary in using alternative treatment options as patients who received alternative medicines had a 2.5 greater risk of dying compared to those who received conventional cancer treatment 42.
Reasons Behind Choosing Alternative Care
Pain is affects approximately 66% cancer patients 43, distressing or intolerable in more than one‐third of patients 44 and chronic pain is associated with primary cancer itself or metastases or its treatment (chronic post-cancer treatment pain) 43, 44, 45, 46. Although, WHO described opioids as essential medicines for pain control but distribution shows substantial inequity, a less than 20% of the world’s population consuming more than 90% of the world’s supply 46. Also, some 85% of PCPs perceived their training in pain management to be inadequate in a Pan-European survey 47. Along with these, fear of dependence, prescription diversion, regulatory scrutiny, withdrawal symptoms, opioid-related adverse events and deaths limit its use 46, 48, 49, 50, 51, 52. There is a lack of high-quality evidence regarding the analgesic efficacy of NSAIDs in cancer; contradiction and inconsistent findings also reported 53, 54, although advocated as a useful adjunct for management of cancer pain 55, 56. In addition, long-term use of NSAIDs is often associated with many serious cardiovascular, gastrointestinal, renal, and other side effects 54, 57. Some other studies also reveal association of NSAIDs with certain cancer types 58, 59. Several studies support use of cannabis/marijuana in cancer pain management 60, 61, 62, 63, 64, 65, 66, 67, 68, 69, 70. Its social acceptability is gradually increasing around the world 71, but many studies oppose it’s use or at least demand further investigation of benefit risk ratio 72, 73, 74, 75, 76, 77, 78, 79, 80. Chemotherapy and radiotherapy are still commonly conventional approaches for treatment of patients harboring advanced cancer 81. Traditional chemotherapy also associated with neuropathic pain 82, fatigue and sleep disturbance 83, anxiety and depression 84, mouth sores, nausea and vomiting, early satiety 85, alopecia 86, bone and muscle wasting 31, 87. Futile medication use in management of terminally ill cancer patients has also been reported, one-fifth of cancer patients at the end of their life took futile medications (statins and antidementia drugs in nearly 100% cases, antihypertensives and bisphosphonates in nearly 30% cases) 88. The goal of cancer palliative care is to prevent or treat, the symptoms and side effects of the cancer type and its treatment, caregiving to any related physical, emotional, social, and spiritual aspects 89, 90, 91. Some alternative therapies, like acupuncture, physical therapy, aromatherapy, CBT are widely recommended along with mind-body interventions like yoga, tai chi, meditation and mindfulness, that keep people fit and energetic as they undergo treatment 1, 2.
Herbal and Non-Herbal Plant Derivatives
Medicinal plants are a rich source of secondary metabolites with interesting biological and pharmacological activities 92. Kuruppu et.al, 2019 reported that there are 3000 plants possess some anticancer properties and nearly 75% cancer drugs are derived from natural sources, 40% of them are FDA approved 93, 94, 95, 96, 97. Only a small number of natural anti-tumor products including vinblastine, vincristine, podophyllotoxin, paclitaxel (Taxol) and camptothecin have been tested clinically, while vinflunine ditartrate, anhydrovinblastine, NK-611, tafluposide, paclitaxel poliglumex, combretastatins, salvicine, curcumin, indirubin, triptolide, homoharringtonine are still on trial 98. In addition, there are 195,000 pharmacologically active compounds for which the interactions are quantitatively known 99. According to an estimate, more than 300,000 secondary metabolites exist in nature 100. Glycosides 92, alkaloids, polyphenols, saponins, tannins and terpenoids 101 have shown promising results in cancer research. Chinese herbal medicines (CHM) also have been demonstrated to exert synergistic effects with other anticancer drugs, improved efficacy and reduced side effects 81, 102, 103, 104, 105, 106, 107, 108, 109, 110. It is an independent medical profession in Hong Kong and mainland China 108. Cancer patients used CHM to improve their physical and emotional well-beings and to reduce cancer therapy-induced toxicities 111. Nutrition and foods are related to about 30% of all the cancers cases 112. Omega-3s from fish pack a stronger punch than other oils when it comes to cancer prevention 113, 114, 115. Seaweeds are specifically used to treat tumors in CHM 116. Several studies revealed that active metabolites among the terpenoids, including carotenoids, polyphenols and alkaloids that can obtained from marine source 117, 118, 119, 120, 121, 122, 123, 124, 125. Compounds from natural sources with anti-proliferative activity represent an important and novel alternative to treat several types of cancer.
Lung Cancer
American Cancer Society estimated that in 2018 lung and bronchus cancers would be responsible for 234,030 new cases which represent 14% of all new cancer cases and 154,050 deaths 126. Non-small-cell lung cancer (NSCLC) is the most common type of lung cancer, accounting for about 80%-85% of all cases 127, 128. More than half of the NSCLC cases are diagnosed at an advanced stage (stages III and IV) 129. Smoking causes at least 80% of lung cancer deaths 130. Lin et.al, 2019 concluded association between lung cancer incidence and increased reliance on coal for energy generation 131. Other possible reasons are exposure to indoor and outdoor air pollution, exposure to radiation, and occupational exposure to agents such as asbestos, nickel, chromium, and arsenic 132. Cannabidiol (a non-psychoactive compound from Cannabis sativa), significantly inhibits the recruitment of tumor-associated macrophages (TAM) in primary tumor stroma and secondary lung metastases 133. Table 1.
Table 1. Medicinal Plants Used in Lung Cancer| Plant | Plant Parts Used | Important Constituents | Mode of Action/ Pathway Modulation/ Study Results | |
| Allium sativum L | Bulbs | Organo-sulfur compounds (OSCs) like allicin (Figure 2a), allixin (Figure 2b), diallyl sulfide, diallyl disulfide, etc. | OSCs are antioxidant, detoxify carcinogen & have antiproliferative properties. Raw garlic intake, <2 times per week, ≥2 times per week was inversely associated with lung cancer 134, 135, 136. | |
| Curcuma longa | Rhizome | Curcumin (Figure 2c) | Inhibition of telomerase activity, dose-dependent cytotoxic effect on A549 lung cancer cell line 137. | |
| Ferula assa-foetida | Resin | Conferone (Figure 2d), a sesquiterpene-coumarin | Cytotoxic effect on A549 lung cancer cell line 138. | |
| Astragalus cytosus | Root | Polysaccharide (and flavonoids of other Astragalus spp.) | Inhibit the proliferation and delay the tumor growth xenograft of human NSCLC in vivo and in vitro through the down-regulation of NF-κB activity 139. Astragalus polysaccharide injection integrated with vinorelbine and cisplatin offered an improved QOL for patients with advanced NSCLC 140. Astragalus-based CHM may increase effectiveness of platinum-based chemotherapy 141. | |
| FritillariaeThunbergii(Bei-Mu) (Figure 3a) | Plant extract | Alkaloids | MDR reversal activity on human lung adenocarcinoma parental cells A549 with dosage dependence and the apoptosis rate was increased over time 142. | |
| Platycodon grandiflorum(Jie-Geng or balloon flower) (Figure 3b) | Roots | Platycodin D (Figure 2e) (Saponin) | Blocks reduction of AKT expression by small interfering RNA (siRNA) and enhance apoptotic effect 143, Modulation of the AMPK/mTOR/AKT, MAPK signaling pathways in A549 cells 144, 145, reduces the protein level of PD-L1 in lung cancer cells 146 and enhances autophagic cell death. | |
| Catharanthus roseus | Root, stem, bark and flower | Vinca alkaloids, vinblastine, vinorelbine (Figure 2f) and vincristine | Vinorelbine plus cisplatin is used for non-small-cell lung cancer. vinorelbine and cisplatin combination in patients with stage III A and stage III B non-small-cell lung exhibited positive results 147. Resistance to chemotherapy of Vinca alkaloids (Microtubule-targeting agents) has been a major obstacle to the treatment of lung cancer 148. New generation agents that have the potential to overcome the mechanisms of resistance to the available drugs may provide new therapeutic opportunities 149. High vinorelbine blood levels were associated with severe toxicity 150. | |
| Selaginellatamariscina(Spike Moss) (Figure 3d) | Whole plant | Amentoflavone (biflavonoid) | S. tamariscina ethanolic extract (STE) potently inhibited human AKR1B10 and synergistically increased the doxorubicin anti-proliferative effect in A549 and NCI-H460 human lung cancer cells 151. STE decreased expressions of matrix metalloproteinase (MMP)-2, -9 and urokinase plasminogen activator (u-PA) reported in an older study 152. Oral administration of STE could not prevent the tumor formation but provided strong inhibition of tumor growth 153. | |
| Crocus sativus L. (Saffron) | Dried stigmas | Crocetin (natural apocarotenoid dicarboxylic acid) | In vivo protective effect 154, induction of apoptosis 155, suppression of pulmonary tumor promotion 156 and also chemosensitizer for vincristine via p53-dependent and independent pathway 157, 158. | |
| Ophiopogonis Decoction(Mài-Mén- Dōng-Tāng) (Figure 3c) | Tuber and Root | Ginsenosides, lignans, steroidal saponins, and homoisoflavanones. | Modulatory effects on apoptosis, autophagy, cell cycle progression, and cell proliferation 159. | |
| Sesbania grandiflora (Humming-bird tree) (Figure 3e) | Dried leaves | Saponosides | Methanolic fraction of S. grandiflora exerted potent antiproliferative effects in the human lung cancer cell line, A549, involve a pathway that prevents NFκB activation, induction of apoptosis with high levels of ROS intermediates 160. | |
| Toona sinensis | Leaves | Terpenoids, phenylpropanoids, gallic acid (Figure 2g) and flavonoids | Inhibited H441 xenograft tumor growth in vivo and in vitro, induction of apoptosis in vitro 161. | |
| Phyllanthus emblica and Terminalia bellerica | Fruits | Pyrogallol and gallic acid (tannin) | With doxorubicin or cisplatin resulted in a synergistic effect and the possibility of reducing the doses of the chemotherapeutic drugs 162. Antiproliferative and antitumor properties on lung cancer cells and lung adenocarcinoma xenografts due to presence of tannins (P. emblica) 163. T. belerica induced apoptosis in lung cancer through regulation of Bax/Bcl-2 is also reported 164. | |
| Cinnamomum subavenium | Leaves and bark | Subamolide A (butanolide) | Induced lung cancer cell death by ROS generation, which triggers mitotic catastrophe followed by apoptosis 165. | |
| Camellia sinensis(Tea) | Leaves | Catechins (Polyphenol) | (−)-Epigallocatechin-3-gallate (catechin), the major polyphenol in green tea induces ROS and oxidative DNA damages as well as apoptosis in vivo and in vitro 166. | |
| Panax ginseng | Roots | Saponins | Ginsenoside Rh2 mediates changes in the microRNA expression, related to angiogenesis, apoptosis, chromatic modification, cell proliferation and differentiation. Another important mechanism is the inhibition of tumor cells angiogenesis that inhibits VEGF expression in LLC. Rg3 has been found to be a potent inhibitor of invasion of several tumor cell lines H1650, H520 and H1963 in SCLC 167. | |
| Taxus brevifolia | Bark | Paclitaxel (Figure 2h)(Taxol®) (taxane dipertene) | The paclitaxel-based formulation Abraxane® is the only nanomedicine approved by EMA and the FDA in combination with carboplatin for the first-line treatment of advanced NSCLC in adult patients who are not candidates for potentially curative surgery and/or radiation therapy 168. Inhaled submicron particle paclitaxel (NanoPac®) demonstrated substantial deposition and retention of paclitaxel in sampled lung tissue in rodent model 169. | |
| Curcuma longa | Rhizomes | Curcumin(yellow polyphenol compound) | Curcumin (4 mg/kg every 2 days for a total of 7 injections) exhibits a better treatment efficacy of doxorubicin (0.4 mg/kg) in cancer due to its efflux inhibitory effect of curcumin 170. | |
Figure 1.Alternative Treatment Options 12. One third cancer patients use alternative medicine-are not well regulated and may interact with conventional treatments like chemotherapy and radiation. Some alternative therapies, like acupuncture, physical therapy, aromatherapy, CBT are widely recommended by oncologists for cancer pain management. Mind-body interventions like yoga, tai chi, meditation and mindfulness, which were each used by less than 10% of patients, can keep people fit and energetic as they undergo treatment, reduce the side effects of traditional therapies and improve patients’ sleep, stress and mental health. Many hospitals even have alternative medicine centers that offer these programs.
Figure 2.Plant derived biomolecules studied in lung cancer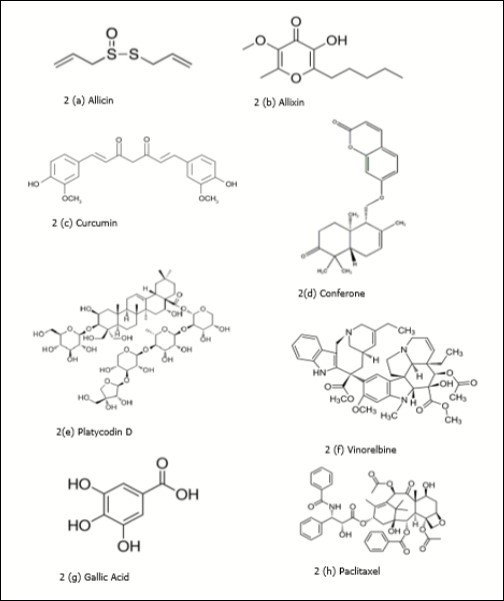
Chemotherapy remains the indispensable choice for the vast majority of patients with advanced NSCLC, including primary tumors and lung metastases 168, 171. Use of the pulmonary route is a promising way to decrease the severe systemic toxicities associated with chemotherapy. Inhalation allows the administration of high drug doses directly to lung tumors without prior distribution in the organism 172, 173. However, Bei-Mu, Jie-Geng, and Mai-Men-Dong-Tang are important CHMs that have improved the survival rate 174. Euphorbia mauritanica and Kedrostishirtella extracts may play a role in inducing cell death in lung cancer cells 175. Several 2019 reviews reveal fucoidans (sulfated polysaccharide mainly derived from brown seaweed) in lung cancer management. Brown algae like Fucusvesiculosus, Turbinariaconoides, Laminaria japonica (Figure 3g) are reported in inhibition of tumor migration and invasion, apoptosis induction and inhibition lung cancer cell progression respectively 176. Fucusevanescens, Sargassum sp., Saccharina Japonica was reported to inhibit proliferation and metastasis, and inducing apoptosis in vitro 177. Undaria pinnatifida acted on ERK1/2 MAPK and p38, PI3K/Akt signaling, F. evanescens increased metastatic activity of cyclophosphamide and showed cytolytic activity of natural killer cells in 2 different studies and F. vesiculosus (Figure 3f) decreased NF-κB in LLC 178. U. pinnatifida (Figure 3h) was found to show average antitumor and superior efficacy against LLC in review of Misra et.al, 2019 179. Sponge alkaloids from Aaptos showed potential in human lung adenocarcinoma A549, from Fascaplysinopsis exerted an anti-proliferative and pro-apoptotic effect in lung cancer, from blue sponge Xestospongia showed apoptosis as well as stimulate anoikis in H460 lung cancer cells in review by Ercolano et.al, 2019 180. Polyphyllin D from Paris polyphylla is well known for its induction of endoplasmic reticulum (ER) stress and mitochondria-mediated apoptotic pathways against lung cancer 181. High fish consumption was significantly associated with a decreased risk of lung cancer 182, 183. Possible mechanism could be changes in formation of PGE2 and PGE3 and alteration of Akt phosphorylation 184. However, other studies reveal healthy dietary intake like high fruit, vegetable, soy protein, poultry (white meat), low-CHO, fish oil-containing diets, together with exercise also decline risks of lung cancer among non-smokers 185, 186, 187. Conversely, long-term use of high doses of some supplements, such as retinol, β-carotene, B vitamins, and vitamin E, increase lung cancer risk in current and former smokers 188. Smokers should continue to avoid β-carotene supplementation 189, 190. When a person stops smoking before the age of 40, they reduce their chances of dying from smoking-related disease by 90% 191. Telephone counseling reduce cost of nicotine replacement therapy (NRT). Again, cessation with intensive telephone counseling and NRT could be over 20% 186. Also, lung cancer mortality can be reduced by 20% via low dose CT lung cancer screening and treatment of early-stage disease 192.
Figure 3.Plants studied in lung cancer (3a). Fritillariae Thunbergii (Bei-Mu) (Source: Inner Path)
Figure 3(b).Platycodon grandiflorum (Jie-Geng) (Source: Wikipedia)
Figure 3(c).Ophiopogonis Decoction (Mài-Mén- Dōng-Tāng)
Figure 3(d).Selaginella tamariscina (Spike Moss)
Figure 3(f).Fucus vesiculosus L. (Source: Seaweed Site of M.D. Guiry)
Figure 3(g).Sesbania grandiflora (Humming-bird tree)
Figure 3(h).Undaria pinnatifida (Source: The Marine Life Information Network)
Blood and Bone Marrow Cancer (Leukemia)
Hematopoietic cancers constitute a diverse group of diseases including leukemias, lymphomas, plasma cell tumors, myelodysplastic syndromes, and mastocytosis. They arise primarily from two categories of immunological cell types, myeloid and lymphoid cells 193. AML is the most common form of acute leukemia in adults, accounting for over 80% of all diagnosed acute leukemias 194, 195. Globally, between 1990 to 2018, the number of leukemia cases markedly increased from 297,000 to 437, 033 196, accounting for close to 250,000 annual deaths due to AML worldwide 197. Optimization of post-remission therapies to maintain complete remission and prevent relapse is a major challenge in treating patients with AML 198. Children with Down syndrome have a 150-fold increased risk of developing AML and 20-fold increased risk of developing ALL 199. The incidence of ALL is about 3.3 cases per 100,000 children 200. Outcomes for patients with CML have substantially improved due to advances in drug development and rational treatment intervention strategies 201. Allowed costs for leukemia patients averaged almost $157,000 in the year after diagnosis, with costs for AML almost tripling that amount, according to a new report from the Leukemia & Lymphoma Society (LLS) 202. Table 2.
Table 2. Traditional Plants Used in Leukemia| Plant | Plant Parts Used | Important Constituents | Mode of Action/ Pathway Modulation/ Study Results |
| Zingiber officinale | Rhizome | 6-gingerol (Figure 4a), 6-shogaol (Figure 4b), and 6-paradol. | Combined with MTX showed synergistic effects on CCRF-CEM, Nalm-6 and ALL primary cells 203. 8-shogaol, originated from ginger, elevated the level of ROS, c-caspase-3, -9, c-PARP, c-DFF-45, and decreased the level of glutathione, MMP, caspase-8 and Bid 204. Enhanced cell growth inhibition while combined with Nerium oleander and imatinib 205. |
| Paris polyphylla | Tubers | Polyphyllin D (Figure 4c) (Steroids) | Polyphyllin D induces apoptosis and differentiation in K562/A02 cells through G2/M phase arrest 206, 207. |
| Withaniasomnifera(Ashwagandha/'Indian ginseng') | Root or the whole plant | Alkaloids, flavonoids, steroids, and terpenoids | Significant cytotoxic and cytostatic potential human T-lymphoblastoid cell line, and induces ICD. Its proapoptotic mechanism involves intracellular Ca2+ accumulation and the generation of ROS 208. Withaferin- A (Withanolides, steroids) from the root induced oxidative stress in human leukemia HL-60 cells 209, 210. |
| Cephalotaxusharringtonia(Korean plum) | Leaves | Homoharringtonine (Figure 4d) (non-proprietory name omacetaxine mepesuccinate, alkaloid) | Suppression of the SP1/TET1/5hmC/FLT3/MYC signaling pathways in AML 211. Elevated ROS generation in *etoposide-treated AML cells and exhibited synergistic cytotoxicity 212. Combined treatment with HSP90 inhibitor provides an alternative way for the treatment of FLT3-ITD positive AML 213. FDA approved for treatment of patients with CML resistant or intolerant to tyrosine kinase inhibitors (TKI) 214. Also reported synergism with Ibrutinib (BTK) 215 and arsenic trioxide on AML stem cells by KG-1 (CD34+/CD96+/CD38+/-) and Kasumi-1 (CD34+/CD38-) cells 216 and by suppressing Mcl-1 through glycogen synthase kinase-3β (GSK3β) 217. Deregulates MYC transcriptional expression by directly binding NF-κB repressing factor and potentiates the therapeutic efficacy of anthracycline/cytarabine induction regimens 218. |
| Ancistrocladus cochinchinensis | Leaves | Naphthalene derivatives and isoquinoline alkaloids | Expresses cytotoxicity against HL-60 cancer cells 219. |
| Chondrodendron platyphyllum | Root barks | Curine (4e)(Bisbenzyl-isoquinoline alkaloid) | Disrupts MMP and curine presented a cytotoxic effect and induced apoptosis in HL-60 cells 220. |
| Alpinia intermedia (Hardy Wild Ginger) | Seeds | Intermedin A (calcitonin family peptide, labdane diterpene) | Increases cleaved (c)-PARP and c-caspase-3 levels, thus inducing apoptosis in HL-60 cells at a dose of 30 µg/mL 221. |
| Thalictrum cultratum(Meadow-rue) | Root | Thalicultratine C (Aporphinoid Alkaloids) | Downregulates MMP and induces apoptosis 222 |
| Artemisia annua L. (sweet wormwood) | Leaves | Artemisinin (Figure 4f) (sesquiterpene lactone) | Initiation of apoptotic cell death through ROS dependent and independent mechanisms, inhibition of cancer proliferation, metastasis and angiogenesis, and modulation of the cell signal transduction pathway and cause lysosomal disruption 223, 224. Combination of artesunate with lenalinomide, commonly used for the treatment of Multiple Myeloma 225. Hybrid 25 which proved even more potent than clinically used doxorubicin against CEM/ADR5000 cells 226. Significantly enhanced NK-92MI cell (natural killer cells) cytotoxicity against K562 cell line 227. |
| Clausenalansium(Wampee) | Stems | Coumarins (8-geranyloxypsolaren) and 2-methoxy-1-(3-methyl-buten-1-yl)-9H-carbazole-3-carbaldehyde | Cytotoxicity against K562 cell line 228. |
| Hericiumerinaceus(Yamabushitake, mushroom) | Whole plant | polysaccharide | Activation of mitochondria-mediated caspase-3 and caspase-9, induce apoptosis through down-regulation of anti-apoptotic proteins (Bcl-2, Bcl-xL(S), XIAP, and cIAPs) in U937 human monocytic leukemia cells 229. |
| Inonotus obliquus(Chaga mushroom) | Whole plant | Inonotodiol and inonotsuoxides (lanostan-type triterpenoids) | Inotodiol inhibits cell proliferation through apoptosis induction by activating caspase-3 230. |
| Allium sativum | Bulbs | Ajoene (Figure 4g) (OSC) | Ajoene induced apoptosis in human leukemic cells via stimulation of peroxide production, activation of caspase-3-like and caspase-8 activity 122, 231. The MAPK family member ERK1/2 was also activated by bisPMB (Ajoene Analogue) 232. |
| Securinega suffruticosa | Callus | Virosecurinine (Figure 4h) (alkaloid) | Inhibits proliferation and induce apoptosis in THP-1 cells by exerting an inhibitory effect on the activation of PI3K/AKT/mTOR signaling pathways 233. Inhibited the growth and proliferation of the K562 cell lines and induced apoptosis in K562 cells by affecting the expression of mTOR, SHIP2, BCR/ABL and PTEN 234. |
| Cynanchum atratum | Root | BW18 (a C-21 steroidal glycoside) | Potential alternative for CML patients. Regulating MAPK pathway leading to S phase cell cycle arrest and apoptosis, inhibited cell viability and proliferation of K562 cells 235. |
| Curcuma longa | Rhizomes | Curcumin(yellow polyphenol compound) | Curcumin targets multiple enzymes (eg. NRF2 targeted NQO1) involved in the ROS metabolic pathway to suppress tumor cell growth, increases ROS levels in CML-derived human leukemic cell 236, 237, 238. Potentiates the efficacy of vincristine and imatinib, significantly increased the apoptosis degree, decreased the activation of NF-κB and the expression of its regulated genes 239. |
| Camellia sinensis(Tea) | Leaves | Epigallocatechin gallate (EGCG) (Catechin) | Inhibits growth of human myeloid leukemia cells through the regulation of pRb synthesis and formation of pRb-E2F complexes 240. Causes caspase-independent necrosis-like cell death in CML 241. In early-stage CLL, the use of 2g of EGCG from the green tea extract twice a day was able to reduce the absolute leukocyte count 242, 243, 244, 245, 246. EGCG was also shown to inhibit DNA replication in leukemia cell lines and to modulate vascular endothelial growth factor leading to apoptosis in leukemic cells 247, 248. |
| Vitis vinifera(Grape) | Seed | Proanthocyanidins, Resveratrol (Figure 4i) (Phenols) | Involves sustained JNK activation and Cip1/p21 up-regulation, culminating in caspase activation 249, 250, apoptotic cell death and cell growth arrest in human promyelocytic leukemia HL-60 cells 251. Effective against the proliferation of both types of acute leukemic lymphocytes of AML and ALL patients 252. Polydatin, a natural precursor of resveratrol (RSV) induces cell cycle arrest and apoptosis in MOLT-4 leukemia cells 253. Combination of chloroquine with RSV and 2 other stilbenes induced significant cell death and toxicity in on RCH-ACV and 697 ALL cells 254. RSV is a molecule without known severe toxicities 255. Proanthocyanidin extract induced mitochondria-associated apoptosis in human AML 14.3D10 cells 256. |
| Punicagranatum(Pomegranate) | Fruit | Gallic acid, ellagic acid, caffeic acid, chlorogenic acid, cyanidin, delphinidin, pelargonidin, gallotannins and ellagitannins | Induced apoptosis and preferentially alters the cell cycle in leukemia cell lines compared with nontumor control cells 257. Flavonoid-rich fractions had proportional inhibitory effects on HL-60 cell proliferation 258. Peel extract promotes growth inhibition of K562 cells mainly via G2/M phase arrest while still conserving apoptosis induction, but at a lower rate 259. Juice extract significantly induced apoptosis in all leukemic cell lines and also induced cell cycle arrest in vitro 260. The polysaccharide PSP001, isolated from the rind of pomegranate fruit exhibited anti-oxidant activity in addition to growth inhibitory effect on leukemic cell lines 261. |
| Panax ginseng | Root | Ginsenoside | Ginsenoside Rh1 showed a suppressive effect on the MAPK signaling pathway, resulting inhibition of invasion and migration of THP-1 acute monocytic cells 262. A metabolite of ginseng saponin, compound K induced apoptosis in human leukemia cells and also induced the activation of caspase-3, -8, and -9, and modulation of Bcl-2 families 263. In addition to cell growth inhibition, compound K suppresses cell DNA synthesis and induces cell cycle arrest at G1 phase in pediatric AML 264. It might have antileukemia activity through CD11c+ cell-mediated antitumor immunity 265. Down-regulated the expression of human telomerase reverse transcriptase, with inhibiting the expression of c-Myc in a concentration-dependent manner 266. |
| Podophyllum emodi(Indian Origin), Podophyllum peltatum(American origin) | Roots and rhizomes | Podophyllotoxins | Podophyllotoxin derivatives showed promising cytotoxicities against a set of human cancer cell lines HL-60 267. Teniposide and etoposide have been reported as inhibitors of MYB transcription factor 268. GMZ-1 suppresses growth and induces apoptosis in adriamycin-resistant K562/A02 cells through modulation of MDR1 expression 269. A398was cytotoxic to the HT-29, MCF-7, MOLT-4 and HL-60 tumor cell lines 270. |
| Coleus forskohlii | Root | Forskolin (Diterpene) | Forskolin as a GSKJ4 sensitizer/adjuvant in vivo, sensitizes Human AML Cells to H3K27me2/3 eemethylases GSKJ4 Inhibitor via Protein Kinase A 271. |
| Andrographis paniculate(Green Chirata) | Leaves | Andrographolide (Figure 4j) (Diterpene) | Pretreatment of U937 with andrographolide (AGP) followed by low doses of topotecan showed an enhancement in inducing apoptosis 272. Inhibits growth of human T-ALL Jurkat cells by downregulation of PI3K/AKT and upregulation of p38 MAPK pathways 273. AGP was most potent to induce cytotoxicity in NALM-6 cells, effectively induced apoptosis by arresting cell cycle progression and increased the nuclear break down in NALM- 6 leukemic cells 274. Cell cycle arrest and mitochondrial-mediated apoptosis in human leukemic HL-60 cells also reported 275. Along with potent derivative NCTU-322, downregulated Bcr-Abl against imatinib-resistant CML cells 276. Inhibits growth of acute promyelocytic leukemia cells by inducing retinoic acid receptor-independent cell differentiation and apoptosis 277. inhibits MV4-11 cell proliferation and reduces drug resistance by blocking FLT3 signaling in AML 278. |
Pterostilbene (Figure 4k) (phytoalexin) isolated from grapevine leaves and blueberries, showing no toxicity in humans up to a dose of 250 mg/day 279, increases Fas expression in T-lymphoblastic leukemia cell lines 280. Blueberry extracts exerted anti-AML efficacy and specifically provoked Erk and Akt regulation within the leukemia stem cell subpopulation 281. Quercetin (Figure 4l) is a polyphenol partially responsible for the anti-AML efficacy of blueberry extracts. It can augment and focus the anti-AML efficacy of nano-liposomal ceramide (Lip-C6) and other ceramide-based therapeutics 282. Plant Homeodomain Finger 6 (PHF6) is frequently mutated in T-cell ALL (T-ALL), or AML 283, are present in about 20% of T-ALL that causes self-renewal and hematopoietic recovery after chemotherapy 284. PHF6 mutations have a significant role in leukemia stem cell activity in the pathogenesis of T-ALL 285. PHF2 low expression was significantly associated with leukemia cell proliferation and several poor prognostic indicators in adult ALL patients. By restoring IKAROS function (zinc finger transcription factor encoded by the IKZF1 gene), PHF2 can be promoted through histone modification 286. Sarkar et.al, 2019 depicted plants of West Bengal (bark of Flacourtiaindica, leaves of Madhucalongifolia (Figure 5b) and Prosopis cineraria) (Figure 5c) showed better cytotoxicity in both AML and CML cell lines (HL-60 and K562) 287. Danışman et.al, 2019 reported combination of flavonoids (apigenin, luteolin, 5-desmethyl sinensetin) and imatinib mesylate were able to enhance the cytotoxic effect on K562 cells in CML 288. Fucoidan (complex polysaccharide from brown seaweeds) inhibited proliferation of the SKM-1 AML cell line via the activation of apoptotic pathways and production of ROS 289 and also induced apoptosis in U937 Cells through activation of p38 MAPK and modulation of Bcl-2 Family 290. In another studies, in vitro and in vivo growth suppression 291 and enhancement of therapeutic potential of arsenic trioxide and all-trans retinoic acid 292 in acute promyelocytic leukemia cells also reported. Fucoxanthin (Figure 4m) induced apoptosis in human promyelocytic leukemia HL-60 cell 293, inhibited growth of leukemia cell lines by ROS generation 294, inhibited phosphorylation of ERK1/2 and histone H3, which are direct downstream signaling targets of lymphokine-activated killer T-cell-originated protein kinase (TOPK) 295, increased cytotoxicity against K562 cells and decreased cell proliferation of K562 and TK6 cells in vitro in imatinib and doxorubicin combination 296. Phlorotannins (algal polyphenols) showed antiproliferative activity in vitro against human leukemia THP-1 and U-937 cells 297. Heteronemin (Figure 4n) (a marine sesterterpenoid) effectively down-regulated cytarabine-induced activation of MAPK, AP-1, NF-κB and c-Myc, the down-stream targets of Ras signaling 298. Cichoriumintybus, Rheum ribes, Alhagipseudalhagi and Glycyrrihza glabra (Figure 5a) (Iranian Traditional plants) also showed notable effects on the leukemia cell lines 299. Juniperus sp. (Figure 5d) can be considered as an alternative source of podophyllotoxin (Figure 4o) and deoxypodophyllotoxin 300.
Figure 4.Plant derived biomolecules studied in leukemias
Figure 5.Plants studied in leukemias (a). Glycyrrhiza glabra (Licorice)
Figure 5(b).Madhuca longifolia (Mahua/Madhuca) (Source: Useful Tropical Plants - Ken Fern)
Figure 5(c).Prosopis cineraria (Khejri/Shami tree) (Source: Greensouq.ae)
Figure 5(d).Juniperus communis (Common Juniper) (Source: IUCN Red List)
Breast Cell Carcinoma
The most common breast cancer type is the invasive ductal carcinoma accounting for 70-80% of all breast cancers diagnosed 301. It starts in a milk passage (a duct), breaks through the wall of the duct and invades the tissue of the breast 302. In US, 232,000 new cases of breast cancer were diagnosed 303 and claimed the lives of 40,290 women 304 in 2015. First-degree relatives of patients with breast cancer have a 2-fold to 3-fold excess risk for development of the disease 305. BRCA1 and BRCA2 are the 2 most important genes responsible for increased breast cancer susceptibility 306. Early breast cancer detection programs depend for effectiveness on the participation rate, which is affected by risk factor awareness 307. Since 1990, between 384,000 and 614,500 breast cancer deaths have been averted due to increased mammography screening and improved treatment 308. However, more than 25% breast cancer is projected to be increased by 2020 309. Women with breast cancer had a higher risk of developing new comorbidities than women without cancer 306. stressful life 310, urban living, mastectomy 311, lower socioeconomic status 309, 312, genetic predisposition, African-American origin, not having children or breastfeeding, early menstruation/late menopause, obesity, alcohol abuse, HRT after menopause, benign breast conditions or having breast proliferation, using contraceptives and exposure to diethylstilbestrol 313, age between 40-60, late age first pregnancy, smoking 314, abortion history 315 are the associated factors. Distressingly, the 5-year cumulative mortality remains unacceptably high at 50%, primarily due to a late-stage presentation 316. Wearing bra is not associated with breast cancer risk 317 but wearing (tight) bras for many hours and having breast implants 315, 318 may have associations. Around 60% of breast cancer mortality occurs in LMICs 319. The prevalence costs of breast cancer care in the US in 2010 was $16.5 billion 320, 321, and exceeded $39 billion before 2017 322. Table 3.
Table 3. Traditional Plants Used in Breast Cell Carcinoma| Plant | Plant Parts Used | Important Constituents | Mode of Action/ Pathway Modulation/ Study Results |
| Podophyllum peltatum | Roots and rhizomes | Etoposide (Figure 6e) and teniposide (semisynthetic derivatives of podophyllotoxin) | Target topoisomerase II and forms a complex with topoisomerase II and DNA. The complex induces breaks in double-stranded DNA and prevents repair by topoisomerase II binding 93. Etoposide alters the balance between CDC25 splice variants in human breast cancer cell lines both at the mRNA and protein levels 323. |
| Juniperuscommunis(Juniper Berry) | Leaves | Deoxypodo-phyllotoxin(aryltetralin lignan or cyclolignan) | Induced apoptosis in malignant MB231 breast cancer cells and inhibited MAPK/ERK and NFκB signaling pathways within hours of treatment 324. Antitumor effect of DPT on MDA-MB-231 human breast cancer xenografts in vivo 325 and in vitro 326. Better efficacy to MDR breast cancer than paclitaxel via avoiding efflux transport 327. Crude aqueous extract of J. communis L. significantly decreased the growth of MCF-7/AZ breast cancer cells 328. |
| Catharanthus roseus | Root, stem, bark and flower | Vinorelbine, vindesine, vincristine and vinblastine (Vinca alkaloids, microtubule inhibitors) | Vinca alkaloids showed Golgi-disrupting activity in 3 different human breast cancer cell lines, BSY-1, MDA-MB-231 and MCF-7 329. Possible involvement of miR-222-3p expression in breast cancer cell apoptosis 330. Quercetin and vincristine are both active against ER breast cancers and exhibit synergism in vitro 331. Vinorelbine-phospholipid complex reduced injection irritation and maintain an antitumor effect in breast cancer in mouse models 332. |
| Taxus brevifoliaand Taxus baccata | Trunk bark | Paclitaxel and docetaxel (Taxanes) | Taxanes are among the most active chemotherapy agents in the management of metastatic breast cancer, associated less nausea and vomiting compared to non-taxane-containing regimens 333, 334, disrupt the equilibrium between polymerized and depolymerized forms of microtubules, the cellular structures required for cell division 335. Paclitaxel+ bevacizumab exhibits synergetic effects and anti-tumor efficacy 336. Paclitaxel/cyclophosphamide better tolerated adjuvant regimen for elderly patients than docetaxel combination in elderly patients 337. Intensive paclitaxel NCT has the lowest incidence rate of neutropenia among other available NCTs 338. Docetaxel combined with trastuzumab and Pertuzumab is the standard first-line therapy for HER2-positive metastatic breast cancer 339, regimens containing docetaxel were associated with lower CIPN severity than paclitaxel 340. Adding taxane to an anthracycline-based regimen improves survival in node-positive breast cancer patients 341. Taxane/cyclophosphamide was more effective than taxane/anthracycline in HER2-negative, breast cancer 342. |
| Syzygiumaromaticum(cloves) | Stems and flowers | β-caryophyllene (Figure 6a) (Sesquiterpene), Eugenol (Essential oil) | Dried flower buds of cloves lowered VEGF-A expressions at high dose and decreased MDA in vivo, induce adoptosis, decrease in CD24 and EpCAM expression in mammary cells 343. β-caryophyllene potentiated the anticancer activity of paclitaxel by facilitating the passage of paclitaxel through the plasma membrane 344. β-caryophyllene induced ionstitutive activation of PI3K/AKT/mTOR/S6K1 signaling and activation of ERK, JNK, and p38 MAPK in tumor cells 345, suppressed constitutive STAT3 activation in breast cancer cell lines and found cytotoxic to MDA-MB-231 346. Eugenol inhibits the cell proliferation and induces the apoptosis in human MCF-7 breast cancer cells 347. |
| Angelica archangelica | Leaves | β-phellandrene (Figure 6b) (cyclic monoterpene) | Moderate antiproliferative activity against Crl mouse mammary carcinoma cells in vitro 348. |
| Nigella sativa | Seed | Thymoquinone (Figure 6c) | Sustained inhibition of breast cancer cell proliferation with long-term treatment potential 349. |
| Viscum Album(European mistletoe, a hemi-parasitic shrub) | Leaves | Mistletoe lectin | Cytotoxic effect breast cancer cells (MFM-223, HCC–1937, KPL-1, MCF-7) 350. Addition to targeted therapy (with mAbs, TKIs, ICIs) significantly reduced adverse effect induced treatment discontinuation 351. Devoid of herb-drug interaction and interference with cytostatic effects of trastuzumab on SK-BR-3 cells in vitro 352. Decreased cell proliferation, increased apoptosis and necrosis reported with human ductal breast carcinoma cell line BT474 353. An increase in the number of neutrophils and the activation of the phagocytic cells also reported with V. Album354. Apoptosis was induced by the activation of its mitochondrial pathway 355. |
| Camptotheca acuminate(xǐ shù or happy tree) | Leaves | Camptothecin (Figure 6d)(Insoluble pentacyclic mono-terpene alkaloid) | Low dosage camptothecin combined with oncolytic measles virus found to elicit the same therapeutic effect as high doses of camptothecin in breast adenocarcinoma 356. |
Figure 6.Plant derived biomolecules studied in breast cancer
Ethanolic extract of Juniperus turbinate was more potent cytotoxic than cisplatin in human breast adenocarcinoma MDA-MB-231 cell lines 357. Juniperusoxycedrus ethanolic extract from needles and berries showed potent cytotoxic effects against two breast cancer cell lines (MDA-MB-468 and MCF-7), with no cytotoxicity towards normal cells (PBMCs) 358. Saturejakhuzistanica (Figure 7a) (Lamiaceae), Casearia Sylvestris (Figure 7b) (Salicaceae), Cedrelopsisgrevei (Rutaceae), Solaniumspirale Roxb. (Solanaceae), carbazole alkaloids, Helichrysumgymnocephalum (Asteraceae), Pituranthostortuosus (Apiaceae), Melaleuca armillaris (Myrtaceae), Rosmarinus officinalis (Lamiaceae), Schinus molle L. and Schinus terebinthifolius Raddi(Anacardiaceae), Erigeron acris L.(Asteraceae), Aquilaria sinensis (Thymelaeaceae), Thymus vulgaris L. (Lamiaceae), Schefflera heptaphylla L. (Araliaceae) showed antiproliferative actions on human MCF-7 breast cancer cells 359. XWL-1-48, a potent orally podophyllotoxin derivative suppress Topo II, induce DNA damage and apoptosis, blocks PI3K/AKT/Mdm2 pathway 360. Alteration of Chk-2 signaling in MCF-7 cells reported with 4'-Demethyl-deoxypodophyllotoxin glucoside isolated from Podophyllum hexandrum(Figure 7c)361. Genistein (most abundant and active isoflavone in soy), binds to the FIH-1 binding site of HIF-1α protein and downregulates HIF-1α in breast cancer cell line 362. Individuals with the habit of green tea (due to presence of EGCG) were found to have a negative association with the risk of future breast cancer (significantly increases circulating estradiol) 363, 364, 365, 366, 367, 368, 369, 370, 371, 372, 373. Compared with the US and EU, some Asian countries like China and Japan have lower breast cancer 364, where dietary consumption of soy products is much higher than US and EU 374. Brown seaweed fucoidan inhibited human breast cancer progression by upregulating microRNA (miR)-29c and downregulating miR-17-5p, thereby suppressing their target genes 375. Lophocladia sp (Lophocladines), Fucus sp (fucoidan), Sargassum muticum (7f) (polyphenol), Porphyra dentata (sterol fraction), Cymopoliabarbata (Figure 7e) (CYP1 inhibitors), Gracilariatermistipitata was found to be effective in breast cancer studies 376. High Urokinase-type plasminogen activator receptor (uPAR) expression predicts for more aggressive disease in several cancer types 377, dietary seaweed may help lowering breast cancer incidence by diminishing levels of uPAR 378. The tropical edible red seaweed Eucheuma cottonii L. (Figure 7d) is rich in polyphenols that exhibited strong anticancer effect with enzyme modulating properties 379. Jazzara et.al, 2016 concluded that λ-carrageenan (Figure 6f) (sulfated galactans found in certain red seaweeds) could be a promising bioactive polymer 380, showed a remarkable inhibitory effect on MDA-MB-231(triple negative breast cancer cell line) cell migration 381. Several studies support polyphenols 382, 383, 384, 385, 386, flavonoids 387, 388, 389, 390, 391, 392, 393, 394, 395, fucoidan 396, 397, 398, 399, 400, 401, 402, 403, 404, 405, 406, 407, lutein/zeaxanthin 408, 409, 410, 411, 412, other seaweed alkaloids, peptides, tannins and polysaccharides 413, 414, 415, 416, 417, 418, 419, 420, 421, 422, 423, 424, 425 in breast cancer management.
Figure 7.Plants studied in breast cancer (a). Satureja khuzistanica (Source: Med P Group)
Figure 7(b).Casearia Sylvestris (Source: Árvores do Bioma Cerrado)
Figure 7(c).Podophyllum hexandrum (Source: Wikimedia Commons)
Figure 7(d).Eucheuma cottonii (Source: tradekey.com)
Figure 7(e).Cymopolia barbata (Source: Melev's Reef)
Colorectal Cancer
Colorectal cancer (CRC) is the third most common cancer worldwide and the fourth most common cause of cancer death 426. It is the second leading cause of death in US, affecting some 135,000 estimated new patients with more than 50000 deaths every year 427, 428, 429. In 2015, there were 376,000 new cases and 191,000 deaths in China 430. The overall incidence of CRC is decreasing in many high-income countries, although reported significant increase in Denmark, New Zealand, Australia, UK and Canada, mainly driven by increases in distal (left) tumors of the colon and predominant in 431, 432, 433, 434, 435, 436, 437, 438. Lifestyle determines around 50% to 60% incident of CRC irrespective of age 439, 440, 441, 442. Physical activity may prevent approximately 15% of the colon cancers 443. Fish, poultry, cheese, fruit, vegetables, tea and coffee were not associated with colorectal-cancer risk 444. Alcohol consumption, red meat/processed meat, junk food, smoking, diabetes and obesity potentiate the same risk 445, 446, 447, 448. In 2018, the estimated national expenditure was $16.6 billion in US, which was $4.5 billion to $9.6 billion in 2009 and projected to be more than $20 in 2020 449, 450, 451. There were over 1.8 million new cases in 2018. Hungary, North Korea, Slovakia, Norway, Denmark, Portugal, Japan are in the top-ranking positions 452. 5-year survival for patients with stage IV CRC is less than 10% 453. The overall risk of CRC among patients with ulcerative colitis is about ten times higher than that of the general population 454. A recent study reveals that chili peppers does not increase or decrease the risk of CRC 455. Previous studies say capsaicin has both carcinogenic and anticancer effects. Table 4.
Table 4. Traditional Plants Used in Colorectal Cancer| Plant | Plant Parts Used | Important Constituents | Mode of Action/ Pathway Modulation/ Study Results | |
| Inula Viscosa | Leaves | Polyphenols (caffeoylquinic acid (Figure 8a), dicaffeoylquinic acid, flavonoids, terpens, lactones) and sesquiterpens (Tomentosin and Inuvisocolide) | Affects the cell cycle progression and induces apoptosis by activation of caspases in colon cancer cells. Moreover, IV extract exhibits anti-tumor activities in an animal model, and it is safe for use 456. | |
| Matricaria chamomilla | Flowers | Flavonoids | Apigenin (4′,5,7-trihydroxyflavone) suppressed the EMT, migration, and invasion of human colon cancer by inhibiting the NF-κB/Snail pathway 457. | |
| Curcuma longa | Rhizome | Curcumin | Inhibit activation of NF-κB, downregulates anti-apoptotic, cell-proliferative, invasive, and angiogenic gene products, suppress activation of STAT3, HIF-1, PPAR and expression of TNF, IL-1, IL-6 458. | |
| Zingiber officinale | Rhizome | 6-gingerol and 6-paradol, shogaols and zingerone | 6-gingerol, regulate the molecules in cellular signal transduction pathways, including NF-κB, AP-1, growth factors, chemokines, MAPK, p53, cyclin D1, VEGF, COX-2 and iNOS pathways. 6-gingerol and 6-paradol have been found to induce cancer cell apoptosis 458. | |
| Alpinia galanga | Rhizome | 1′-Acetoxychavicol acetate (ACA) (Figure 8b) | ACA has been shown to induce apoptosis in CRC cell lines, inhibits DNA synthesis, thereby inhibiting cell proliferation. In rat intestine epithelial cells (IEC6), ACA induced glutathione S-transferase and NAD(P)H: quinone oxidoreductase 1 (NQO1) activities, increased intracellular glutathione levels, and upregulated intranuclear Nrf2 and cytosolic p21. It also has the ability to inhibit azoxymethane-induced colon tumorigenesis in rats 458. | |
| Piper longum(Long pepper or pipli) | Dried fruit | Piperlongumine (Figure 8c) | Piperlongumine targets Ras/PI3K/Akt/mTOR signaling axis to inhibit tumor cell growth and proliferation in DMH/DSS induced experimental colon cancer 459. | |
| Rhizomacoptidis(Huang Lian) | Rhizome | Berberine (Figure 8d) | Downregulates β-catenin-induced proliferation by binding RXR, cell proliferation by inducing the G2/M phase arrest and down-regulated the expression of the related cyclins 460. Promotes apoptosis of CRC via regulation of the long non-coding RNA (lncRNA) cancer susceptibility candidate 2 (CASC2)/AU-binding factor 1 (AUF1)/B-Cell CLL/Lymphoma 2 (Bcl-2) axis 461. | |
| Punicagranatum(Pomegranate) | Fruit | Ellagitannins, ellagic acid | CDKN1A (p21, Cip1) induction followed by cell-unique downregulation of miR-224 or upregulation of miR-215 462. Pomegranate ellagic acid and their microbiota metabolites urolithins exert anticancer effects in preclinical CRC models, and target normal and malignant colon tissues in CRC patients 463. Consumption of the pomegranate extract was significantly associated with a counterbalance effect in the expression of CD44, CTNNB1, CDKN1A, EGFR and TYMs 464. | |
| Phaseolus vulgaris(Navy bean) | Beans | Anacardic acid (Figure 8e) and nobiletin | Imparts glutathione regulation, and involved cancer control mechanisms such as detoxification of xenobiotics, antioxidant defense, proliferation, and apoptosis. Metabolic pathways involving lysine, and phytochemicals were also modulated by navy bean intake in CRC survivors 465. Anacardic acid efficiently repressed expression of CD44 and MMP14 in HCT116 colon cancer cells, with repression of the SUMO-conjugated TFAP2A isoform and elimination of CD44+/hi/ALDH+/hi cells 466. | |
| Macleaya cordata | Leaves | Sanguinarine (8f) | Sanguinarine decreased the tumor size in a dose-dependent manner in orthotopical colorectal carcinomas through intrinsic apoptosis pathway in BALB/c-nu mice. It dephosphorelates STRAP and MELK and disassociates the interaction between them to trigger intrinsic apoptosis. Overexpression of STRAP and MELK may be markers of CRC and their disassociation may be a determinant of therapeutic efficacy 467. | |
| Betula alba (white birch) | Bark | Betulinic acid (Pentacyclic triterpenoid) | Significantly reduced the expression of matrix metalloproteinase (MMPs) and increased the expression of MMPs inhibitor (TIMP-2), MMP-2+ cells and Ki-67+ cells were reduced and cleaved caspase-3+ cells were increased in tumor tissues of mice. Betulinic acid promoted the apoptosis of CRC cells and also inhibited the metastasis of cancer cells 468. Nano-capsulated analogue (2c) with better therapeutic efficacy than parent molecule to colon carcinoma cells has been reported 469. | |
| Boswellia serrata | Oleo-gum-resin | 3 acetyl-11-keto-β-boswellic acid (AKBA) | AKBA induced upregulation of tumor-suppressive miR-34a and downregulation of miR-27a in CRC cells, inhibited cellular proliferation, induced apoptosis and cell-cycle arrest in CRC cell lines, and these effects were significantly enhanced with combined treatment of AKBA and curcumin 470. | |
| Toxicodendronvernicifluum(formerly known asRhusverniciflua) | Stokes | Butein* (3,4,2',4'-tetrahydroxychalcone, aromatic ketone) | The depletion of securing (onchoprotein) enhances butein-induced apoptosis and tumor inhibition in human CRC. 471, 472, 473. Synergistic effects of butein and cisplatin, induce combined inhibition of p38α and MEK specifically induced apoptosis through caspase-3 in CRC cells 474. Butein ameliorated colitis (most important risk factor of CRC) in IL-10(-/-) mice by regulating IL-6/STAT3 and MMP-9 activation 454. | |
| Capsicum annuum(Chili pepper) | Fruit | E-capsaicin (8-methyl-N-vanillyl-trans-6-nonenamide) | Chili peppers can promote digestive juice to secrete and accelerate bowel movements, which may reduce the risk of CRC. Capsaicin can downregulate the expression of COX-2 and B-catenin mRNA, promoting apoptosis through caspase 3 activation and inhibiting the proliferation of cells 455. Capsaicin Mediates Cell Cycle Arrest and Apoptosis in Human Colon Cancer Cells via Stabilizing and Activating p53 475, 476. Low concentration capsaicin promotes CRC cell migration and invasion by triggering production of ROS 477. | |
| Colchicum autumnale (meadow saffron) or Gloriosa superba (glory lily) | Seeds and bulbs | Colchicine | The cellular uptake and apoptotic efficiency of colchicine is correlated with downregulation of MMP-9 mRNA Expression in SW480 CRC cells 478. Colchicine induces apoptosis via MMP loss in HT-29 cells, ROS production, caspase-3 activation, upregulation of pro-apoptotic Bax, downregulation of anti-apoptotic Bcl-2 and phosphorylation of p38, which indicates an involvement of p38-regulated intrinsic apoptosis pathway 479, 480. | |
| Vitis vinifera(Grape) | Seed | Resveratrol | Resveratrol was found to upregulate miR-96 in a genetically engineered mouse model for sporadic CRC, which caused the downregulation of KRAS, an oncogene associated with tumor aggressiveness and chemoresistance 481. Upregulation of miR-101b and miR-455, which in turn led to decreased levels of IL-6 and TNF-α; these are pro-inflammatory proteins known to be promoters of colon cancer 482, 483. Additionally, a combination of resveratrol and grape seed extract has been reported to suppress Wnt/β-catenin signaling and increase mitochondria-dependent apoptosis in in vitro and in vivo models 484. Finally, resveratrol has been shown to increase miR-34a levels in DLD-1 and SW480 cells 485. | |
| Allium cepa(Red onion) | Bulb | Quercetin** | Cytotoxic activity of Quercetin on two human colonic cancer cell lines, HT29 and HCT15, depends on COX-2 dependent ROS generation that induces apoptosis and inhibits cell survival 486. In HT-29 colon cancer cells quercetin treatment decreases cell viability, arrests the cell cycle at the G1 phase and induces apoptosis, also Decreases the expression of CSN6, a subunit of the constitutive photomorphogenesis 9 multiprotein complex 487. Additionally, treatment of HT-29 cells with quercetin upregulates AMP-activated protein kinase, a physiological cellular energy sensor, which markedly suppresses cell proliferation 488. Quercetin has also been demonstrated to suppress the Wnt/β-catenin and NF-κB pathways in CRC cells 489, 490. | |
| Elettaria cardamomum | Bark | Cardamonin (Figure 8g) | Induction of apoptosis, cell cycle arrest, ROS generation, downregulation of MAPK signaling, induction of Bax translocation and loss of mitochondrial integrity were the mechanisms behind the anti-proliferative effect of cardamonin in human CRC cell lines. Also, activation of both p38 and JNK and in presence of ROS scavenger the activation was attenuated 491. Suppression of β-catenin dependent gene expression in human CRC cell lines 492. Cardamonin reduces chemotherapy resistance of colon cancer cells via the TSP50/NFκB pathway in vitro 493. | |
| Tripterygium wilfordii Hook F (Mandarin) | Root | Celastrol (Figure 8h) | Inhibit the growth, adhesion, and metastasis of human CRC cells through the inhibition of TGF-β1/Smad signaling 493. Suppression of the expression of key genes (TYMP, CDH5, THBS2, LEP, MMP9, and TNF) and proteins (IL-1b, MMP-9, PDGF, Serpin E1, and TIMP-4) involved in the angiogenesis pathway 495. Reduces the cell size of the SP (side population) increases frequency of apoptosis and binds to Pgp protein in cell membranes inhibiting its transport function 496. Inhibits CRC cell proliferation and migration through suppression of MMP3 and MMP7 by the PI3K/AKT signaling pathway 497. Effectively inhibited SW480 CRC cell proliferation, down-regulation of Shoc2 expression also significantly inhibited proliferation, colony formation, and migration functions of tumor cells 498. | |
| Mundulea sericea | Bark, roots, and leaves | Deguelin (Figure 8i) (Rotenoid, flavonoid) | Deguelin inhibited CRC cell growth by inducing apoptosis via activation of p38 MAPK pathway 499. Promoted cell cycle arrest at G0/G1 phase in colon cancer cells 500. Deguelin has been found to regulate cell cycle in colon cancer cells by stimulating p27 expression. Cyclin D1 and cyclin E is dramatically downregulated with treatment of deguelin 501. Deguelin exerted anticancer activity of human gastric cancer MGC-803 and MKN-45 cells in vitro 502. | |
| Trigonellafoenum graecum (Fenugreek) | Seed | Diosgenin (Figure 8j)(phytosteroid sapogenin) | Diosgenin induces apoptosis due to HMG (3-hydroxy-3-methylglutaryl) CoA suppression in human colon carcinoma cells 503. Diosgenin induced apoptosis in colorectal cancer cell lines HCT-116 and HT-29 504. HT-29 is sensitized by diosgenin to TRAIL induced apoptosis 505. Acts on colon carcinoma (HCT-15) cells, induces apoptosis via mitochondrial dependent pathway 506. | |
| Darmera peltate (Indian Rhubarb) andRheum palmatum (Chinese Rhubarb) | Bark and roots | Emodin (Figure 8k) (Trihydroxy-anthraquinone) | Inhibited the invasion and migration abilities of RKO cells and decreased the expression of MMP-7, MMP-9, and suppressed the growth of colorectal cancer cells by inhibiting VEGFR2 507, 508, decreased viability of CoCa cells and induced apoptosis in a time and dose-dependent manner, down regulated Bcl-2 family expression 509. Mitochondrial dysfunction and ROS accumulation in colon cancer cells also reported 510. | |
| Embeliaribes (White-flowered Embelia) | Fruit | Embelin (Figure 8l) | In tumor milieu, embelin increased the infiltration of CD8+ T cells, NK cells and mature dendritic cells whilst depleted the regulatory T cells. Moreover, embelin could directly interfere with the generation and function of MDSCs in vitro 511. In colon cancer cells, embelin diminished both the constitutive and IL-6-induced STAT3 activation by stimulating Src homology domain 2-containing protein tyrosine phosphatase (SHP2) activity 512. Embelin potently inhibited NF-κB signaling in macrophages and decreased the production of key pro-inflammatory cytokines and tumorigenic factors involved in CAC, such as TNFα, IL-6 and COX-2 513. | |
Aloe-emodin, a natural compound extract from Aloe Vera, has been discovered to suppress cell proliferation and accelerate apoptosis in a variety of tumor cells 514. Camptothecin induces the upregulation of Programmed Death-Ligand 1(PD-L1) and other cytokines that modulate the attraction, migration, and functions of immune cells, primarily T-cells 515. Scutellarin (Figure 8m) is a flavonoid isolated from a medicinal herb Scutellariabarbata(Figure 9a), downregulates the anti-apoptotic protein Bcl-2 and induces apoptosis by activating p53, which upregulates Bax to activate caspase 3 via the mitochondrial pathway 516. Treatment of HT-29 cells with luteolin (flavonoid, exist in fruits, vegetables and medicinal herbs) results in a loss of the mitochondrial membrane potential, an increase in mitochondrial Ca2+ level, upregulation of Bax, downregulation of Bcl-2, release of cytochrome c from the mitochondria to the cytosol and an increase in the levels of the active forms of caspase-9 and caspase-3 517. Treatment of Caco-2 CRC cells with extra virgin olive oil (rich in hydroxytyrosol and oleuropein) miR-23a and miR-301a, which were predicted to target type 1 cannabinoid receptor (CB1) in colon cancer 518, important implications in chemoprevention. Gambogic acid (Figure 8n), a xanthonoid extracted from the resin of Garcinia hanburyi (Figure 9b) inhibits HT-29 proliferation via induction of apoptosis 519. Walnuts (genus Juglans) have been shown to suppress colon cancer in mice models through the decreased expression of miR-1903, miR-467c, and miR-3068, as well as the increased expression of miR-297a in athymic nude mice injected subcutaneously with HT-29 CRC cells 520. Also, Aggarwal et.al, 2013 listed phytochemicals like garcinol, gossypol, gossypin, guggulsterone, indole-3-carbinol, morin, naphthoquinone, nimbolide, noscapine, oleandrin, piperine, piceatannol, pinitol, plumbagin, pomegranate, retnoids, honokiol, sesamin, silymarin, simvastatin, terpenoid, thymoquinone, tocotrienol, triptolide, ursolic acid, withanolides, xanthohumol, and zerumbone 458 having potentials in CRC. Seaweeds like U. pinnatifida175, 401, 521, 522, 523, 524, 525, 526, 527, Saccharina latissimi (9c) 528, Fucusvesiculosus176, 295, 529, 530, Sargassum hemiphyllum (Figure 9d) 531, 532, 533 have proven efficacy in this situation. Also, Algae derived astaxanthin 534, 535, 536, 537, 538, 539, 540, fucoxanthin 541, 542, 543, 544, 545, lutein and zeaxanthin 546, 547, 548, 549, polyphenols 550, 551, 552, 553, 554 shown individual excellence.
Figure 8.Plant derived biomolecules studied in colorectal cancer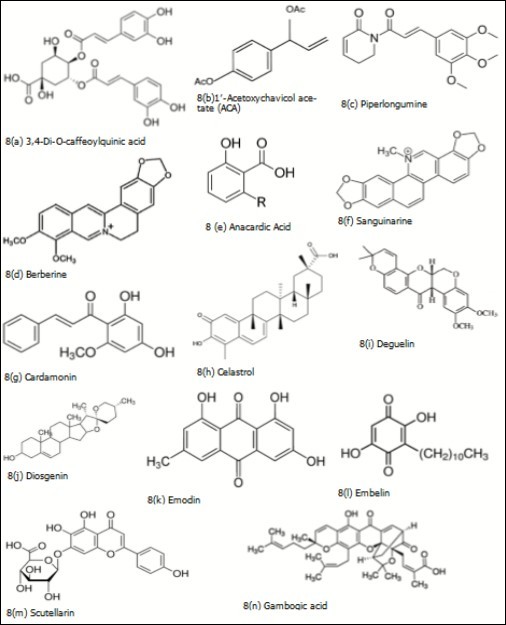
Figure 9(a).Scutellaria barbata (Source: Strictly Medicinal Seeds)
Figure9(b).Garcinia hanburyi (Source: Vitamin Supplement Ingredients Information)
Figure 9(c).Saccharina latissimi (Source: Nature Picture Library Print Store)
Figure 9(d).Sargassum hemiphyllum (Source: natural-history.main.jp)
Other Bioactive Non-Plant Compounds
Caffeic acid phenethyl ester (Figure 10a) is a central active component of propolis from honeybee hives. Propolis is a well-known health supplement that is extremely popular in Australia and New Zealand. It is constantly marketed in Japan with sales exceeding US$300 million/year 555. It can impart strong antimitogenic activity in lung cancer, breast cancer 556 and apoptosis in colon cancer 557. Peripheral neuropathy is a common side effect of many chemotherapeutic agents including paclitaxel. Poor nutritional status and obesity increase the risk of paclitaxel induced neuropathy 558. PEGylated liposomes of paclitaxel were successfully developed and demonstrated reduced neurotoxicity in-vitro in neuronal cells and prevented development of peripheral neuropathy in-vivo 559. Glutathione 560 and gallic acid 561 may ameliorate paclitaxel-induced neuropathic pain. Di(2-ethylhexyl) phthalate (DEHP) (Figure 10b), estrogen receptor alpha (ERα) agonist due to its ability to interact with ERα and promote the cell proliferation of ERα-positive breast cancer cells, significantly protected MCF-7 cells against the genotoxicity of camptothecin 562. Actinomycin D obtained from various Streptomyces strains decreases Mcl-1 expression in lung cancer cells 563, induces p53-independent cell death in leukemia 564, synergistically suppressed multiple metastasis of TRAIL-resistant colon cancer in the liver with soluble TRAIL gene 565. Hyperthermic intraperitoneal chemotherapy (HIPEC) with cisplatin and mitomycin C (Figure 10c) (obtained from Streptomyces caespitosus) is the only protocol to demonstrate an adjuvant HIPEC benefit in colorectal cancer patients at high risk for peritoneal failure and an alternative to high-dose and short-term oxaliplatin 566. 5-FU plus mitomycin remains the preferred chemotherapy in most patients with anal cancer 567. Bleomycin (Figure 10e) is an antibiotic complex of several glycopeptides derived from Streptomyces verticillus, gained FDA approval in July 1973. The extract from Streptomyces sp. MUM265- represents a valuable bioresource of bioactive compounds for the future development of chemo-preventive agents, with particular promise suggested for treatment of colon cancer 568. Bleomycin is an indispensable antineoplastic agent for the treatment of germ cell tumors and lymphomas. Pirfenidone (Figure 10d) (novel orally available antifibrotic drug approved by the FDA in 2014) is currently the only approved therapy for idiopathic pulmonary fibrosis (IPF), considered as a salvage drug for refractory cases of bleomycin-induced lung injury 569. In a similar study, Yu et.al, 2019 reported EZY-1 (16-amino-acid peptide was isolated from Eucheuma) can inhibit the IPF induced by bleomycin 570.
Figure 10.Biomolecules from non-plant origin studied or used in different types cancers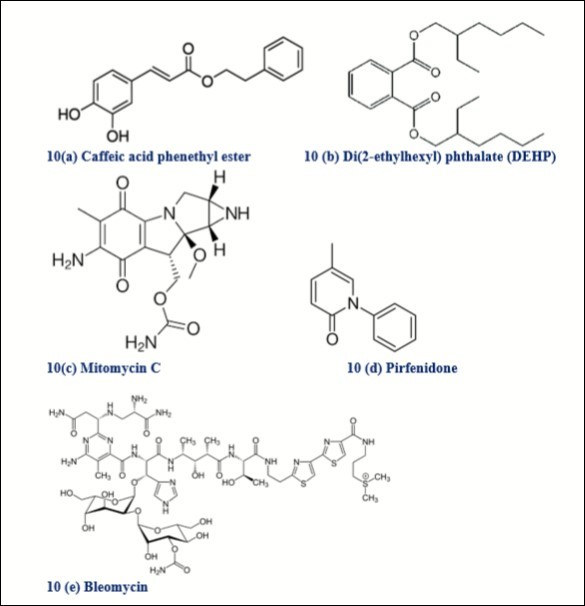
Alternative Therapies and Mind-Body Interventions
According to the Global Health Observatory Report from the WHO, insufficient physical activity is the 4th leading risk factor for mortality. Participation in 150 minutes of moderate physical activity a week or its equivalent is estimated to reduce risk of breast and colon cancer by 21%–25% 571. Approximately 50% of all leukemia, lymphoma, colorectal- and breast cancer patients are affected by CIPN. Sensorimotor training (SMT) or whole-body vibration (WBV) can reduce the symptoms of CIPN and attenuate motor and sensory deficits 572. Hypnosis, music (Figure 11) and relaxing video reduced anxiety and pain associated with colonoscopy and need for sedation during colon cancer screening 573, 574, 575, 576, 577, 578, 579, 580, 581. Impaired cognitive function, change in brain metabolism and change in brain structure are associated with cancer treatment. CBT moderately improved anxiety and depression in patients with early-stage breast cancer 582, significantly improved tumor associated fatigue levels after 8 weeks 583, improved QoL 584, improved cognitive function 585, improved insomnia 586, 587, reduced fear of cancer recurrence 588 and most importantly, reduced pain and distress 589. Mindfulness-based approaches and hypnosis reduced demonstrated efficacy in reducing anxiety and depressive symptoms. 40% to 50% CRC patients reported fear of cancer recurrence, tends to increase around the time of scans or other testing for recurrence 590. Also, CRC patients have unique psychosocial needs (e.g., isolation, embarrassment) related to altered eating and bowel habits and sexual dysfunction that warrant clinical attention 591. Acceptance and commitment therapy, meta-cognitive therapy, and mindfulness-based therapies emphasize mindfulness, acceptance, cognitive flexibility, and patient values changes in self-efficacy or confidence in using coping skills targeted by the intervention, acceptance of unwanted thoughts and feelings, or enhanced social support as well as physiological mechanisms (e.g., decreased arousal to negative thoughts and feelings about cancer) 592. Combined CBT/GET improves fatigue and functional outcomes for a subset of patients with post-cancer fatigue in breast or colon cancer 593. CBT intervention has the potential to ease acute anxiety during the often-challenging re-entry phase and to prevent the development of chronic, debilitating, and costly anxiety 594. Physical activity interventions also reduce depressive and anxiety symptoms in breast cancer survivors 595. Telehealth approaches may improve access to mental health resources especially for those with limited online access or lack of online skill 596. Yoga has a solid effect on cancer-related fatigue in patients with breast cancer 597. It is one of the most prevalent complementary therapies used in breast cancer care, seems to be as effective as other exercise modalities for improving the QoL of women with breast cancer 598. Wei et.al, 2019 reported significant improvement in lymphedema status, range of shoulder motion and spinal mobility after an 8-week yoga intervention 599. Although, yoga could not improve HRQoL in patients with colorectal cancer 600 but research supports that yoga is a promising intervention for reducing fatigue and sleep disturbances in this patient group 601.
Figure 11.Music Therapy: Pain or Distress Management 619. In the UK, music therapists are trained to master’s level and are registered with Health and Care Professions Council as allied health professionals. Aristotle recognized the innate ability of melodies to surpass “feelings such as pity and fear, or enthusiasm,” and thus “heal and purify the soul.” The Greeks identified Apollo as the father of both healing and music, alongside his many other accolades (as God of light, sun, truth, prophecy, plague and poetry).
Dyadic yoga may offer effective relaxation techniques for lung cancer patients and their caregivers who were undergoing an extreme stressor in addition to the cancer experience 602, feasible and beneficial for patients having toxic thoracic radiography 603. Approximately 20% of breast cancer survivors develop breast cancer-related lymphedema (BCRL) 604. Acupuncture is safe and effective at reducing breast cancer-related lymphoedema in patients after breast cancer treatment 605 and managing joint stiffness. Acupuncture use among breast cancer patients in the US is currently as high as 16% to 63% 606. At the current time breast cancer related lymphedema is incurable but well manageable by a number of physical therapy modalities, especially complete decongestive therapy (CDT) 607. Obesity is a factor that deteriorates the CDT efficacy. Early treatment, before developing fat accumulation and fibrosis, must be primary goal in the treatment of BCRL 608. The first “intensive treatment” phase aims to decongest the swollen arm through two or more weeks of daily therapist-delivered treatment including multi-layer compression bandaging and manual lymph drainage (MLD). This is followed by a “maintenance” phase of patient self-treatment, with compression usually in the form of hosiery 609. The mindfulness component may enhance the positive impact of exercise on cognitive function in breast cancer 610, 611. Tai Chi is accessible to most people and does not require special facilities or expensive equipment 612. Healthier dietary choices were the most frequently reported change already made by people affected by CRC, followed by increased physical activity, stress management, quitting smoking and alcohol and therapies including meditation, tai chi, and naturopathy 613. Greater shoulder muscular strength was significantly associated with better functional well-being in breast cancer survivors with TC Qigong training 614. Massage with or without aromatherapy have been suggested by a few studies in breast cancer to ameliorate anxiety and other symptom relief 615 and immunologic state 616 that needs further investigation. TENS was found valuable in lung cancer patient underwent standard posterolateral thoracotomy 617. Animal-assisted activities (Figure 12) has potential benefit children with cancer because pediatric oncology patients often suffer from distress due to physical examinations, venipuncture, chemotherapy infusions, spinal taps, surgery, hospitalization, pain, fear of medical procedures, unpleasant physical symptoms, uncertainty, and worry about death 618.
Figure 12.Hospitalized kid on animal visit 620. Understanding whether AAA is safe and effective for pediatric cancer patients is critical, especially because of concern about infection in immunosuppressed persons. Conducting AAA research in pediatric oncology requires understanding current regulations and variations in practice. Knowledge of regulations helps us understand elements required for intervention protocols (e.g., hand-cleaning), whereas knowledge of practice variation can help us identify research opportunities.
Conclusion
The journey from diagnosis to treatment of cancer affects the patients' lives in a variety of ways. Debilitating symptoms arising both due to disease and its treatments consistently hamper their QoLs. CAM treatment aims to restore body’s ability to protect, regulate and heal itself. Since almost 50% of existing medicine is derived from plants, it is clear that natural sources, especially plants can be investigated for effective medicines in cancer treatment. These data can equip providers and patients with the information they need to have informed conversations regarding non-drug approaches for treatment of specific cancer conditions. The use of CAM by cancer patients is becoming widespread. This is a reflection of the many needs and concerns that are currently not being met by conventional medical practice. Significant proportions of cancer patients in developed countries use complementary therapies as adjuncts to conventional symptom management to improve their QoL. India’s indigenous systems of medicine, such as Ayurveda, Siddha, and Unani, are more than 5,000 years old, and in rural areas, the Indian population has relied heavily on these practices, particularly Ayurveda. In addition, CAM has the potential for the primary and secondary prevention of cancer through counselling on healthy lifestyle, nutrition and supporting the human power of ‘salutogenesis’ throughout life. The lack of communication about CAM use may be due to fear of a negative response, physicians being perceived as not supportive nor helpful, or physicians and patients having differing views about CAM. Discussions of CAM therapies may have additional benefits for the patient-provider relationship, as studies have shown it indicates use of participatory decision-making, patient-centered communication, and thus greater patient satisfaction, not only in cancer care but also in other arenas of healthcare.
Financial Disclosure or Funding
N/A
Informed Consent
N/A
Author contributions
N/A
Acknowledgements
I’m thankful to Dr. Alexandra McCarthy, The University of Auckland, New Zealand for her valuable time to audit my paper and for her thoughtful suggestions. I’m also grateful to seminar library of Faculty of Pharmacy, University of Dhaka and BANSDOC Library, Bangladesh for providing me books, journal and newsletters.
Abbreviations
Mortality and Prevalence (GLOBOCAN)
Chronic Myeloid Leukemia (CML) Leukemia & Lymphoma Society (LLS) cleaved Poly (ADP-ribose) Polymerase (c-PARP) Immunogenic Cell Death (ICD) Tyrosine Kinase Inhibitors (TKI) Bruton Tyrosine Kinase (BTK) Glycogen Synthase Kinase-3β (GSK3β) Myeloid cell leukemia-1 (Mcl-1) 'Tamm-Horsfall Protein 1' (THP-1) mammalian target of rapamycin (mTOR) Src-Homology 2-Containing Inositol-5-Phosphatase 2 (SHIP2) Phosphatase and Tensin homolog (PTEN) Plant Homeodomain Finger 6 (PHF6) T-cell acute lymphoblastic leukemia (T-ALL) NADPH Quinone Dehydrogenase 1 (NQO1) Nuclear factor erythroid 2-related factor 2 (Nrf2) Rb tumor suppressor protein (pRb) c-Jun NH2-terminal kinase (JNK) Human Leukocyte Antigen (HLA) Epigallocatechin Gallate (EGCG) BReast CAncer gene-1 (BRCA-1) Chemotherapy-induced peripheral neuropathy (CIPN) Sensorimotor Training (SMT) Whole Body Vibration (WBV) Neoadjuvant Chemotherapy (NCT) Di(2-ethylhexyl)phthalate (DEHP) Programmed Death-Ligand 1(PD-L1) cyclin-dependent kinase inhibitor 1A gene (CDKN1A) Transcription Factor AP-2α (TFAP2A) Serine-threonine kinase receptor-associated protein (STRAP) Maternal embryonic leucine zipper kinase (MELK) COP9 signalosome subunit 6 (CSN6) TNF-related apoptosis-inducing ligand (TRAIL) Idiopathic Pulmonary Fibrosis (IPF) Graded Exercise Therapy (GET) Manual Lymph Drainage (MLD) Transcutaneous electrical nerve stimulation (TENS) Animal-Assisted Activities (AAA)References
- 1.Ducharme J. (2019) A Third of People with Cancer Use Alternative Medicine. Here's Why That Could Be Dangerous. Time Magazine.
- 2.Integrative PDQ. (2018) Alternative, and Complementary Therapies Editorial Board. Topics in Integrative, Alternative, and Complementary Therapies (PDQ®): Patient Version. PDQ Cancer Information Summaries [Internet]. Bethesda (MD): National Cancer Institute (US); Available from: https://www.ncbi.nlm.nih.gov/books/NBK131880/ .
- 3.Siegel R L, Miller K D, statistics Jemal A Cancer. (2019) . Jan;69(1): 7-34. doi: 10.3322/caac.21551. Epub 2019 Jan 8. PubMed PMID: , CA Cancer 30620402.
- 4.Shah S C, Kayamba V, Peek RM Jr, Heimburger D. (2019) Cancer Control in Low- and Middle-Income Countries: Is It Time to Consider Screening? J Glob Oncol. Mar;5: 1-8. doi: 10.1200/JGO.18.00200. PubMed PMID: 30908147; PubMed Central PMCID: PMC6452918 .
- 5.Ferlay J, Colombet M, Soerjomataram I, Mathers C, Parkin D M et al. (2019) Estimating the global cancer incidence and mortality in 2018: GLOBOCAN sources and methods. 10.1002/ijc.31937. Epub 2018 Dec 6. PubMed PMID: , Int 144(8), 1941-1953.
- 6.Feng R M, Zong Y N, Cao S M, Xu R H. (2019) Current cancer situation in China: good or bad news from the 2018 Global Cancer Statistics? Cancer Commun (Lond). PubMed PMID: 31030667; PubMed Central PMCID: PMC6487510 39(1), 22-10.
- 7.WHO. (2018) Latest global cancer data: Cancer burden rises to 18. 1 million new cases and 9. 6 million cancer deaths in 2018. Presse Release. Available From: https://www.who.int/cancer/PRGlobocanFinal.pdf
- 8.Li M, Chen Z, Liu Z, Zhang N, Liu J et al. (2019) Twelve Chinese herbal preparations for the treatment of depression or depressive symptoms in cancer patients: a systematic review and meta-analysis of randomized controlled trials. BMC Complement Altern Med. PubMed PMID: 30674300; PubMed Central PMCID: PMC6345004 19(28), 1-16.
- 9.Schüz J, Espina C, Wild C P. (2019) Primary prevention: a need for concerted action. Mol Oncol. 18. Review. PubMed PMID: 30582778; PubMed Central PMCID: PMC6396360 13(3), 567-578.
- 10.Cancer American. (2018) Society. Cancer Facts & Figures. Available From:https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/annual-cancer-facts-and-figures/2018/cancer-facts-and-figures-2018.pdf
- 11.Fitzmaurice C, Allen C, Barber R M, Barregard L, Bhutta Z A et al. (2017) Global Burden of Disease Cancer Collaboration, Global, Regional, and National Cancer Incidence, Mortality, Years of Life Lost, Years Lived With Disability, and Disability-Adjusted Life-years for 32 Cancer Groups. 3(4), 524-548.
- 12.Cancer WHO. (2018) . Available from: https://www.who.int/news-room/fact-sheets/detail/cancer , Health Topics 12.
- 14.Bray F, Ferlay J, Soerjomataram I, Siegel R L, Torre L A et al. (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. Nov;68(6): 394-424. doi: 10.3322/caac.21492. Epub 2018 Sep 12. PubMed PMID: , CA Cancer 30207593.
- 15.Rawla P, Barsouk A.Epidemiology of gastric cancer: global trends, risk factors and prevention. Epub 2018 Nov 28. Review. PubMed PMID: 30944675; PubMed Central PMCID: PMC6444111 , Prz Gastroenterol 14(1), 26-38.
- 16.Rawla P, Sunkara T, Gaduputi V. (2019) Epidemiology of Pancreatic Cancer: Global Trends, Etiology and Risk Factors. Feb;10(1): 10-27. doi: 10.14740/wjon1166. Epub 2019 Feb 26. Review. PubMed PMID: 30834048; PubMed Central PMCID: PMC6396775 .
- 17.Moradi A, Zamani M, Moudi E. (2019) A systematic review and meta-analysis on incidence of prostate cancer in Iran. Health Promot Perspect. 10.15171/hpp.2019.13. eCollection 2019. Review. PubMed PMID: 31249795; PubMed Central PMCID: PMC6588804 9(2), 92-98.
- 18.Rawla P. (2019) Epidemiology of Prostate Cancer. Apr;10(2): 63-89. doi: 10.14740/wjon1191. Epub 2019 Apr 20. Review. PubMed PMID: 31068988; PubMed Central PMCID: PMC6497009 .
- 19.Waks A G, Winer E P. (2019) Breast Cancer Treatment: A Review. 10.1001/jama.2018.19323. Review. PubMed PMID: , JAMA 321(3), 288-300.
- 20.Malvezzi M, Carioli G, Bertuccio P, Boffetta P, Levi F et al. (2019) European cancer mortality predictions for the year 2019 with focus on breast cancer. Ann Oncol. 10.1093/annonc/mdz051. PubMed PMID: 30(5), 781-787.
- 21.Miller K D, Nogueira L, Mariotto A B, Rowland J H, Yabroff K R et al. (2019) Cancer treatment and survivorship statistics. , CA Cancer 31184787.
- 22.DeSantis C E, Miller K D, Goding Sauer A, Jemal A, Siegel R L. (2019) Cancer statistics for African Americans. May;69(3): 211-233. doi: 10.3322/caac.21555. Epub 2019 Feb 14. PubMed PMID: , CA Cancer 30762872.
- 23.Layne T M, Graubard B I, Ma X, Mayne S T, Albanes D. (2019) Prostate cancer risk factors in black and white men in the NIH-AARP Diet and Health Study. Prostate Cancer Prostatic Dis. 22(1), 91-100.
- 24.Ghose S, Radhakrishnan V, Bhattacharya S.Ethics of cancer care: beyond biology and medicine. Ecancermedicalscience. 2019 Mar 28;13: 911. doi: 10.3332/ecancer.2019.911. eCollection 2019. Review. PubMed PMID: 31123494; PubMed Central PMCID: PMC6467456 .
- 25.Allcott N, Dunham L, Levy D, Carr J, Stitzenberg K. (2019) Financial burden amongst cancer patients treated with curative intent surgery alone. doi: 10.1016/j.amjsurg.2019.01.033. (Epub ahead of print) PubMed PMID: , Am 218(3), 452-456.
- 26.Coumoundouros C, Ould Brahim L, Lambert S D, McCusker J. (2019) The direct and indirect financial costs of informal cancer care: A scoping review. Health Soc Care Community. 31293013.
- 27.WHO. (2018) 46 billion in productivity lost to cancer in major emerging economies.Presse Release. Available From: https://www.iarc.fr/wp-content/uploads/2018/07/pr255_E.pdf 31.
- 29.Screening PDQ, Prevention Editorial Board. (2019) Cancer Prevention Overview (PDQ®): Health Professional Version. PDQ Cancer Information Summaries [Internet]. Bethesda (MD): National Cancer Institute (US); Available from: https://www.ncbi.nlm.nih.gov/books/NBK66016/ .
- 30.Sung H, Siegel R L, Rosenberg P S, Jemal A. (2019) Emerging cancer trends among young adults in the USA: analysis of a population-based cancer registry. Lancet Public Health. Epub 2019 Feb 4. PubMed PMID: 4(3), 137-147.
- 31.Park B, You S, WCS Cho, Choi J Y, Lee M S. (2019) A systematic review of herbal medicines for the treatment of cancer cachexia in animal models. Jan.;20(1): 9-22. doi: 10.1631/jzus.B1800171. Review. PubMed PMID: 30614226; PubMed Central PMCID: PMC6331334 , J Zhejiang Univ Sci.
- 32.Zhang Q. (2015) Traditional and Complementary Medicine in Primary Health Care. Health For All:The Journey of Universal Health Coverage. Hyderabad (IN): Orient Blackswan. Chapter 12. Available from: https://www.ncbi.nlm.nih.gov/books/NBK316267/ In: Medcalf A, Bhattacharya S, Momen H, et al, editors .
- 33.Mawoza T, Nhachi C, Magwali T. (2019) Prevalence of Traditional Medicine Use during Pregnancy, at Labour and for Postpartum Care in a Rural Area in Zimbabwe. Clinics in mother and child health. 16(2), 321-10.
- 34.Krupa J, Sureshkumar J, Silambarasan R, Priyadarshini K, Ayyanar M. (2019) Integration of traditional herbal medicines among the indigenous communities in Thiruvarur District of Tamil Nadu. , India. Journal of Ayurveda and integrative medicine 10(1), 32-37.
- 35.Wode K, Henriksson R, Sharp L, Stoltenberg A, Hök Nordberg J. (2019) Cancer patients' use of complementary and alternative medicine in Sweden: a cross-sectional study. BMC Complement Altern Med. PubMed PMID: 30866916; PubMed Central PMCID: PMC6417272 19(1), 62-10.
- 36.Jermini M, Dubois J, Rodondi P Y, Zaman K, Buclin T et al. (2019) Complementary medicine use during cancer treatment and potential herb-drug interactions from a cross-sectional study in an academic centre. Sci Rep. PubMed PMID: 30911084; PubMed Central PMCID: PMC6434040 9(1), 1-11.
- 37.Kwon J H, Lee S C, Lee M A, Kim Y J, Kang J H et al.. Behaviors and Attitudes toward the Use of Complementary and Alternative Medicine among Korean Cancer Patients. Cancer Res Treat. 2019 Jul;51(3): 851-860. doi: 10.4143/crt.2019.137. Epub 2019 Jun 7. PubMed PMID: 31208165; PubMed Central PMCID: PMC6639220 .
- 38.Jones E, Nissen L, McCarthy A, Steadman K, Windsor C. (2019) Exploring the Use of Complementary and Alternative Medicine in Cancer Patients. Integr Cancer Ther. Jan-Dec;18: 1534735419854134. doi: 10.1177/1534735419854134. PubMed PMID: 31170844; PubMed Central PMCID: PMC6557018 .
- 39.Chotipanich A, Sooksrisawat C, Jittiworapan B. (2019) Association between complementary and alternative medicine use and prolonged time to conventional treatment among Thai cancer patients in a tertiary-care hospital. PeerJ. 14;7:e7159. doi: 10.7717/peerj.7159. eCollection 2019. PubMed PMID: 31231600; PubMed Central PMCID: PMC6573806 .
- 40.Ekor M. (2014) The growing use of herbal medicines: issues relating to adverse reactions and challenges in monitoring safety. Front Pharmacol. 10;4: 177. doi: 10.3389/fphar.2013.00177. eCollection 2014 Jan 10. Review. PubMed PMID: 24454289; PubMed Central PMCID: PMC3887317 .
- 41.Haefeli W E, Carls A. (2014) Drug interactions with phytotherapeutics in oncology. Expert Opin Drug Metab Toxicol. Epub 2014 Jan 6. Review. PubMed PMID: 10(3), 359-77.
- 43.Caraceni A, Shkodra M. (2019) Cancer Pain Assessment and Classification. Cancers. E510. doi: 10.3390/cancers11040510. Review. PubMed PMID: 30974857; PubMed Central PMCID: PMC6521068 , (Basel) 11(4).
- 44.Derry S, Wiffen P J, Moore R A, McNicol E D, Bell R F et al.Oral nonsteroidal anti-inflammatory drugs (NSAIDs) for cancer pain in adults. Cochrane Database Syst Rev. 2017 Jul 12;7: CD012638. doi: 10.1002/14651858.CD012638.pub2. Review. PubMed PMID: 28700091; PubMed Central PMCID: PMC6369931 .
- 45.Bennett M I, Kaasa S, Barke A, Korwisi B, Rief W. (2019) Treede RD; IASP Taskforce for the Classification of Chronic Pain. The IASP classification of chronic pain for ICD-11: chronic cancer-related. Review. PubMed PMID: 30586069 160(1), 38-44.
- 46.Asthana R, Goodall S, Lau J, Zimmermann C, Diaz P L et al. (2019) De Angelis C. Framing of the opioid problem in cancer pain management in Canada. Curr Oncol. Jun;26(3):e410-e413. doi: 10.3747/co.26.4517. Epub 2019 Jun 1. PubMed PMID: 31285686; PubMed Central PMCID: PMC6588080 .
- 47.Johnson M, Collett B, Castro-Lopes J M. (2013) The challenges of pain management in primary care: a pan-European survey. J Pain Res. 22;6: 393-401. doi: 10.2147/JPR.S41883. Print 2013. PubMed PMID: 23723719; PubMed Central PMCID: PMC3666876 .
- 48.Jones M R, Viswanath O, Peck J, Kaye A D, Gill J S et al. (2018) A Brief History of the Opioid Epidemic and Strategies for Pain Medicine. , Pain Ther 7(1), 13-21.
- 49.Oelhaf R C, Azadfard M, Toxicity Kum B Opioid. (2019) In:StatPearls Internet. Treasure Island (FL):StatPearls Publishing;. Available from: https://www.ncbi.nlm.nih.gov/books/NBK431077/
- 50.Gallagher R. (2018) New category of opioid-related death. Can Fam Physician. Feb;64(2): 95-96. PubMed PMID: 29449232; PubMed Central PMCID: PMC5964377 .
- 51.Roland C L, Ye X, Stevens V, Oderda G M. (2019) The Prevalence and Cost of Medicare Beneficiaries Diagnosed and At Risk for Opioid Abuse, Dependence, and Poisoning. J Manag Care Spec Pharm. Jan;25(1): 18-27. doi: 10.18553/jmcp.2019.25.1.018. PubMed PMID: 30589633.
- 52.Shah M, Huecker M R. (2019) Opioid Withdrawal In: StatPearls [Internet]. Treasure Island (FL):. Available from:https://www.ncbi.nlm.nih.gov/books/NBK526012/
- 53.Magee D J, Jhanji S, Poulogiannis G, Farquhar-Smith P, MRD Brown. (2019) Nonsteroidal anti-inflammatory drugs and pain in cancer patients: a systematic review and reappraisal of the evidence. Aug;123(2):e412-e423. doi: 10.1016/j.bja.2019.02.028. Epub , Br 6676054.
- 54.RSY Wong. (2019) Role of Nonsteroidal Anti-Inflammatory Drugs (NSAIDs) in Cancer Prevention and Cancer Promotion. Adv Pharmacol Sci. eCollection 2019. Review. PubMed PMID: 30838040; PubMed Central PMCID: PMC6374867 31, 3418975-10.
- 55.Cuomo A, Bimonte S, Forte C A, Botti G, Cascella M. (2019) Multimodal approaches and tailored therapies for pain management: the trolley analgesic model. J Pain Res. 19, 711-714.
- 56.Nair A S. (2019) Cardiovascular Safety of Naproxen for Treating Cancer and Noncancer Chronic Pain. Indian J Palliat Care. Jan-Mar;25(1): 164-165. doi: 10.4103/IJPC.IJPC_143_18. PubMed PMID: 30820123; PubMed Central PMCID: PMC6388596 .
- 57.Wongrakpanich S, Wongrakpanich A, Melhado K, Rangaswami J. (2018) A Comprehensive Review of Non-Steroidal Anti-Inflammatory Drug Use in The Elderly. Aging Dis. 10.14336/AD.2017.0306. eCollection 2018 Feb. Review. PubMed PMID: 29392089; PubMed Central PMCID: PMC5772852 9(1), 143-150.
- 58.Brasky T M, Bonner M R, Moysich K B, Ambrosone C B, Nie J et al. (2011) Non-steroidal anti-inflammatory drugs (NSAIDs) and breast cancer risk: differences by molecular subtype. Cancer Causes Control. 22(7), 965-75.
- 59.Choueiri T K, Je Y, Cho E. (2014) Analgesic use and the risk of kidney cancer: a meta-analysis of epidemiologic studies. 10.1002/ijc.28093. Epub 2013 Sep 23. PubMed PMID: 23400756; PubMed Central PMCID: PMC3815746 , Int 134(2), 384-96.
- 60.Byars T, Theisen E, Bolton D L. (2019) Using Cannabis to Treat Cancer-Related Pain. Semin Oncol Nurs. Jun;35(3): 300-309. doi: 10.1016/j.soncn.2019.04.012. Epub 2019 Apr 30. Review. PubMed PMID: 31053395.
- 61.Dzierżanowski T. (2019) Prospects for the Use of Cannabinoids in Oncology and Palliative Care Practice: A Review of the Evidence. Cancers. pii: E129. doi: 10.3390/cancers11020129. Review. PubMed PMID: 30678303; PubMed Central PMCID: PMC6406915 , (Basel) 11(2).
- 62.Carr Daniel, Schatman Michael. (2019) Cannabis for Chronic Pain: Not Ready for Prime Time.”. , American Journal of Public Health 109(1), 50-51.
- 63.Sharafi G, He H, Nikfarjam M. (2019) Potential Use of Cannabinoids for the Treatment of Pancreatic Cancer. J Pancreat Cancer. 10.1089/pancan.2018.0019. eCollection 2019. Review. PubMed PMID: 30706048; PubMed Central PMCID: PMC6352507 5(1), 1-7.
- 64.Campbell G, Stockings E, Nielsen S. (2019) Understanding the evidence for medical cannabis and cannabis-based medicines for the treatment of chronic non-cancer pain. Eur Arch Psychiatry Clin Neurosci. 11. Review. PubMed PMID: 269(1), 135-144.
- 65.Stockings E, Campbell G, Hall W D, Nielsen S, Zagic D et al.Cannabis and cannabinoids for the treatment of people with chronic noncancer pain conditions: a systematic review and meta-analysis of controlled and observational studies. Pain. 2018 Oct;159(10): 1932-1954. doi: 10.1097/j.pain.0000000000001293. PubMed PMID: 29847469.
- 66.Wang J, Wang Y, Tong M, Pan H, Li D. (2019) New Prospect for Cancer Cachexia: Medical. 10.7150/jca.28246. eCollection 2019. Review. PubMed PMID: 30719170; PubMed Central PMCID: PMC6360413 10(3), 716-720.
- 67.Turgeman I, Bar-Sela G. (2019) Cannabis for cancer - illusion or the tip of an iceberg: a review of the evidence for the use of Cannabis and synthetic cannabinoids in oncology. Expert Opin Investig Drugs. Epub 2018 Dec 29. Review. PubMed PMID: 28(3), 285-296.
- 68.Urits I, Borchart M, Hasegawa M, Kochanski J, Orhurhu V et al. (2019) An Update of Current Cannabis-Based Pharmaceuticals in Pain Medicine. Pain Ther. Epub 2019 Feb 5. Review. PubMed PMID: 30721403; PubMed Central PMCID: PMC6514017 8(1), 41-51.
- 69.Lossignol D. (2019) Cannabinoids: a new approach for pain control? Curr Opin Oncol. Jul;31(4): 275-279. doi: 10.1097/CCO.0000000000000523. PubMed PMID: 30789867.
- 70.Steele G, Arneson T, Zylla D. (2019) A Comprehensive Review of Cannabis in Patients with Cancer: Availability in the USA, General Efficacy, and Safety. Curr Oncol Rep. Review. PubMed PMID: 30707319 21(1), 1-10.
- 71.Mead A. (2019) Legal and Regulatory Issues Governing Cannabis and Cannabis-Derived Products in the United States. Front Plant Sci. 14;10: 697. doi: 10.3389/fpls.2019.00697. eCollection 2019. Review. PubMed PMID: 31263468; PubMed Central PMCID: PMC6590107 .
- 72.Shi S, Brant A R, Sabolch A, Pollom E. (2019) False News of a Cannabis Cancer Cure. Cureus. doi: 10.7759/cureus.3918. PubMed PMID: 30931189; PubMed Central PMCID: PMC6426557 .
- 73.Wilkinson S T. (2013) Medical and recreational marijuana: commentary and review of the literature. Mo Med. Nov-Dec;110(6): 524-8. Review. PubMed PMID: 24564006; PubMed Central PMCID: PMC6179811 .
- 74.Boehnke K F, Gangopadhyay S, Clauw D J, Haffajee R L. (2019) Qualifying Conditions Of Medical Cannabis License Holders In The United States. Health Aff (Millwood). Feb;38(2): 295-302. doi: 10.1377/hlthaff.2018.05266. Erratum in: Health Aff (Millwood). 2019 Mar;38(3): 511. PubMed PMID: 30715980; PubMed Central PMCID: PMC6398594 .
- 75.Stuyt E. (2018) The Problem with the Current High Potency THC Marijuana from the Perspective of an Addiction Psychiatrist. Mo Med. Nov-Dec;115(6): 482-486. PubMed PMID: 30643324; PubMed Central PMCID: PMC6312155 .
- 76.Kansagara D, O'Neil M, Nugent S. (2017) Benefits and Harms of Cannabis in Chronic Pain or Post-traumatic Stress Disorder: A Systematic Review [Internet]. Washington (DC): Department of Veterans Affairs (US);. RESULTS. Available from:https://www.ncbi.nlm.nih.gov/books/NBK476452/
- 77.Pacula R L, Smart R. (2017) Medical Marijuana and Marijuana Legalization. Annu Rev Clin Psychol. Review. PubMed PMID: 28482686; PubMed Central PMCID: PMC6358421 8, 397-419.
- 78.Dariš B, Tancer Verboten M, Knez Ž, Ferk P. (2019) Cannabinoids in cancer treatment: Therapeutic potential and legislation. Bosn J Basic Med Sci. 10.17305/bjbms.2018.3532. Review. PubMed PMID: 30172249; PubMed Central PMCID: PMC6387667 19(1), 14-23.
- 79.Gonçalves J, Rosado T, Soares S, Simão A Y, Caramelo D et al. (2019) Cannabis and Its Secondary Metabolites: Their Use as Therapeutic Drugs, Toxicological Aspects, and Analytical Determination. Medicines (Basel). 10.3390/medicines6010031. Review. PubMed PMID: 30813390; PubMed Central PMCID: PMC6473697. 6(1) 31.
- 80.Cooke A C, Knight K R, Miaskowski C.Patients' and clinicians' perspectives of co-use of cannabis and opioids for chronic non-cancer pain management in primary care. Int J Drug Policy. 2019 Jan;63: 23-28. doi: 10.1016/j.drugpo.2018.09.002. Epub 2018 Nov 23. PubMed PMID: 30472467; PubMed Central PMCID: PMC6353665 .
- 81.Huang M Y, Zhang L L, Ding J, Lu J J. (2018) Anticancer drug discovery from Chinese medicinal herbs. Chin Med.13(35): 1-9. eCollection Review. PubMed PMID: 29997684; PubMed Central PMCID:. 6031194-10.
- 82.Li K, Giustini D, Seely D. (2019) A systematic review of acupuncture for chemotherapy-induced peripheral neuropathy. Curr Oncol. Apr;26(2):e147-e154. doi: 10.3747/co.26.4261. Epub 2019 Apr 1. PubMed PMID: 31043820; PubMed Central PMCID: PMC6476456 .
- 83.Chou H L, Chao T Y, Chen T C, Chu C M, Hsieh C H et al. (2019) Chemotherapy agents induce tartrate-resistant acid phosphatase 5a contributing to the symptom distress in lung cancer patients. 10.1016/j.ejphar.2019.01.011. Epub , Eur J Pharmacol 846, 38-48.
- 84.Bonhof C S, LV van de Poll-Franse, PAJ Vissers, Wasowicz D K, Wegdam J A et al. (2019) Anxiety and depression mediate the association between chemotherapy-induced peripheral neuropathy and fatigue: Results from the population-based PROFILES registry. Psychooncology. 31293046.
- 85.Chui P L. (2019) Cancer and Chemotherapy-Related Symptoms and the Use of Complementary and Alternative Medicine. 10.4103/apjon.apjon_51_18. PubMed PMID: 30599008; PubMed Central PMCID: PMC6287385 , Asia Pac J Oncol Nurs. Jan-Mar; 6(1), 4-6.
- 86.Munzone E, Bagnardi V, Campennì G, Mazzocco K, Pagan E et al. (2019) Preventing chemotherapy-induced alopecia: a prospective clinical trial on the efficacy and safety of a scalp-cooling system in early breast cancer patients treated with anthracyclines. , Br 121(4), 325-331.
- 87.Hain B A, Xu H, Wilcox J R, Mutua D, Waning D L.Chemotherapy-induced loss of bone and muscle mass in a mouse model of breast cancer bone metastases and cachexia. JCSM Rapid Commun. 2019 Jan-Jun;2(1). pii: e00075. PubMed PMID: 31032492; PubMed Central PMCID: PMC6481302 .
- 88.Dy S M, Isenberg S R, Al Hamayel NA. (2017) Palliative Care for Cancer Survivors. Med Clin North Am. Nov;101(6): 1181-1196. doi: 10.1016/j.mcna.2017.06.009. Review. PubMed PMID: 28992862; PubMed Central PMCID: PMC6467511 .
- 89.Lee Y H. (2019) Spiritual Care for Cancer Patients. Asia Pac J Oncol Nurs. Apr-Jun;6(2): 101-103. doi: 10.4103/apjon.apjon_65_18. PubMed PMID: 30931352; PubMed Central PMCID: PMC6371666 .
- 91.Mohiuddin A K.Community and Clinical Pharmacists in Transition Care. , Glob J Pharmaceu Sci 7(2), 555706-10.
- 92.Khan H, Saeedi M, Nabavi S M, Mubarak M S, Bishayee A. (2019) Glycosides from Medicinal Plants as Potential Anticancer Agents: Emerging Trends Towards Future Drugs. Review. PubMed PMID: , Curr Med Chem 26(13), 2389-2406.
- 93.Kuruppu A I, Paranagama P, Goonasekara C L. (2019) Medicinal plants commonly used against cancer in traditional medicine formulae in Sri Lanka. Saudi Pharm J. May;27(4): 565-573. doi: 10.1016/j.jsps.2019.02.004. Epub 2019 Feb 7. Review. PubMed PMID: 31061626; PubMed Central PMCID: PMC6488922 .
- 94.Tuama A A, Mohammed A A. (2019) Phytochemical screening and in vitro antibacterial and anticancer activities of the aqueous extract of Cucumis sativus. Mar;26(3): 600-604. doi: 10.1016/j.sjbs.2018.07.012. Epub 2018 Jul 31. PubMed PMID: 30899178; PubMed Central PMCID: PMC6408718 , Saudi J Biol Sci.
- 95.AML Seca, DCGA Pinto. (2018) Plant Secondary Metabolites as Anticancer Agents: Successes in Clinical Trials and Therapeutic Application. Int J Mol Sci. pii: E263. doi: 10.3390/ijms19010263. Review. PubMed PMID: 29337925; PubMed Central PMCID: PMC5796209 19(1).
- 96.Alves-Silva J M, Romane A, Efferth T, Salgueiro L North. (2017) African Medicinal Plants Traditionally Used in Cancer Therapy. Front Pharmacol. 26;8: 383. doi: 10.3389/fphar.2017.00383. eCollection 2017. Review. PubMed PMID: 28694778; PubMed Central PMCID: PMC5483438 .
- 97.Tariq A, Sadia S, Pan K, Ullah I, Mussarat S et al. (2017) A systematic review on ethnomedicines of anti-cancer plants. Phytother Res. Feb;31(2): 202-264. doi: 10.1002/ptr.5751. Epub 2017 Jan 17. Review. PubMed PMID: 28093828.
- 98.Gezici S, Şekeroğlu N.Current Perspectives in the Application of Medicinal Plants Against Cancer: Novel Therapeutic Agents. Anticancer Agents Med Chem. PubMed PMID: 19(1), 101-111.
- 99.Lichota A, Gwozdzinski K. (2018) Anticancer Activity of Natural Compounds from Plant and Marine Environment. Int J Mol Sci. 9;19(11). pii: E3533. doi: 10.3390/ijms19113533. Review. PubMed PMID: 30423952; PubMed Central PMCID: PMC6275022 .
- 100.Mushtaq S, Abbasi B H, Uzair B, Abbasi R. (2018) Natural products as reservoirs of novel therapeutic agents. EXCLI J. Review. PubMed PMID: 29805348; PubMed Central PMCID: PMC5962900 4, 420-451.
- 101.Dutt R, Garg V, Khatri N, Madan A K.Phytochemicals in Anticancer Drug Development. PubMed PMID: , Anticancer Agents Med Chem 19(2), 172-183.
- 102.Qi F, Zhao L, Zhou A, Zhang B, Li A et al. (2015) The advantages of using traditional Chinese medicine as an adjunctive therapy in the whole course of cancer treatment instead of only terminal stage of cancer. Biosci Trends. Feb;9(1): 16-34. doi: 10.5582/bst.2015.01019. Review. PubMed PMID: 25787906.
- 103.Wong W, Chen B Z, AKY Lee, AHC Chan, JCY Wu et al. (2019) Chinese Herbal Medicine Effectively Prolongs the Overall Survival of Pancreatic Cancer Patients: A Case Series. PubMed PMID: 30791742; PubMed Central PMCID: PMC6432679 , Integr Cancer Ther 18(1), 1-8.
- 104.Jiao L, Xu J, Sun J, Chen Z, Gong Y et al.. Chinese Herbal Medicine Combined With EGFR-TKI in EGFR Mutation-Positive Advanced Pulmonary Adenocarcinoma (CATLA): A Multicenter, Randomized, Double-Blind, Placebo-Controlled Trial. Front Pharmacol. 2019 Jul 2;10: 732. doi: 10.3389/fphar.2019.00732. eCollection 2019. PubMed PMID: 31333456; PubMed Central PMCID: PMC6614728 .
- 105.Shen S, Jiang S. (2019) Chinese herbal medicines of supplementing Qi and nourishing Yin combined with chemotherapy for non-small cell lung cancer: A meta-analysis and systematic review. J Cell Biochem. Jun;120(6): 8841-8848. doi: 10.1002/jcb.28192. Epub 2019 Feb 7. PubMed PMID: 30730073.
- 106.Wu J, Liu Y, Fang C, Zhao L, Lin L et al. (2019) Traditional Chinese Medicine Preparation Combined Therapy May Improve Chemotherapy Efficacy: A Systematic Review and Meta-Analysis. Evid Based Complement Alternat Med. 1-8.
- 107.Ma Z, Fan Y, Wu Y, Kebebe D, Zhang B et al. (2019) Traditional Chinese medicine-combination therapies utilizing nanotechnology-based targeted delivery systems: a new strategy for antitumor treatment. , Int J Nanomedicine. Mar22; 14, 2029-2053.
- 108.So T H, Chan S K, Lee V H, Chen B Z, Kong F M et al. (2019) Chinese Medicine in Cancer Treatment - How is it Practised in the East and the West? Clin Oncol (R Coll Radiol). Aug;31(8): 578-588. doi: 10.1016/j.clon.2019.05.016. Epub 2019 Jun 6. PubMed PMID: 31178347.
- 109.Gong Y, Xu Z, Jin C, Deng H, Wang Z et al. (2018) Treatment of Advanced Non-small-Cell Lung Cancer with Qi-Nourishing Essence-Replenishing Chinese Herbal Medicine Combined with Chemotherapy. Biol Proced Online. 20(9), 1-7.
- 110.Jiao L, Bi L, Lu Y, Wang Q, Gong Y et al. (2018) Cancer chemoprevention and therapy using chinese herbal medicine. Biol Proced Online. Review. PubMed PMID: 29321719; PubMed Central PMCID: PMC5757296 , Jan8 20(1), 1-14.
- 111.Yue G G, Lee J K, Chan B C, Kwok H F, Hoi S W et al. (2018) An innovative anti-cancer Chinese herbal formula exhibited multi-targeted efficacies in metastatic breast cancer mouse model. Chin Med. , Dec22 13(64), 1-12.
- 112.Aghajanpour M, Nazer M R, Obeidavi Z, Akbari M, Ezati P et al. (2017) Functional foods and their role in cancer prevention and health promotion: a comprehensive review. Am J Cancer Res. Review. PubMed PMID: 28469951; PubMed Central PMCID: PMC5411786 7(4), 740-769.
- 113.Volpato M, Hull M A. (2018) Omega-3 polyunsaturated fatty acids as adjuvant therapy of colorectal cancer. Cancer Metastasis Rev. Review. PubMed PMID: 29971573; PubMed Central PMCID: PMC6133177 37(23), 545-555.
- 114.Liu J, Abdelmagid S A, Pinelli C J, Monk J M, Liddle D M et al. (2018) Marine fish oil is more potent than plant-based n-3 polyunsaturated fatty acids in the prevention of mammary tumors. J Nutr Biochem. May;55: 41-52. doi: 10.1016/j.jnutbio.2017.12.011. Epub 2017 Dec 27. PubMed PMID: 29413488.
- 115.Pacheco B S, Dos Santos MAZ, Schultze E, Martins R M, Lund R G et al. (2018) De Pereira CMP. Cytotoxic Activity of Fatty Acids From Antarctic Macroalgae on the Growth of Human Breast Cancer Cells. Front Bioeng Biotechnol. , Dec3 6, 1-10.
- 116.Teas J, Vena S, Cone D L, Irhimeh M. (2013) The consumption of seaweed as a protective factor in the etiology of breast cancer: proof of principle. Jun;25(3): 771-779. Epub 2012 Nov 10. PubMed PMID: 23678231; PubMed Central PMCID: PMC3651528 , J Appl Phycol.
- 117.DHA Rocha, AML Seca, DCGA Pinto. (2018) Seaweed Secondary Metabolites In Vitro and In Vivo Anticancer Activity. Mar Drugs. pii: E410. doi: 10.3390/md16110410. Review. PubMed PMID: 30373208; PubMed Central PMCID: PMC6266495 16(11).
- 118.Shreadah M A, El Moneam NMA, Al-Assar S A, Nabil-Adam A. (2018) Phytochemical and pharmacological screening of Sargassium vulgare from Suez Canal, Egypt. Food Sci Biotechnol. 27(4), 963-979.
- 119.Shin S A, Moon S Y, Kim W Y, Paek S M, Park H H et al.Structure-Based Classification and Anti-Cancer Effects of Plant Metabolites. Int J Mol Sci. 2018 Sep 6;19(9). pii: E2651. doi: 10.3390/ijms19092651. Review. PubMed PMID: 30200668; PubMed Central PMCID: PMC6163735 .
- 120.Bernardini G, Minetti M, Polizzotto G, Biazzo M, Santucci A. (2018) Pro-Apoptotic Activity of French Polynesian Padina pavonica Extract on Human Osteosarcoma Cells. Mar Drugs. 13;16(12). pii: E504. doi: 10.3390/md16120504. PubMed PMID: 30551628; PubMed Central PMCID: PMC6316765 .
- 121.Stonik V A, Fedorov S N. (2014) Marine low molecular weight natural products as potential cancer preventive compounds. Mar Drugs. 10.3390/md12020636. Review. PubMed PMID: 24473167; PubMed Central PMCID: PMC3944507 12(2), 636-71.
- 122.Kooti W, Servatyari K, Behzadifar M, Asadi-Samani M, Sadeghi F et al. (2017) Effective Medicinal Plant in Cancer Treatment, Part 2: Review Study. Epub 2017 Mar 31. Review. PubMed PMID: 28359161; PubMed Central PMCID: PMC5871268 , J Evid Based Complementary Altern Med 22(4), 982-995.
- 123.A F Wali, Majid S, Rasool S.Natural products against cancer: Review on phytochemicals from marine sources in preventing cancer. , Saudi Pharmaceutical Journal,https://doi.org/10.1016/j.jsps.2019.04.013
- 124.Shree T J, Poompavai S, SMFM Begum, Gowrisree V, Hemalatha S. (2019) Cancer-Fighting Phytochemicals: Another Look. , J Nanomedine Biotherapeutic Discov 9(1), 1-7.
- 125.Smith R A, Andrews K S, Brooks D, Fedewa S A, Manassaram-Baptiste D et al. (2017) Cancer screening in the United States, 2017: A review of current American Cancer Society guidelines and current issues in cancer screening. Mar;67(2): 100-121. doi: 10.3322/caac.21392. Epub 2017 Feb 7. PubMed PMID: , CA Cancer 28170086.
- 126.Kim S-K, Kalimuthu S. (2014) Chapter 1. Introduction to Anti-cancer Drugs from Marine Origine. In: Se-Kwon Kim. Handbook of Anticancer Drugs from Marine Origin , ISBN 3319071459, 9783319071459.
- 127.Sun L, Yim W S, Fahey P, Wang S, Zhu X et al. (2019) Investigation on Advanced Non-Small-Cell Lung Cancer among Elderly Patients Treated with Chinese Herbal Medicine versus Chemotherapy: A Pooled Analysis of Individual Data. Evid Based Complement Alternat Med. Jan2, doi: 10.1155/2019/1898345. eCollection 2019. PubMed PMID: 30719055; PubMed Central PMCID: PMC6334362 .
- 128.Abdelaziz H M, Elzoghby A O, Helmy M W, Samaha M W, Fang J Y et al.Liquid crystalline assembly for potential combinatorial chemo-herbal drug delivery to lung cancer cells. , Int J Nanomedicine. 2019 Jan11; 14, 499-517.
- 129.Blandin Knight S, Crosbie P A, Balata H, Chudziak J, Hussell T et al. (2017) Progress and prospects of early detection in lung cancer. Open Biol. Sep;7(9). pii: 170070. doi: 10.1098/rsob.170070. Review. PubMed PMID: 28878044; PubMed Central PMCID: PMC5627048 .
- 130.Zappa C, Mousa S A. (2016) Non-small cell lung cancer: current treatment and future advances. Transl Lung Cancer Res. Jun;5(3): 288-300. doi: 10.21037/tlcr.2016.06.07. Review. PubMed PMID: 27413711; PubMed Central PMCID: PMC4931124 .
- 131.Lin C K, Lin R T, Chen T, Zigler C, Wei Y et al. (2019) A global perspective on coal-fired power plants and burden of lung cancer. Environ Health. PubMed PMID: 30691464; PubMed Central PMCID: PMC6350330 , Jan28 18(9), 1-11.
- 132.Alberg A J, Brock M V, Ford J G, Samet J M, Spivack S D.Epidemiology of lung cancer: Diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2013 May;143(5 Suppl):e1S-e29S. doi: 10.1378/chest.12-2345. Review. PubMed PMID: 23649439; PubMed Central PMCID: PMC4694610 .
- 133.Sulé-Suso J, Watson N A, van Pittius DG, Jegannathen A.Striking lung cancer response to self-administration of cannabidiol: A case report and literature review. SAGE Open Med Case Rep. 2019 Feb 21;7: 2050313X19832160. doi: 10.1177/2050313X19832160. eCollection 2019. PubMed PMID: 30815264; PubMed Central PMCID: PMC6385325 .
- 134.Myneni A A, Chang S C, Niu R, Liu L, Swanson M K et al. (2016) Raw Garlic Consumption and Lung Cancer in a Chinese Population. Cancer Epidemiol Biomarkers Prev. 25(4), 624-33.
- 135.Jin Z Y, Wu M, Han R Q, Zhang X F, Wang X S et al. (2013) Raw garlic consumption as a protective factor for lung cancer, a population-based case-control study in a Chinese population. Cancer Prev Res (Phila). 6(7), 711-8.
- 136.Lin Y, Cai L. (2012) Environmental and dietary factors and lung cancer risk among Chinese women: a case-control study in southeast China. Nutr Cancer. Epub 2012 Apr 10. PubMed PMID: 64(4), 508-14.
- 137.Mohammad P, Nosratollah Z, Mohammad R, Abbas A, Javad R. (2017) The inhibitory effect of Curcuma longa extract on telomerase activity in A549 lung cancer cell line. http://www.ajol.info/index.php/ajb/article/view/78098. Accessed , Afr J Biotechnol 9(6).
- 138.Valiahdi S M, Iranshahi M, Sahebkar A. (2013) Cytotoxic activities of phytochemicals from Ferula species. PubMed PMID: 23701832; PubMed Central PMCID: PMC3671137 , Daru, May23 21(39), 1-7.
- 139.Wu C Y, Ke Y, Zeng Y F, Zhang Y W, Yu H J. (2017) Anticancer activity of Astragalus polysaccharide in human non-small cell lung cancer cells. Cancer Cell Int. PubMed PMID: 29225515; PubMed Central PMCID: PMC5716001 , Dec4 17(115), 1-9.
- 140.Guo L, Bai S P, Zhao L, Wang X H. (2012) Astragalus polysaccharide injection integrated with vinorelbine and cisplatin for patients with advanced non-small cell lung cancer: effects on quality of life and survival. Med Oncol. 29(3), 1656-62.
- 141.McCulloch M, See C, Shu X J, Broffman M, Kramer A et al. (2006) Astragalus-based Chinese herbs and platinum-based chemotherapy for advanced non-small-cell lung cancer: meta-analysis of randomized trials. J Clin Oncol. PubMed PMID: 24(3), 419-30.
- 142.Li H, Hung A, Li M, AWH Yang.Fritillariae Thunbergii Bulbus: Traditional Uses, Phytochemistry, Pharmacodynamics, Pharmacokinetics and Toxicity. Int J Mol Sci. 2019 Apr 3;20(7). pii: E1667. doi: 10.3390/ijms20071667. Review. PubMed PMID: 30987173; PubMed Central PMCID: PMC6479889 .
- 143.Li T, Chen X, Chen X, Ma D L, Leung C H et al. (2016) Platycodin D potentiates proliferation inhibition and apoptosis induction upon AKT inhibition via feedback blockade in non-small cell lung cancer cells. Sci Rep. 29;6: 37997. doi: 10.1038/srep37997. PubMed PMID: 27897231; PubMed Central PMCID: PMC5126555 .
- 144.Yim N H, Hwang Y H, Liang C, Ma J Y.A platycoside-rich fraction from the root of Platycodon grandiflorum enhances cell death in A549 human lung carcinoma cells via mainly AMPK/mTOR/AKT signal-mediated autophagy induction. J Ethnopharmacol. 2016 Dec 24;194: 1060-1068. doi: 10.1016/j.jep.2016.10.078. Epub 2016 Oct 27. PubMed PMID: 27989873.
- 145.Platycodin D. (2019) a bioactive component of Platycodon grandiflorum, induces cancer cell death associated with extreme vacuolation. Anim Cells Syst (Seoul). 23(2), 118-127.
- 146.Huang M Y, Jiang X M, Xu Y L, Yuan L W, Chen Y C et al. (2019) Platycodin D triggers the extracellular release of programed death Ligand-1 in lung cancer cells. Food Chem Toxicol. Sep;131: 110537. doi: 10.1016/j.fct.2019.05.045. Epub 31150782.
- 147.Lee C T, Huang Y W, Yang C H, Huang K S.Drug delivery systems and combination therapy by using vinca alkaloids. Review. PubMed PMID: 25877096; PubMed Central PMCID: PMC4997956 , Curr Top Med Chem 15(15), 1491-500.
- 148.Zhang Y, Yang S H, Guo X L. (2017) New insights into Vinca alkaloids resistance mechanism and circumvention in lung cancer. Biomed Pharmacother. Dec;96: 659-666. doi: 10.1016/j.biopha.2017.10.041. Epub 2017 Nov 6. Review. PubMed PMID: 29035832.
- 149.Tagliamento M, Genova C, Rossi G, Coco S, Rijavec E et al. (2019) Microtubule-targeting agents in the treatment of non-small cell lung cancer: insights on new combination strategies and investigational compounds. Expert Opin Investig Drugs. Epub 2019 Jun 7. Review. PubMed PMID: 28(6), 513-523.
- 150.Gusella M, Pasini F, Caruso D, Barile C, Modena Y et al. (2019) Clinical outcomes of oral metronomic vinorelbine in advanced non-small cell lung cancer: correlations with pharmacokinetics and MDR1 polymorphisms. Cancer Chemother Pharmacol. 83(3), 493-500.
- 151.Jung Y J, Lee E H, Lee C G, Rhee K J, Jung W S et al. (2017) AKR1B10-inhibitory Selaginella tamariscina extract and amentoflavone decrease the growth of A549 human lung cancer cells in vitro and in vivo. J Ethnopharmacol. 202: 78 - 84, doi: 10.1016/j.jep.2017.03.010. Epub 2017 Mar 9. PubMed PMID: 28286104.
- 152.Yang S F, Chu S C, Liu S J, Chen Y C, Chang Y Z et al. (2007) Antimetastatic activities of Selaginella tamariscina (Beauv.) on lung cancer cells in vitro and in. PubMed PMID: 110(3), 483-9.
- 153.MH Do TT Le, Hoang T H, Chau V M, Nguyen T D. (2012) Toxicity and anticancer effects of an extract from Selaginella tamariscina on a mice model. Nat Prod Res. Epub 2011 Oct 14. PubMed PMID: 26(12), 1130-4.
- 154.Magesh V, DurgaBhavani K, Senthilnathan P, Rajendran P, Sakthisekaran D. (2009) In vivo protective effect of crocetin on benzo(a)pyrene-induced lung cancer in Swiss albino mice. Phytother Res. Apr;23(4): 533-9. doi: 10.1002/ptr.2666. PubMed PMID: 19067387.
- 155.Samarghandian S, Borji A, Farahmand S K, Afshari R, Davoodi S. (2013) Crocus sativus L. (saffron) stigma aqueous extract induces apoptosis in alveolar human lung cancer cells through caspase-dependent pathways activation. Biomed Res Int. Epub 2013 Oct 29. PubMed PMID: 24288678; PubMed Central PMCID: PMC3830877 1-13.
- 156.Samarghandian S, Tavakkol Afshari J, Davoodi S. (2011) Suppression of pulmonary tumor promotion and induction of apoptosis by Crocus sativus L. extraction. Appl Biochem Biotechnol. 164(2), 238-47.
- 157.Zhong Y J, Shi F, Zheng X L, Wang Q, Yang L et al. (2011) Crocetin induces cytotoxicity and enhances vincristine-induced cancer cell death via p53-dependent and -independent mechanisms. Acta Pharmacol Sin. Dec;32(12): 1529-36. doi: 10.1038/aps.2011.109. Epub 2011 Oct 10. PubMed PMID: 21986580; PubMed Central PMCID: PMC4010206 .
- 158.Bhandari P R. (2015) Crocus sativus L. (saffron) for cancer chemoprevention: A mini review. J Tradit Complement Med. 10.1016/j.jtcme.2014.10.009. eCollection 2015 Apr. Review. PubMed PMID: 26151016; PubMed Central PMCID: PMC4488115 5(2), 81-7.
- 159.Lin Y J, Liang W M, Chen C J, Tsang H, Chiou J S et al.Network analysis and mechanisms of action of Chinese herb-related natural compounds in lung cancer cells. Phytomedicine. 2019 May;58: 152893. doi: 10.1016/j.phymed.2019.152893. Epub 2019 Mar 13. PubMed PMID: 30901663.
- 160.Pajaniradje S, Mohankumar K, Pamidimukkala R, Subramanian S, Rajagopalan R. (2014) Antiproliferative and apoptotic effects of Sesbania grandiflora leaves in human cancer cells. Biomed Res Int. Epub 1-12.
- 161.Yang C J, Huang Y J, Wang C Y, Wang C S, Wang P H et al. (2010) Antiproliferative and antitumorigenic activity of Toona sinensis leaf extracts in lung adenocarcinoma. J Med Food. Feb;13(1): 54-61. doi: 10.1089/jmf.2009.1166. PubMed PMID: 20136436.
- 162.Pinmai K, Chunlaratthanabhorn S, Ngamkitidechakul C, Soonthornchareon N, Hahnvajanawong C. (2008) Synergistic growth inhibitory effects of Phyllanthus emblica and Terminalia bellerica extracts with conventional cytotoxic agents: doxorubicin and cisplatin against human hepatocellular carcinoma and lung cancer cells. PubMed PMID: 18330936; PubMed Central PMCID: PMC2693740 14(10), 1491-7.
- 163.Zhao T, Sun Q, Marques M, Witcher M. (2015) Anticancer Properties of Phyllanthus emblica (Indian Gooseberry). Oxid Med Cell Longev. Epub 2015 Jun 9. Review. PubMed PMID: 26180601; PubMed Central PMCID: PMC4477227 1, 10-1155.
- 164.Basu T, Panja S, Ghate N B, Chaudhuri D, Mandal N. (2017) Antioxidant and antiproliferative effects of different solvent fractions from Terminalia belerica Roxb. fruit on various cancer cells. Cytotechnology. 69(2), 201-216.
- 165.Hung J Y, Wen C W, Hsu Y L, Lin E S, Huang M S et al. (2013) Subamolide a induces mitotic catastrophe accompanied by apoptosis in human lung cancer cells. Evid Based Complement Alternat Med. Epub 1-15.
- 166.Li G X, Chen Y K, Hou Z, Xiao H, Jin H et al. (2010) Pro-oxidative activities and dose-response relationship of (-)-epigallocatechin-3-gallate in the inhibition of lung cancer cell growth: a comparative study in vivo and in vitro. Carcinogenesis. May;31(5): 902-10. doi: 10.1093/carcin/bgq039. Epub 2010 Feb 16. PubMed PMID: 20159951; PubMed Central PMCID: PMC2864413 .
- 167.Metwaly A M, Lianlian Z, Luqi H, Deqiang D. (2019) Black Ginseng and Its Saponins: Preparation, Phytochemistry and Pharmacological Effects. Molecules. pii: E1856. doi: 10.3390/molecules24101856. Review. PubMed PMID: 31091790; PubMed Central PMCID: PMC6572638 24(10).
- 168.Rosière R, Berghmans T, P De Vuyst, Amighi K, Wauthoz N. (2019) The Position of Inhaled Chemotherapy in the Care of Patients with Lung Tumors: Clinical Feasibility and Indications According to Recent Pharmaceutical Progresses. Cancers (Basel). 7;11(3). pii: E329. doi: 10.3390/cancers11030329. Review. PubMed PMID: 30866545; PubMed Central PMCID: PMC6468657 .
- 169.Verco J, Johnston W, Baltezor M, Kuehl P J, Gigliotti A et al. (2019) Pharmacokinetic Profile of Inhaled Submicron Particle Paclitaxel (NanoPac(®)) in a Rodent Model. J Aerosol Med Pulm Drug Deliv. Apr;32(2): 99-109. doi: 10.1089/jamp.2018.1467. Epub 2018 Oct 25. PubMed PMID: 30359162; PubMed Central PMCID: PMC6477588 .
- 170.Tan B L, Norhaizan M E. (2019) Curcumin Combination Chemotherapy: The Implication and Efficacy in Cancer. Molecules. E2527. doi: 10.3390/molecules24142527. Review. PubMed PMID: 31295906; PubMed Central PMCID: PMC6680685 24(14).
- 171.Lwin Z, Riess J W, Gandara D. (2013) The continuing role of chemotherapy for advanced non-small cell lung cancer in the targeted therapy era. J Thorac Dis. Oct;5 Suppl 5:S556-64. doi: 10.3978/j.issn.2072-1439.2013.08.47. Review. PubMed PMID: 24163748; PubMed Central PMCID: PMC3804876 .
- 172.Europa Scitech. (2018) Inhaled chemotherapy: a promising solution to treat lung cancer. , Health Research News 11.
- 173.Sapalidis K, Zarogoulidis P, Huang H, Bai C, Wen Y et al. (2018) Inhaled Immunotherapy Administration for Lung Cancer; Efficient? CertainlyPossible.JCancer. Mar2; 9(6): 1121-1126. doi: 10.7150/jca.24397. eCollection 2018. PubMed PMID: 29581792; PubMed Central PMCID:. 5868180.
- 174.Thafeni M A, Sayed Y, Motadi L R. (2012) Euphorbia mauritanica and Kedrostis hirtella extracts can induce anti-proliferative activities in lung cancer cells. Mol Biol Rep. PubMed PMID: 39(12), 10785-94.
- 175.Hsu H Y, Hwang P A. (2019) Clinical applications of fucoidan in translational medicine for adjuvant cancer therapy. Clin Transl Med. Review. PubMed PMID: 31041568; PubMed Central PMCID: PMC6491526 8(15), 1-18.
- 176.G van Weelden, Bobiński M, Okła K, van Weelden WJ, Romano A et al. (2019) Fucoidan Structure and Activity in Relation to Anti-Cancer Mechanisms. Mar Drugs. pii: E32. doi: 10.3390/md17010032. Review. PubMed PMID: 30621045; PubMed Central PMCID: PMC6356449 17(1).
- 177.Wang Y, Xing M, Cao Q, Ji A, Liang H et al. (2019) Biological Activities of Fucoidan and the Factors Mediating Its Therapeutic Effects: A Review of Recent Studies. Mar Drugs. 20; 17(3). pii: E183. doi: 10.3390/md17030183. Review. PubMed PMID: 30897733; PubMed Central PMCID: PMC6471298 .
- 178.Misra P, Singh S. (2019) Role of cytokines in combinatorial immunotherapeutics of non-small cell lung cancer through systems perspective. Cancer Med. May;8(5): 1976-1995. doi: 10.1002/cam4.2112. Epub 2019 Apr 17. Review. PubMed PMID: 30997737; PubMed Central PMCID: PMC6536974 .
- 179.Ercolano G, P De Cicco, Ianaro A. (2019) New Drugs from the Sea: Pro-Apoptotic Activity of Sponges and Algae Derived Compounds. Mar Drugs. pii: E31. doi: 10.3390/md17010031. Review. PubMed PMID: 30621025; PubMed Central PMCID: PMC6356258 17(1).
- 180.Song J, Su H, Wang B L, Zhou Y Y, Guo L L.Fish consumption and lung cancer risk: systematic review and meta-analysis. Epub 2014 Apr 7. Review. PubMed PMID: , Nutr Cancer 66(4), 539-49.
- 181.Siu F M, Ma D L, Cheung Y W, Lok C N, Yan K et al. (2008) Proteomic and transcriptomic study on the action of a cytotoxic saponin (Polyphyllin D): induction of endoplasmic reticulum stress and mitochondria-mediated apoptotic pathways. Proteomics. Aug;8(15): 3105-17. doi: 10.1002/pmic.200700829. PubMed PMID: 18615425.
- 182.Takezaki T, Inoue M, Kataoka H, Ikeda S, Yoshida M et al. (2003) Diet and lung cancer risk from a 14-year population-based prospective study in Japan: with special reference to fish consumption. PubMed PMID: , Nutr Cancer 45(2), 160-7.
- 183.Yang P, Cartwright C, Chan D, Ding J, Felix E et al.Anticancer activity of fish oils against human lung cancer is associated with changes. in formation of PGE2 and PGE3 and alteration of Akt phosphorylation. Mol Carcinog. 2014 Jul;53(7): 566-77. doi: 10.1002/mc.22008. Epub 2013 Jan 31. PubMed PMID: 23371504; PubMed Central PMCID: PMC4395033 .
- 184.Daniel C R, Cross A J, Graubard B I, Hollenbeck A R, Park Y et al. (2011) Prospective investigation of poultry and fish intake in relation to cancer risk. Cancer Prev Res (Phila). 4(11), 1903-11.
- 185.Sun Y, Li Z, Li J, Li Z, Han J. (2016) A Healthy Dietary Pattern Reduces Lung Cancer Risk: A Systematic Review and Meta-Analysis. Nutrients. 4;8(3): 134. doi: 10.3390/nu8030134. Review. PubMed PMID: 26959051; PubMed Central PMCID: PMC4808863 .
- 186.Elisia I, Cho B, Hay M, Li M Y, Hofs E et al. (2019) The effect of diet and exercise on tobacco carcinogen-induced lung cancer. Carcinogenesis. PubMed PMID: 40(3), 448-460.
- 187.Alsharairi N A. (2019) The Effects of Dietary Supplements on Asthma and Lung Cancer Risk in Smokers and Non-Smokers: A Review of the Literature. pii: E725. doi: 10.3390/nu11040725. Review. PubMed PMID: 30925812; PubMed Central PMCID: PMC6521315 , Nutrients 11(4).
- 188.Middha P, Weinstein S J, Männistö S, Albanes D, Mondul A M. (2019) β-Carotene Supplementation and Lung Cancer Incidence in the Alpha-Tocopherol, Beta-Carotene Cancer Prevention Study: The Role of Tar and Nicotine. Nicotine Tob Res. 10.1093/ntr/nty115. PubMed PMID: 29889248; PubMed Central PMCID: PMC6636175 21(8), 1045-1050.
- 189.Narita S, Saito E, Sawada N, Shimazu T, Yamaji T et al. (2018) Tsugane S; JPHC Study Group. Dietary consumption of antioxidant vitamins and subsequent lung cancer risk: The Japan Public Health Center-based prospective study. Epub 2018 Jan 31. PubMed PMID: , Int 142(12), 2441-2460.
- 190.Sealock T, Sharma S. (2019) Smoking Cessation. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing;. Available from:https://www.ncbi.nlm.nih.gov/books/NBK482442/
- 191.Steliga M A, Yang P. (2019) Integration of smoking cessation and lung cancer screening. Transl Lung Cancer Res. May;8(Suppl 1):S88-S94. doi: 10.21037/tlcr.2019.04.02. Review. PubMed PMID: 31211109; PubMed Central PMCID: PMC6546623 .
- 192.Taylor K L, Deros D E, Fallon S, Stephens J, Kim E et al. (2019) Study protocol for a telephone-based smoking cessation randomized controlled trial in the lung cancer screening setting: The lung screening, tobacco, and health trial. Contemp Clin Trials. Jul;82: 25-35. doi: 10.1016/j.cct.2019.05.006. Epub 6657688.
- 193.Robbins S L, Kumar V, Cotran R S. (2010) Robbins and Cotran Pathologic Basis of Disease. , Philadelphia, PA:Elsevier
- 194.Vakiti A, Mewawalla P Cancer. (2019) Acute Myeloid Leukemia (AML, Erythroid Leukemia, Myelodysplasia-Related Leukemia. Available from:https://www.ncbi.nlm.nih.gov/books/NBK507875/ , BCR-ABL Chronic Leukemia) [Updated
- 195.Naik J, Themeli M, R de Jong-Korlaar, RWJ Ruiter, Poddighe P J et al.CD38 as a therapeutic target for adult acute myeloid leukemia and T-cell acute lymphoblastic leukemia. Haematologica. 2019 Mar;104(3):e100-e103. doi: 10.3324/haematol.2018.192757. Epub 2018 Sep 6. PubMed PMID: 30190344; PubMed Central PMCID: PMC6395314 .
- 196.Bawazir A, Al-Zamel N, Amen A, Akiel M A, Alhawiti N M et al. (2019) The burden of leukemia in the Kingdom of Saudi Arabia: 15 period (1999-2013). BMC Cancer. PubMed PMID: 31315607; PubMed Central PMCID: PMC6637507 19(703), 1-10.
- 197.Dhall A, Zee B M, Yan F, Blanco M A. (2019) Intersection of Epigenetic and Metabolic Regulation of Histone Modifications in Acute Myeloid Leukemia. Front Oncol. 22;9: 432. doi: 10.3389/fonc.2019.00432. eCollection 2019. Review. PubMed PMID: 31192132; PubMed Central PMCID: PMC6540842 .
- 198.Medeiros B C, Chan S M, Daver N G, Jonas B A, Pollyea D A. (2019) Optimizing survival outcomes with post-remission therapy in acute myeloid leukemia. Jul;94(7): 803-811. doi: 10.1002/ajh.25484. Epub 2019 May 1. Review. PubMed PMID: 30945331; PubMed Central PMCID: PMC6593671 , Am.
- 199.Murphy B R, Roth M, Kolb E A, Alonzo T, Gerbing R et al. (2019) Development of acute lymphoblastic leukemia following treatment for acute myeloid leukemia in children with Down syndrome: A case report and retrospective review of Children's Oncology Group acute myeloid leukemia trials. Pediatr Blood Cancer. Aug;66(8):e27700. doi: 10.1002/pbc.27700. Epub 2019 Mar 25. Review. PubMed PMID: 30908863.
- 200.Puckett Y, Chan O. (2019) Cancer, Acute Lymphocytic Leukemia (ALL), In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing;. Available from: https://www.ncbi.nlm.nih.gov/books/NBK459149/
- 201.Branford S, DDH Kim, Apperley J F, Eide C A, Mustjoki S et al. (2019) Hochhaus A, Hughes TP; International CML Foundation Genomics Alliance. Laying the foundation for genomically-based risk assessment in chronic myeloid leukemia. Leukemia. Review. PubMed PMID: 33(8), 1835-1850.
- 203.Rahimi Babasheikhali S, Rahgozar S, Mohammadi M. (2019) Ginger extract has anti-leukemia and anti-drug resistant effects on malignant cells. , J Cancer Res Clin Oncol 145(8), 1987-1998.
- 204.Hwang D, Kim M, Park H, Jeong M I, Jung W et al. (2019) Natural Products and Acute Myeloid Leukemia: A Review Highlighting Mechanisms of Action. Nutrients. 3;11(5). pii: E1010. doi: 10.3390/nu11051010. Review. PubMed PMID: 31058874; PubMed Central PMCID: PMC6567155 .
- 205.Bhargava S, Malhotra H, Rathore O S, Malhotra B, Sharma P et al. (2015) Chiplunkar SV. Anti-leukemic activities of alcoholic extracts of two traditional Indian medicinal plants. Epub , Leuk Lymphoma 56(11), 3168-82.
- 206.Yang C, Cai H, Meng X. (2016) Polyphyllin D induces apoptosis and differentiation in K562 human leukemia cells. Int Immunopharmacol. Jul;36: 17-22. doi: 10.1016/j.intimp.2016.04.011. Epub 2016 Apr 19. PubMed PMID: 27104314.
- 207.Wu L, Li Q, Liu Y. (2014) Polyphyllin D induces apoptosis in K562/A02 cells through G2/M phase arrest. May;66(5): 713-21. doi: 10.1111/jphp.12188. Epub 2013 Dec 11. PubMed PMID: , J Pharm Pharmacol 24325805.
- 208.Turrini E, Calcabrini C, Sestili P, Catanzaro E, E de Gianni et al. (2016) Withania somnifera Induces Cytotoxic and Cytostatic Effects on Human T Leukemia Cells. Toxins (Basel). 12;8(5). pii: E147. doi: 10.3390/toxins8050147. PubMed PMID: 27187469; PubMed Central PMCID: PMC4885062 .
- 209.Pires N, Gota V, Gulia A, Hingorani L, Agarwal M et al. (2019) Safety and Pharmacokinetics of Withaferin-A in advanced stage high grade Osteosarcoma: A phase I trial. J Ayurveda Integr Med. pii: S0975-9476(18)30789-7. doi: 10.1016/j.jaim.2018.12.008. [Epub ahead of print] PubMed PMID: 30904387.
- 210.Kim S, Yu J S, Lee J Y, Choi S U, Lee J et al.Cytotoxic Withanolides from the Roots of Indian Ginseng (Withania somnifera). 10.1021/acs.jnatprod.8b00665. Epub 2019 Feb 18. PubMed PMID: , J Nat Prod. 2019 Apr 82(4), 765-773.
- 211.Li C, Dong L, Su R, Bi Y, Qing Y et al.Homoharringtonine exhibits potent anti-tumor effect and modulates DNA epigenome in acute myeloid leukemia by targeting. SP1/TET1/5hmC. Haematologica. 2019 Apr 11. pii: haematol.2018.208835. doi: 10.3324/haematol.2018.208835. [Epub ahead of print] PubMed PMID: 30975912.
- 212.Zhang J, Geng H, Liu L, Zhang H. (2019) Synergistic cytotoxicity of homoharringtonine and etoposide in acute myeloid leukemia cells involves disrupted antioxidant defense. Cancer Manag Res. , Jan22; 11, 1023-1032.
- 213.Wu Z, Zhuang H, Yu Q, Zhang X, Jiang X et al.. Homoharringtonine Combined with the Heat Shock Protein 90 Inhibitor IPI504 in the Treatment of FLT3-ITD Acute Myeloid Leukemia. Transl Oncol. 2019 Jun;12(6): 801-809. doi: 10.1016/j.tranon.2019.02.016. Epub 2019 Apr 4. PubMed PMID: 30953928; PubMed Central PMCID: PMC6449739 .
- 214.Yakhni M, Briat A, A El Guerrab, Furtado L, Kwiatkowski F et al. (2019) Homoharringtonine, an approved anti-leukemia drug, suppresses triple negative breast cancer growth through a rapid reduction of anti-apoptotic protein abundance. Am J Cancer Res. 9(5), 1043-1060.
- 215.Huang S, Pan J, Jin J, Li C, Li X et al. (2019) a novel BTK inhibitor: Anti-Leukemia effects and synergistic efficacy with homoharringtonine in acute myeloid leukemia. Cancer Lett. Oct1; 461: 132-143. doi: 10.1016/j.canlet.2019.07.008. Epub 2019 Jul 13. PubMed PMID: 31310800.
- 216.Tan M, Zhang Q, Yuan X, Chen Y, Wu Y. (2019) Synergistic killing effects of homoharringtonine and arsenic trioxide on acute myeloid leukemia stem cells and the underlying mechanisms. J Exp Clin Cancer Res. PubMed PMID: 31307525; PubMed Central PMCID: PMC6631946 , Jul15; 38(308), 1-8.
- 217.Chen P, Zhan W, Wang B, You P, Jin Q et al. (2019) Homoharringtonine potentiates the antileukemic activity of arsenic trioxide against acute myeloid leukemia cells. Exp Cell Res. Mar15; 376(2): 114-123. doi: 10.1016/j.yexcr.2019.02.008. Epub 2019 Feb 11. PubMed PMID: 30763586.
- 218.Chen X J, Zhang W N, Chen B, Xi W D, Lu Y et al. (2019) Homoharringtonine deregulates MYC transcriptional expression by directly binding NF-κB repressing factor. Proc Natl Acad Sci U S A. 2019 Feb 5;116(6): 2220-2225. doi: 10.1073/pnas.1818539116. Epub 6369765.
- 219.Lien le Q, Linh T M, Giang V H, Mai N C, Nhiem N X et al. (2016) New naphthalene derivatives and isoquinoline alkaloids from Ancistrocladus cochinchinensis with their anti-proliferative activity on human cancer cells. Bioorg Med Chem Lett. Epub 2016 Jul 5. PubMed PMID: 26(16), 3913-7.
- 220.Dantas B B, Faheina-Martins G V, Coulidiati T H, Bomfim C C, C da Silva Dias et al. (2015) Effects of curine in HL-60 leukemic cells: cell cycle arrest and apoptosis induction. PubMed PMID: , J Nat Med. 2015 Apr;69(2): 218-23.
- 221.Chen L G, Su P J, Tsai P W, Yang L L, Wang C C. (2016) Intermedin A, a New Labdane Diterpene Isolated from Alpinia intermedia. Prolonged the Survival Time of P-388D1 Tumor-Bearing CDF1 Mice. Planta Med. 2017 Jan;83(1-02): 151-157.
- 222.Li D H, Li J Y, Xue C M, Han T, Sai C M et al. (2017) Antiproliferative Dimeric Aporphinoid Alkaloids from the Roots of Thalictrum cultratum. 10.1021/acs.jnatprod.7b00387. Epub 2017 Nov 13. PubMed PMID: , J 80(11), 2893-2904.
- 223.Lam N S, Long X, Wong J W, Griffin R C, JCG Doery. (2019) Artemisinin and its derivatives: a potential treatment for leukemia. Anticancer Drugs. Jan;30(1): 1-18. doi: 10.1097/CAD.0000000000000697. PubMed PMID: 30540593.
- 224.Beck J, Schwarzer A, Gläser D, Mügge L O, Uhlig J et al. (2017) Lenalidomide in combination with bendamustine and prednisolone in relapsed/refractory multiple myeloma: results of a phase 2 clinical trial (OSHO-#077). J Cancer Res Clin Oncol. 143(12), 2545-2553.
- 225.Drenberg C D, Buaboonnam J, Orwick S J, Hu S, Li L et al. (2016) Evaluation of artemisinins for the treatment of acute myeloid leukemia. Cancer Chemother Pharmacol. 77(6), 1231-43.
- 226.Letis A S, Seo E J, Nikolaropoulos S S, Efferth T, Giannis A et al. (2017) Synthesis and cytotoxic activity of new artemisinin hybrid molecules against human leukemia cells. Bioorg Med Chem. 10.1016/j.bmc.2017.04.021. Epub 2017 Apr 20. PubMed PMID: 25(13), 3357-3367.
- 227.Houh Y K, Kim K E, Park S, Hur D Y, Kim S et al.. The Effects of Artemisinin on the Cytolytic Activity of Natural Killer (NK) Cells. Int J Mol Sci. 2017 Jul 24;18(7). pii: E1600. doi: 10.3390/ijms18071600. PubMed PMID: 28737711; PubMed Central PMCID: PMC5536087 .
- 228.Jiang H Y, Wang C F, Fan L, Yang K, Feng J B et al. (2013) Cytotoxic constituents from the stems of Clausena lansium (Lour.) Skeels. Molecules. 10.3390/molecules180910768. PubMed PMID: 24005969; PubMed Central PMCID: PMC6270150 18(9), 10768-75.
- 229.Kim S P, Kang M Y, Choi Y H, Kim J H, Nam S H et al. (2011) Mechanism of Hericium erinaceus (Yamabushitake) mushroom-induced apoptosis of U937 human monocytic leukemia cells. Food Funct. Jun;2(6): 348-56. doi: 10.1039/c1fo10030k. Epub 2011 Jun 8. PubMed PMID: 21779573.
- 230.Nomura M, Takahashi T, Uesugi A, Tanaka R, Kobayashi S Inotodiol. (2008) a lanostane triterpenoid, from Inonotus obliquus inhibits cell proliferation through caspase-3-dependent apoptosis. Anticancer Res. Sep-Oct;28(5A): 2691-6. PubMed PMID: 19035296.
- 231.Bayan L, Koulivand P H, Gorji A. (2014) Garlic: a review of potential therapeutic effects. Avicenna. Jan;4(1): 1-14. Review. PubMed PMID: 25050296; PubMed Central PMCID: PMC4103721 .
- 232.Antlsperger D S, Dirsch V M, Ferreira D, Su J L, Kuo M L et al. (2003) Ajoene-induced cell death in human promyeloleukemic cells does not require JNK but is amplified by the inhibition of ERK. Oncogene. , Jan30; 22(4), 582-9.
- 233.Zhang G, Gao X, Zeng H, Li Y, Guo X. (2018) Virosecurinine induces apoptosis in human leukemia THP-1 cells and other underlying molecular mechanisms. Oncol Lett. Jan;15(1): 849-854. doi: 10.3892/ol.2017.7437. Epub 5772865.
- 234.Zhang G, Li M, Han S, Chen D, Wang Y et al. (2014) Induction of human chronic myeloid leukemia K562 cell apoptosis by virosecurinine and its molecular mechanism. Mol Med Rep. Nov;10(5): 2365-71. doi: 10.3892/mmr.2014.2531. Epub 2014 Sep 3. PubMed PMID: 25189629; PubMed Central PMCID: PMC4214351 .
- 235.Yang J, Chen L, Yan Y, Qiu J, Chen J et al. (2019) BW18, a C-21 steroidal glycoside, exerts an excellent anti-leukemia activity through inducing S phase cell cycle arrest and apoptosis via MAPK pathway in K562 cells. Biomed Pharmacother. Apr;112: 108603. doi: 10.1016/j.biopha.2019.108603. Epub 2019 Feb 20. PubMed PMID: 30784914.
- 236.Larasati Y A, Yoneda-Kato N, Nakamae I, Yokoyama T, Meiyanto E et al. (2018) Curcumin targets multiple enzymes involved in the ROS metabolic pathway to suppress tumor cell growth. Sci Rep. Feb1; 8(1): 2039. doi: 10.1038/s41598-018-20179-6. PubMed PMID: 29391517; PubMed Central PMCID: PMC5794879 .
- 237.Kouhpeikar H, Butler A E, Bamian F, Barreto G E, Majeed M et al. (2019) Curcumin as a therapeutic agent in leukemia. Aug;234(8): 12404-12414. doi: 10.1002/jcp.28072. Epub 2019 Jan 4. Review. PubMed PMID: , J Cell Physiol 30609023.
- 238.Kujundžić R N, Stepanić V, Milković L, AČ Gašparović, Tomljanović M et al.Curcumin and its Potential for Systemic Targeting of Inflamm-Aging and Metabolic Reprogramming. in Cancer. Int J Mol Sci. 2019 Mar 8;20(5). pii: E1180. doi: 10.3390/ijms20051180. Review. PubMed PMID: 30857125; PubMed Central PMCID: PMC6429141 .
- 239.Santana-Bejarano U F, Bobadilla-Morales L, Mendoza-Maldonado L, Torres-Anguiano E, Brukman-Jiménez S A et al. (2019) In vitro effect of curcumin in combination with chemotherapy drugs in Ph(+) acute lymphoblastic leukemia cells. Oncol Lett. Jun;17(6): 5224-5240. doi: 10.3892/ol.2019.10204. Epub 2019 Apr 2. PubMed PMID: 31186739; PubMed Central PMCID: PMC6507345 .
- 240.Henry D, Brumaire S, Hu X. (2019) Involvement of pRb-E2F pathway in green tea extract-induced growth inhibition of human myeloid leukemia cells. Leuk Res. Feb;77: 34-41. doi: 10.1016/j.leukres.2018.12.014. Epub 2019 Jan 2. PubMed PMID: 30641474.
- 241.Iwasaki R, Ito K, Ishida T, Hamanoue M, Adachi S et al. (2009) Catechin, green tea component, causes caspase-independent necrosis-like cell death in chronic myelogenous leukemia. Cancer Sci. PubMed PMID: 100(2), 349-56.
- 242.Marjanovic G.The use of inexpensive broad spectrum lower toxicity therapeutics in chronic lymphocytic leukemia. J BUON. 2017 Mar-Apr;22(2): 288-294. Review. PubMed PMID: 28534346.
- 243.Yang C S, Wang H. (2013) Cancer therapy combination: green tea and a phosphodiesterase 5 inhibitor? J Clin Invest. Feb;123(2): 556-8. doi: 10.1172/JCI67589. Epub 2013 Jan 25. PubMed PMID: 23348734; PubMed Central PMCID: PMC3561839 .
- 244.Yang C S, Wang H. (2016) Cancer Preventive Activities of Tea Catechins. Molecules. 9;21(12). pii: E1679. Review. PubMed PMID: 27941682; PubMed Central PMCID: PMC6273642 .
- 245.Angelo L S, Kurzrock R. (2009) Turmeric and green tea: a recipe for the treatment of B-chronic lymphocytic leukemia. Clin Cancer Res. PubMed PMID: 19228716; PubMed Central PMCID: PMC2646173 15(4), 1123-5.
- 246.Shanafelt T D, Call T G, Zent C S, Leis J F, LaPlant B et al.. Phase 2 trial of daily, oral Polyphenon E in patients with asymptomatic, Rai stage 0 to II chronic lymphocytic leukemia. Cancer. 2013 Jan15; 119(2): 363-70. doi: 10.1002/cncr.27719. Epub 2012 Jul 3. PubMed PMID: 22760587; PubMed Central PMCID: PMC3902473 .
- 247.Smith D M, Dou Q P. (2001) Green tea polyphenol epigallocatechin inhibits DNA replication and consequently induces leukemia cell apoptosis. Int J Mol Med. Jun;7(6): 645-52. PubMed PMID: 11351279.
- 248.Lee Y K, Bone N D, Strege A K, Shanafelt T D, Jelinek D F et al. (2004) VEGF receptor phosphorylation status and apoptosis is modulated by a green tea component, epigallocatechin-3-gallate (EGCG). in B-cell chronic lymphocytic leukemia. Blood 104(3), 788-94.
- 249.Gao N, Budhraja A, Cheng S, Yao H, Zhang Z et al. (2009) Induction of apoptosis in human leukemia cells by grape seed extract occurs via activation of c-Jun NH2-terminal kinase. Clin Cancer Res. PubMed PMID: 19118041; PubMed Central PMCID: PMC2760842 15(1), 140-9.
- 250.Saedi T A, Noor S, Ismail P, Othman F. (2014) The effects of herbs and fruits on leukaemia. Evid Based Complement Alternat Med. Epub 2014 Aug 27. Review. PubMed PMID: 25250054; PubMed Central PMCID: PMC4163312 1-8.
- 251.Espino J, González-Gómez D, Moreno D, Fernández-León M F, Rodríguez A B et al. (2013) Tempranillo-derived grape seed extract induces apoptotic cell death and cell growth arrest in human promyelocytic leukemia HL-60 cells. Food Funct. Dec;4(12): 1759-66. doi: 10.1039/c3fo60267b. Epub 2013 Oct 16. PubMed PMID: 24129601.
- 252.AAB Al-Asady, HMS Algarmavy, SKM Salih.Antileukemic Effect of Polyphenol of Local Grape Seeds Extract from Duhok/Kurdistan of Iraq:. in vitro Study. Research in Cell Biology 2017 3(1), 1-6.
- 253.Cao W J, Wu K, Wang C, Wan D M. (2016) Polydatin-induced cell apoptosis and cell cycle arrest are potentiated by Janus kinase 2 inhibition in leukemia cells. Mol Med Rep. Apr;13(4): 3297-302. doi: 10.3892/mmr.2016.4909. Epub 2016 Feb 18. PubMed PMID: 26934953.
- 254.Papandreou I, Verras M, McNeil B, Koong A C, Denko N C. (2015) Plant stilbenes induce endoplasmic reticulum stress and their anti-cancer activity can be enhanced by inhibitors of autophagy. Exp Cell Res. 10.1016/j.yexcr.2015.10.014. Epub 2015 Oct 17. PubMed PMID: 26477823; PubMed Central PMCID: PMC4822495 339(1), 147-53.
- 255.Frazzi R, Guardi M. (2017) Cellular and Molecular Targets of Resveratrol on Lymphoma and Leukemia Cells. Molecules. pii: E885. doi: 10.3390/molecules22060885. Review. PubMed PMID: 28555002; PubMed Central PMCID: PMC6152792 22(6).
- 256.Hu H, Qin Y M. (2006) Grape seed proanthocyanidin extract induced mitochondria-associated apoptosis in human acute myeloid leukaemia 14.3D10 cells. PubMed PMID: , Chin Med 119(5), 417-21.
- 257.Dahlawi H, Jordan-Mahy N, Clench M, McDougall G J, Maitre C L. (2013) Polyphenols are responsible for the proapoptotic properties of pomegranate juice on leukemia cell lines. Food Sci Nutr. Mar;1(2): 196-208. doi: 10.1002/fsn3.26. Epub 2013 Feb 20. PubMed PMID: 24804028; PubMed Central PMCID: PMC3967757 .
- 258.Kawaii S, Lansky E P. (2004) Differentiation-promoting activity of pomegranate (Punica granatum) fruit extracts in HL-60 human promyelocytic leukemia cells. J Med Food. Spring;7(1): 13-8. PubMed PMID: 15117547.
- 259.Asmaa M J, Ali A J, Farid J M, Azman S.Growth inhibitory effects of crude pomegranate peel extract on chronic myeloid leukemia, K562 cells. PubMed PMID: 26097816; PubMed Central PMCID: , Int J Appl Basic Med Res. 2015 May-Aug;5(2): 100-5.
- 260.Dahlawi H, Jordan-Mahy N, Clench M R, Le Maitre CL.Bioactive actions of pomegranate fruit extracts on leukemia cell lines in vitro hold promise for new therapeutic agents for leukemia. Epub 2011 Nov 18. PubMed PMID: , Nutr Cancer 64(1), 100-10.
- 261.Joseph M M, Aravind S R, Varghese S, Mini S, Sreelekha T T. (2012) Evaluation of antioxidant, antitumor and immunomodulatory properties of polysaccharide isolated from fruit rind of Punica granatum. Mol Med Rep. Feb;5(2): 489-96. doi: 10.3892/mmr.2011.638. Epub 2011 Oct 18. PubMed PMID: 22012001.
- 262.Choi Y J, Yoon J H, Cha S W, Lee S G.Ginsenoside Rh1 inhibits the invasion and migration of THP-1 acute monocytic leukemia cells via inactivation of the MAPK signaling pathway. Fitoterapia. 2011 Sep;82(6): 911-9. doi: 10.1016/j.fitote.2011.05.005. Epub 2011 May 14. PubMed PMID: 21605636.
- 263.Compound K. (2009) a metabolite of ginseng saponin, induces apoptosis via caspase-8-dependent pathway in HL-60 human leukemia cells. PubMed PMID: 20017956; PubMed Central PMCID: PMC2806409 , BMC Cancer. Dec18; 9, 449-10.
- 264.Chen Y, Xu Y, Zhu Y, Li X. (2013) Anti-cancer effects of ginsenoside compound k on pediatric acute myeloid leukemia cells. Cancer Cell Int. PubMed PMID: 23497352; PubMed Central PMCID: PMC3602037 13(1), 24-10.
- 265.Park J G, Son Y J, Aravinthan A, Kim J H, Cho J Y. (2016) Korean Red Ginseng water extract arrests growth of xenografted lymphoma cells. J Ginseng Res. Oct;40(4): 431-436. Epub 2016 Aug 4. PubMed PMID: 27746697; PubMed Central PMCID: PMC5052435 .
- 266.Park S E, Park C, Kim S H, Hossain M A, Kim M Y et al. (2009) Korean red ginseng extract induces apoptosis and decreases telomerase activity in human leukemia cells. J Ethnopharmacol. 121(2), 304-12.
- 267.Ardalani H, Avan A, Ghayour-Mobarhan M. (2017) Podophyllotoxin: a novel potential natural anticancer agent. Avicenna. Jul-Aug;7(4): 285-294. Review. PubMed PMID: 28884079; PubMed Central PMCID: PMC5580867 .
- 268.Yusenko M, Jakobs A, Klempnauer K H. (2018) A novel cell-based screening assay for small-molecule MYB inhibitors identifies podophyllotoxins teniposide and etoposide as inhibitors of MYB activity. Sci Rep. PubMed PMID: 30177851; PubMed Central PMCID: PMC6120916 8(1), 1-11.
- 269.Cao B, Yang S, Li W, Chen H, Chen Y et al. (2018) GMZ-1 is a podophyllotoxin derivative that suppresses growth and induces apoptosis in adriamycin-resistant K562/A02 cells through modulation of MDR1 expression. Mol Med Rep. Jan;17(1): 474-478. doi: 10.3892/mmr.2017.7862. Epub 2017 Oct 25. PubMed PMID: 29115592.
- 270.Silveira A L, Faheina-Martins G V, Maia R C, Araújo D A. (2014) Compound A398, a novel podophyllotoxin analogue: cytotoxicity and induction of apoptosis in human leukemia cells. PLoS One. doi: 10.1371/journal.pone.0107404. eCollection 2014. PubMed PMID: 25221997; PubMed Central PMCID: PMC4164611 9(9), 107404.
- 271.Illiano M, Conte M, Sapio L, Nebbioso A, Spina A et al.Forskolin Sensitizes Human Acute Myeloid Leukemia Cells to. H3K27me2/3 Demethylases GSKJ4 Inhibitor via Protein Kinase A. Front Pharmacol. 2018 Jul 20;9: 792. doi: 10.3389/fphar.2018.00792. eCollection 2018. PubMed PMID: 30079022; PubMed Central PMCID: PMC6063003 .
- 272.Hodroj M H, Jardaly A, Abi Raad S, Zouein A, Rizk S. (2018) Andrographolide potentiates the antitumor effect of topotecan in acute myeloid leukemia cells through an intrinsic apoptotic pathway. Cancer Manag Res. 10, 1079-1088.
- 273.Yang T, Yao S, Zhang X, Guo Y. (2016) Andrographolide inhibits growth of human T-cell acute lymphoblastic leukemia Jurkat cells by downregulation of PI3K/AKT and upregulation. of p38 MAPK pathways. Drug Des Devel Ther. Apr11; 10: 1389-1397. doi: 10.2147/DDDT.S94983. eCollection 2016. PubMed PMID: 27114702; PubMed Central PMCID: PMC4833376 .
- 274.Sarkar S, Gopal P K, Paul S.Andrographolide Induced Apoptosis in NALM-6 Cells Mediated Through the Cell Cycle Arrest and Nuclear Fragmentation. DOI: 10.5530/pj.2018.2.36. Available from:http://www.phcogj.com/sites/default/files/PharmacognJ-10_2_210.pdf , Pharmacog J 10(2), 210-4.
- 275.Cheung H Y, Cheung S H, Li J, Cheung C S, Lai W P et al. (2005) Andrographolide isolated from Andrographis paniculata induces cell cycle arrest and mitochondrial-mediated apoptosis in human leukemic HL-60 cells. Planta Med. Dec;71(12): 1106-11. PubMed PMID: 16395645.
- 276.Liao H C, Chou Y J, Lin C C, Liu S H, Oswita A et al. (2019) Andrographolide and its potent derivative exhibit anticancer effects against imatinib-resistant chronic myeloid leukemia cells by downregulating the Bcr-Abl oncoprotein. Biochem Pharmacol. May;163: 308-320. doi: 10.1016/j.bcp.2019.02.028. Epub 2019 Feb 26. PubMed PMID: 30822403.
- 277.Manikam S D, Stanslas J. (2009) Andrographolide inhibits growth of acute promyelocytic leukaemia cells by inducing retinoic acid receptor-independent cell differentiation and apoptosis. J Pharm Pharmacol. Jan;61(1): 69-78. doi: 10.1211/jpp/61.01.0010. Erratum in: J Pharm Pharmacol. 2009 May;61(5): 687. Manikam, Shiamala T [corrected to Manikam, Shiamala T]. PubMed PMID: 19126299.
- 278.Chen X, Zhang J, Yuan L, Lay Y, Wong Y K et al.. Andrographolide Suppresses MV4-11 Cell Proliferation through the Inhibition of FLT3 Signaling, Fatty Acid Synthesis and Cellular Iron Uptake. Molecules. 2017 Aug 31;22(9). pii: E1444. doi: 10.3390/molecules22091444. PubMed PMID: 28858244; PubMed Central PMCID: PMC6151431 .
- 279.Chatterjee K, AlSharif D, Mazza C, Syar P, Al Sharif M et al.. Resveratrol and Pterostilbene Exhibit Anticancer Properties Involving the Downregulation of HPV Oncoprotein E6 in Cervical Cancer Cells. Nutrients. 2018 Feb 21;10(2). pii: E243. doi: 10.3390/nu10020243. PubMed PMID: 29485619; PubMed Central PMCID: PMC5852819 .
- 280.Ramezani G, Pourgheysari B, Shirzad H, Sourani Z. (2019) Pterostilbene increases Fas expression in T-lymphoblastic leukemia cell lines. Res Pharm Sci. PubMed PMID: 30936933; PubMed Central PMCID: PMC6407337 14(1), 55-63.
- 281.McGill C M, Brown T J, Cheng Y Y, Fisher L N, Shanmugavelandy S S et al. (2018) Therapeutic Effect of Blueberry Extracts for Acute Myeloid Leukemia. Int J Biopharm Sci. Jan;1(1). pii: 102. Epub 2018 Jan 2. PubMed PMID: 29607443; PubMed Central PMCID: PMC5875929 .
- 282.McGill C M, Brown T J, Fisher L N, Gustafson S J, Dunlap K L et al. (2018) Combinatorial Efficacy of Quercitin and Nanoliposomal Ceramide for Acute Myeloid Leukemia. pii: 106. doi: 10.31021/ijbs.20181106. Epub , Int J Biopharm Sci 1(1), 6349237.
- 283.Liu Z, Li F, Zhang B, Li S, Wu J et al. (2015) Structural basis of plant homeodomain finger 6 (PHF6) recognition by the retinoblastoma binding protein 4 (RBBP4) component of the nucleosome remodeling and deacetylase (NuRD) complex. , J Biol Chem. 2015 Mar 290(10), 6630-8.
- 284.P Van Vlierberghe, Patel J, Abdel-Wahab O, Lobry C, Hedvat C V et al. (2010) 29. PubMed PMID: 21030981; PubMed Central PMCID:. PHF6 mutations in adult acute myeloid leukemia. Leukemia. 2011 Jan;25(1): 130-4. doi: 10.1038/leu.2010.247. Epub 3878659.
- 285.Ge Z, Gu Y, Han Q, Sloane J, Ge Q et al. (2018) Plant homeodomain finger protein 2 as a novel IKAROS target in acute lymphoblastic leukemia. Epigenomics. 10(1), 59-69.
- 286.Wendorff A A, Quinn S A, Rashkovan M, Madubata C J, Ambesi-Impiombato A et al. (2018) 19. PubMed PMID: 30567843; PubMed Central PMCID:. Phf6 Loss Enhances HSC Self-Renewal Driving Tumor Initiation and Leukemia Stem Cell Activity in T-ALL. Cancer Discov. 2019 Mar;9(3): 436-451.
- 287.Sarkar M K, Vadivel V, MRC Raja, Kar Mahapatra S. (2019) Investigation of phytochemical constituents of anti-leukemic herbal drugs used by the traditional healers of Purulia, Birbhum and Bankura districts of West Bengal. Nat Prod Res. [Epub ahead of print] PubMed PMID: 15, 1-6.
- 288.Danışman Kalındemirtaş F, Birman H, Candöken E, Bilgiş Gazioğlu S, Melikoğlu G et al. (2019) Cytotoxic Effects of Some Flavonoids and Imatinib on the K562 Chronic Myeloid Leukemia Cell Line: Data Analysis Using the Combination Index Method. Balkan Med J. Epub 2018 Nov 5. PubMed PMID: 30396879; PubMed Central PMCID: PMC6409953 36(2), 96-105.
- 289.Wei C, Xiao Q, Kuang X, Zhang T, Yang Z et al. (2015) Fucoidan inhibits proliferation of the SKM-1 acute myeloid leukaemia cell line via the activation of apoptotic pathways and production of reactive oxygen species. Mol Med Rep. Nov;12(5): 6649-55. doi: 10.3892/mmr.2015.4252. Epub 2015 Aug 25. PubMed PMID: 26324225; PubMed Central PMCID: PMC4626197 .
- 290.Park H S, Hwang H J, Kim G Y, Cha H J, Kim W J et al.Induction of apoptosis by fucoidan in human leukemia U937 cells through activation. of p38 MAPK and modulation of Bcl-2 family. Mar Drugs. 2013 Jul 4;11(7): 2347-64. doi: 10.3390/md11072347. PubMed PMID: 23880928; PubMed Central PMCID: PMC3736427 .
- 291.Atashrazm F, Lowenthal R M, Woods G M, Holloway A F, Karpiniec S S et al.Fucoidan Suppresses the Growth of Human Acute Promyelocytic Leukemia Cells In. Vitro and In Vivo. J Cell Physiol. 2016 Mar;231(3): 688-97. doi: 10.1002/jcp.25119. PubMed PMID: 26241708.
- 292.Atashrazm F, Lowenthal R M, Dickinson J L, Holloway A F, Woods G M. (2016) Fucoidan enhances the therapeutic potential of arsenic trioxide and all-trans retinoic acid in acute promyelocytic leukemia. 10.18632/oncotarget.10016. PubMed PMID: 27329592; PubMed Central PMCID: PMC5216779 in vitro and in 7(29), 46028-46041.
- 293.Rengarajan T, Rajendran P, Nandakumar N, Balasubramanian M P, Nishigaki I. (2013) Cancer preventive efficacy of marine carotenoid fucoxanthin: cell cycle arrest and apoptosis. Nutrients. 10.3390/nu5124978. Review. PubMed PMID: 24322524; PubMed Central PMCID: PMC3875925 5(12), 4978-89.
- 294.Kumar S R, Hosokawa M, Miyashita K. (2013) Fucoxanthin: a marine carotenoid exerting anti-cancer effects by affecting multiple mechanisms. Mar Drugs. 10.3390/md11125130. Review. PubMed PMID: 24351910; PubMed Central PMCID: PMC3877908 11(12), 5130-47.
- 295.Catarino M D, AMS Silva, Cardoso S M. (2018) Phycochemical Constituents and Biological Activities of Fucus spp. Mar Drugs. pii: E249. doi: 10.3390/md16080249. Review. PubMed PMID: 30060505; PubMed Central PMCID: PMC6117670 16(8).
- 296.Almeida T P, Ferreira J, Vettorazzi A, Azqueta A, Rocha E et al. (2018) Cytotoxic activity of fucoxanthin, alone and in combination with the cancer drugs imatinib and doxorubicin, in CML cell lines. Environ Toxicol Pharmacol. Apr;59: 24-33. doi: 10.1016/j.etap.2018.02.006. Epub 2018 Feb 16. PubMed PMID: 29518678.
- 297.Almeida T P, Ramos A A, Ferreira J, Azqueta A, Rocha E. (2019) Bioactive Compounds from Seaweed with Anti-Leukemic Activity: A Mini-Review on Carotenoids and Phlorotannins. Mini Rev Med Chem. doi: 10.2174/1389557519666190311095655. [Epub ahead of print] PubMed PMID:. 30854962.
- 298.Saikia M, Retnakumari A P, Anwar S, Anto N P, Mittal R et al. (2018) Heteronemin, a marine natural product, sensitizes acute myeloid leukemia cells towards cytarabine chemotherapy by regulating farnesylation of Ras. 10.18632/oncotarget.24771. eCollection 2018 Apr 6. PubMed PMID: 29719594; PubMed Central PMCID: PMC5915061 , Oncotarget. Apr 9(26), 18115-18127.
- 299.Esmaeilbeig M, Kouhpayeh S A, Amirghofran Z. (2015) An Investigation of the Growth Inhibitory Capacity of Several Medicinal Plants From Iran on Tumor Cell Lines. Iran J Cancer Prev. Oct;8(5):e4032. doi: 10.17795/ijcp-4032. Epub 2015 Oct 27. PubMed PMID: 26634.
- 300.Och M, Och A, Cieśla Ł, Kubrak T, Pecio Ł et al. (2015) Study of cytotoxic activity, podophyllotoxin, and deoxypodophyllotoxin content in selected Juniperus species cultivated in Poland. Pharm Biol. Epub 2015 Feb 27. PubMed PMID: 53(6), 831-7.
- 301.Erfani N, Nazemosadat Z, Moein M. (2015) Cytotoxic activity of ten algae from the Persian Gulf and Oman Sea on human breast cancer cell lines; MDA-MB-231, MCF-7, and T-47D. Pharmacognosy Res. PubMed PMID: 25829786; PubMed Central PMCID: PMC4357963 7(2), 133-7.
- 302.Joseph O A. (2016) The prospects of medicinal plants in the treatment of breast cancer. , European Pharmaceutical Review 13.
- 303.Azubuike S O, Muirhead C, Hayes L, McNally R. (2018) Rising global burden of breast cancer: the case of sub-Saharan Africa (with emphasis on Nigeria) and implications for regional development: a review. World J Surg Oncol. Review. PubMed PMID: 29566711; PubMed Central PMCID: PMC5863808 16(63), 1-13.
- 304.Blumen H, Fitch K, Polkus V. (2016) Comparison of Treatment Costs for Breast Cancer, by Tumor Stage and Type of Service. Am Health Drug Benefits. Feb;9(1): 23-32. PubMed PMID: 27066193; PubMed Central PMCID: PMC4822976 .
- 305.Alkabban F M, Ferguson T Cancer, Breast. (2019) In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing;. Available from:https://www.ncbi.nlm.nih.gov/books/NBK482286/
- 306.Mehrgou A, Akouchekian M. (2016) The importance of BRCA1 and BRCA2 genes mutations in breast cancer development.Med J Islam Repub Iran.May 15; 30: 369. eCollection 2016.Review.PubMed PMID: 27493913; PubMed Central PMCID:. 4972064.
- 307.Poehls U G, Hack C C, Wunderle M, Renner S P, Lux M P et al. (2019) Awareness of breast cancer incidence and risk factors among healthy women in Germany: an update after 10 years. Eur J Cancer Prev. 30681416.
- 308.Hendrick R E, Baker J A, Helvie M A. (2019) Breast cancer deaths averted over 3 decades. Cancer. 10.1002/cncr.31954. Epub 2019 Feb 11. PubMed PMID: 125(9), 1482-1488.
- 309.Vishwakarma G, Ndetan H, Das D N, Gupta G, Suryavanshi M et al. (2019) Reproductive factors and breast cancer risk: A meta-analysis of case-control studies in Indian women. Apr-Jun;8(2): 80-84. doi: 10.4103/sajc.sajc_317_18. PubMed PMID: 31069183; PubMed Central PMCID: PMC6498720 , South Asian.
- 310.Ng H S, Vitry A, Koczwara B, Roder D, McBride M L. (2019) Patterns of comorbidities in women with breast cancer: a Canadian population-based study. Cancer Causes Control. Epub 2019 Jul 6. PubMed PMID: 30(9), 931-941.
- 311.Bahri N, Fathi Najafi T, Homaei Shandiz F, Tohidinik H R, Khajavi A. (2019) The relation between stressful life events and breast cancer: a systematic review and meta-analysis of cohort studies. Breast Cancer Res Treat. Review. PubMed PMID: 176(1), 53-61.
- 312.Ho-Huynh A, Tran A, Bray G, Abbot S, Elston T et al. (2019) Factors influencing breast cancer outcomes in Australia: A systematic review. Jul;28(4):e13038. doi: 10.1111/ecc.13038. Epub 2019 Mar 27. Review. PubMed PMID: , Eur J Cancer Care 30919536.
- 313.Feng Y, Spezia M, Huang S, Yuan C, Zeng Z et al. (2018) Breast cancer development and progression: Risk factors, cancer stem cells, signaling pathways, genomics, and molecular pathogenesis. Genes Dis. 10.1016/j.gendis.2018.05.001. eCollection 2018 Jun. Review. PubMed PMID: 30258937; PubMed Central PMCID: PMC6147049 5(2), 77-106.
- 314.Sun Y S, Zhao Z, Yang Z N, Xu F, Lu H J et al. (2017) Risk Factors and Preventions of Breast Cancer. , Int J Biol Sci 13(11), 1387-1397.
- 315. (2006) InformedHealth.org [Internet]. Cologne, Germany: Institute for Quality and Efficiency in Health Care (IQWiG); Risk factors for breast cancer. Available from: https://www.ncbi.nlm.nih.gov/books/NBK447103/
- 316.Alexander A, Kaluve R, Prabhu J S, Korlimarla A, Srinath B S et al.. The Impact of Breast Cancer on the Patient and the Family in Indian Perspective. Indian J Palliat Care. 2019 Jan-Mar;25(1): 66-72. doi: 10.4103/IJPC.IJPC_158_18. PubMed PMID: 30820105; PubMed Central PMCID: PMC6388591 .
- 317.Chen L, Malone K E, Li C I. (2014) Bra wearing not associated with breast cancer risk: a population-based case-control study. Cancer Epidemiol Biomarkers Prev. Epub 2014 Sep 5. PubMed PMID: 25192706; PubMed Central PMCID: PMC4184992 23(10), 2181-5.
- 318.SSD Rios, ACR Chen, Chen J R. (2016) Wearing a Tight Bra for many hours a day is associated with increased risk of breast cancer. Adv Oncol Res Treat. 1, 1-5.
- 319.Virani S, Chindaprasirt J, Wirasorn K, Sookprasert A, Somintara O et al. (2018) 12. PubMed PMID: 29760320; PubMed Central PMCID:. Breast Cancer Incidence Trends and Projections in Northeastern Thailand. J Epidemiol. 2018 Jul 5;28(7): 323-330. doi: 10.2188/jea.JE20170045. Epub 6004364.
- 320.Yabroff K R, Lund J, Kepka D, Mariotto A. (2011) Economic burden of cancer in the United States: estimates, projections, and future research. Cancer Epidemiol Biomarkers Prev. PubMed PMID: 21980008; PubMed Central PMCID: PMC3191884 20(10), 2006-14.
- 321.Mariotto A B, Yabroff K R, Shao Y, Feuer E J, Brown M L. (2011) Projections of the cost of cancer care in the United States: 2010-2020. J Natl Cancer Inst. J Natl Cancer Inst. 2011 Apr 20;103(8): 699. PubMed PMID: 21228314; PubMed Central PMCID: PMC3107566 103(2), 117-28.
- 322.Iadeluca L, Mardekian J, Chander P, Hopps M, Makinson G T. (2017) The burden of selected cancers in the US: health behaviors and health care resource utilization. Cancer Manag Res. Nov28; 9: 721 - 730. doi: 10.2147/CMAR.S143148. eCollection 2017. PubMed PMID: 29238222; PubMed Central PMCID: PMC5713681 .
- 323.Montecucco A, Zanetta F, Biamonti G. (2015) Molecular mechanisms of etoposide. Review. PubMed PMID: 26600742; PubMed Central PMCID: PMC4652635 , EXCLI J. 2015 Jan19; 14, 95-108.
- 324.Benzina S, Harquail J, Jean S, Beauregard A P, Colquhoun C D et al.Deoxypodophyllotoxin isolated from Juniperus communis induces apoptosis in breast cancer cells. Anticancer Agents Med Chem. PubMed PMID: 15(1), 79-88.
- 325.Khaled M, Belaaloui G, Jiang Z Z, Zhu X, Zhang L Y. (2016) Antitumor effect of Deoxypodophyllotoxin on human breast cancer xenograft transplanted in BALB/c nude mice model. J Infect Chemother. Oct;22(10): 692-6. doi: 10.1016/j.jiac.2016.07.017. Epub 2016 Aug 28. PubMed PMID: 27578026.
- 326.Guerram M, Jiang Z Z, Sun L, Zhu X, Zhang L Y.Antineoplastic effects of deoxypodophyllotoxin, a potent cytotoxic agent of plant origin. on glioblastoma U-87 MG and SF126 cells. Pharmacol Rep. 2015 Apr;67(2): 245-52. doi: 10.1016/j.pharep.2014.10.003. Epub 2014 Oct 19. PubMed PMID: 25712646.
- 327.Zang X, Wang G, Cai Q, Zheng X, Zhang J et al. (2018) A Promising Microtubule Inhibitor Deoxypodophyllotoxin Exhibits Better Efficacy to Multidrug-Resistant Breast Cancer than Paclitaxel via Avoiding Efflux Transport. Drug Metab Dispos. May;46(5): 542-551. doi: 10.1124/dmd.117.079442. Epub 2018 Mar 9. PubMed PMID: 29523600.
- 328.S Van, Daniels A L, Hooten C J, Brock S L, Jenkins A R et al. (2007) Effects of crude aqueous medicinal plant extracts on growth and invasion of breast cancer cells. Oncol Rep. PubMed PMID: 17(6), 1487-92.
- 329.Kamata H, Sadahiro S, Yamori T. (2019) Discovery of Inhibitors of Membrane Traffic from a Panel of Clinically Effective Anticancer Drugs. Biol Pharm Bull. Epub 2019 Feb 21. PubMed PMID: 42(5), 814-818.
- 330.Mavrogiannis A V, Kokkinopoulou I, Kontos C K, Sideris D C.Effect of Vinca Alkaloids on the Expression Levels of microRNAs Targeting Apoptosis-related Genes in Breast Cancer Cell Lines. PubMed PMID: , Curr Pharm Biotechnol 19(13), 1076-1086.
- 331.Wong M Y, Chiu G N. (2010) Simultaneous liposomal delivery of quercetin and vincristine for enhanced estrogen-receptor-negative breast cancer treatment. Anticancer Drugs. Apr;21(4): 401-10. doi: 10.1097/CAD.0b013e328336e940. PubMed PMID: 20110806.
- 332.Su M, Zhao M, Luo Y, Lin X, Xu L et al. (2011) Evaluation of the efficacy, toxicity and safety of vinorelbine incorporated in a lipid emulsion. doi: 10.1016/j.ijpharm.2011.03.028. Epub 2011 Mar 21. PubMed PMID: , Int 21421039.
- 333.Ghersi D, Willson M L, Chan M M, Simes J, Donoghue E et al. (2015) Taxane-containing regimens for metastatic breast cancer. Cochrane Database Syst Rev. 10;(6):CD003366. doi: 10.1002/14651858.CD003366.pub3. Review. PubMed PMID: 26058962; PubMed Central PMCID: PMC6464903 .
- 334.Bachegowda L S, Makower D F, Sparano J A. (2014) Taxanes: impact on breast cancer therapy. Anticancer Drugs. May;25(5): 512-21. doi: 10.1097/CAD.0000000000000090. PubMed PMID: 24552749.
- 335.Alken S, Kelly C M. (2013) Benefit risk assessment and update on the use of docetaxel in the management of breast cancer. Cancer Manag Res. 14;5: 357-65. doi: 10.2147/CMAR.S49321. Review. PubMed PMID: 24143122; PubMed Central PMCID: PMC3798099 .
- 336.Habib S, Delourme J, Dhalluin X, Petyt G, Tacelli N et al. (2013) Bevacizumab and weekly paclitaxel for non-squamous non small cell lung cancer patients: a retrospective study. Lung Cancer. May;80(2): 197-202. doi: 10.1016/j.lungcan.2013.01.015. Epub 2013 Feb 14. PubMed PMID: 23414642.
- 337.Joris S, Fontaine C, Decoster L, Vanacker L, Schallier D et al. (2019) Retrospective comparison of two consecutive cohorts of adjuvant chemotherapy regimens of cyclophosphamide with either docetaxel or paclitaxel in older patients with early breast cancer. Jul;25(4): 663-666. doi: 10.1111/tbj.13306. Epub 2019 May 9. PubMed PMID: , Breast 31074007.
- 338.Liu Y, Xu Z, Zhang Z, Wen G, Sun J et al. (2019) Efficacy and safety of TE/TEC/intensive paclitaxel neoadjuvant chemotherapy for the treatment of breast cancer. Oncol Lett. Jan;17(1): 907-912. doi: 10.3892/ol.2018.9658. Epub 2018 Nov 1. PubMed PMID: 30655846; PubMed Central PMCID: PMC6312931 .
- 339.Bachelot T, Ciruelos E, Schneeweiss A, Puglisi F, Peretz-Yablonski T et al. (2019) PERUSE investigators . Preliminary safety and efficacy of first-line pertuzumab combined with trastuzumab and taxane therapy for HER2-positive locally recurrent or metastatic breast cancer (PERUSE). Ann Oncol. 10.1093/annonc/mdz061. PubMed PMID: 30(5), 766-773.
- 340.Nyrop K A, Deal A M, Reeder-Hayes K E, Shachar S S, Reeve B B et al. (2019) Patient-reported and clinician-reported chemotherapy-induced peripheral neuropathy in patients with early breast cancer: Current clinical practice. , Cancer 125(17), 2945-2954.
- 341.Hojo T, Masuda N, Iwamoto T, Niikura N, Anan K et al. (2019) Taxane-based combinations as adjuvant chemotherapy for node-positive ER-positive breast cancer based on data from the Breast Cancer Registry of the Japanese Breast Cancer Society. Breast Cancer. 31327134.
- 342.Ntellas P, Spathas N, Agelaki S, Zintzaras E, Saloustros E. (2019) Taxane & cyclophosphamide vs anthracycline & taxane-based chemotherapy as adjuvant treatment for breast cancer: a pooled analysis of randomized controlled trials by the Hellenic Academy of Oncology. Oncotarget. 10.18632/oncotarget.26632. eCollection 2019 Feb 5. PubMed PMID: 30838092; PubMed Central PMCID: PMC6383821 10(11), 1209-1216.
- 343.Kubatka P, Uramova S, Kello M, Kajo K, Kruzliak P et al. (2017) Antineoplastic effects of clove buds (Syzygium aromaticum L.) in the model of breast carcinoma. J Cell Mol Med. Nov;21(11): 2837-2851. doi: 10.1111/jcmm.13197. Epub 5661249.
- 344.Legault J, Pichette A. (2007) Potentiating effect of beta-caryophyllene on anticancer activity of alpha-humulene, isocaryophyllene and paclitaxel. J Pharm Pharmacol. Dec;59(12): 1643-7. PubMed PMID: 18053325.
- 345.Park K R, Nam D, Yun H M, Lee S G, Jang H J et al. (2011) β-Caryophyllene oxide inhibits growth and induces apoptosis through the suppression of PI3K/AKT/mTOR/S6K1 pathways and ROS-mediated MAPKs activation. Cancer Lett. 10.1016/j.canlet.2011.08.001. Epub 2011 Aug 26. PubMed PMID: 312(2), 178-88.
- 346.Kim C, Cho S K, Kapoor S, Kumar A, Vali S et al. (2014) β-Caryophyllene oxide inhibits constitutive and inducible STAT3 signaling pathway through induction of the SHP-1 protein tyrosine phosphatase. Mol Carcinog. Oct;53(10): 793-806. doi: 10.1002/mc.22035. Epub 2013 Jun 13. PubMed PMID: 23765383.
- 347.Vidhya N, Devaraj S N. (2011) Induction of apoptosis by eugenol in human breast cancer cells. Nov;49(11): 871-8. PubMed PMID: , Indian J Exp Biol 22126019.
- 348.Sigurdsson S, Ogmundsdottir H M, Hallgrimsson J, Gudbjarnason S.Antitumour activity of Angelica archangelica leaf extract. In Vivo. 2005 Jan-Feb;19(1): 191-4. PubMed PMID: 15796173.
- 349.Motaghed M, Al-Hassan F M, Hamid S S. (2013) Cellular responses with thymoquinone treatment in human breast cancer cell line MCF-7. Pharmacognosy Res. PubMed PMID: 23900121; PubMed Central PMCID: PMC3719263 10-4103.
- 350.Eggenschwiler J, L von Balthazar, Stritt B, Pruntsch D, Ramos M et al. (2007) Mistletoe lectin is not the only cytotoxic component in fermented preparations of Viscum album from white fir (Abies pectinata). BMC Complement Altern Med. 1878504.
- 351.Thronicke A, Oei S L, Merkle A, Matthes H, Schad F. (2018) Clinical Safety of Combined Targeted and Viscum album L. Therapy in Oncological Patients. Medicines. 6;5(3). pii: E100. doi: 10.3390/medicines5030100. PubMed PMID: 30200590; PubMed Central PMCID: PMC6164814 , (Basel) .
- 352.Weissenstein U, Kunz M, Urech K, Regueiro U, Baumgartner S.Interaction of a standardized mistletoe (Viscum album) preparation with antitumor effects of Trastuzumab. in vitro. BMC Complement Altern Med. 2016 Aug 4;16: 271. doi: 10.1186/s12906-016-1246-2. PubMed PMID: 27491866; PubMed Central PMCID: PMC4973521 .
- 353.Beuth J, Ko H L, Schneider H, Tawadros S, Kasper H U et al. (2006) Intratumoral application of standardized mistletoe extracts down regulates tumor weight via decreased cell proliferation, increased apoptosis and necrosis in a murine model. Anticancer Res. Nov-Dec;26(6B): 4451-6. PubMed PMID: 17201168.
- 354.Kienle G S, Glockmann A, Schink M, Kiene H. (2009) Viscum album L. extracts in breast and gynaecological cancers: a systematic review of clinical and preclinical research. J Exp Clin Cancer Res. Review. PubMed PMID: 19519890; PubMed Central PMCID: PMC2711058 28(79), 1-33.
- 355.Harmsma M, Grommé M, Ummelen M, Dignef W, Tusenius K J et al. (2004) Differential effects of Viscum album extract IscadorQu on cell cycle progression and apoptosis in cancer cells. Dec;25(6): 1521-9. PubMed PMID: , Int 15547686.
- 356.Tai C J, Liu C H, Pan Y C, Wong S H, Tai C J et al. (2019) Chemovirotherapeutic Treatment Using Camptothecin Enhances Oncolytic Measles Virus-Mediated Killing of Breast Cancer Cells. Sci Rep. PubMed PMID: 31043633; PubMed Central PMCID: PMC6494908 9(1), 6767-10.
- 357.Venditti A, Maggi F, Quassinti L, Bramucci M, Lupidi G et al. (2018) Bioactive Constituents of Juniperus turbinata Guss. from La Maddalena Archipelago. Chem Biodivers. Aug;15(8):e1800148. doi: 10.1002/cbdv.201800148. Epub 2018 Jun 28. PubMed PMID: 29790302.
- 358.Ben Mrid R, Bouchmaa N, Bouargalne Y, Ramdan B, Karrouchi K et al.Phytochemical Characterization, Antioxidant and. In Vitro Cytotoxic Activity Evaluation of Juniperus oxycedrus Subsp. oxycedrus Needles and Berries. Molecules. 2019 Jan 30;24(3). pii: E502. doi: 10.3390/molecules24030502. PubMed PMID: 30704127; PubMed Central PMCID: PMC6384603 .
- 359.Bayala B, Bassole I H, Scifo R, Gnoula C, Morel L et al. (2014) Anticancer activity of essential oils and their chemical components - a review. Am J Cancer Res. 4(6), 591-607.
- 360.Wang Y, Sun H, Xiao Z, Zhang G, Zhang D et al. (2018) DNA damage and apoptosis induced by a potent orally podophyllotoxin derivative in breast cancer. Cell Commun Signal. PubMed PMID: 30176902; PubMed Central PMCID: PMC6122736 16(52), 1-13.
- 361.Zilla M K, Nayak D, Amin H, Nalli Y, Rah B et al.4'-Demethyl-deoxypodophyllotoxin glucoside isolated from Podophyllum hexandrum exhibits potential anticancer activities by altering. Chk-2 signaling pathway in MCF-7 breast cancer cells. Chem Biol Interact. 2014 Dec 5;224: 100-7. doi: 10.1016/j.cbi.2014.09.022. Epub 2014 Oct 18. PubMed PMID: 25446499.
- 362.Mukund V, Saddala M S, Farran B, Mannavarapu M, Alam A et al. (2019) Molecular docking studies of angiogenesis target protein HIF-1α and genistein in breast. Epub 2019 Mar 28. PubMed PMID: 15, 169-172.
- 363.Yu S, Zhu L, Wang K, Yan Y, He J et al. (2019) Green tea consumption and risk of breast cancer: A systematic review and updated meta-analysis of case-control studies. Medicine (Baltimore). Jul;98(27):e16147. doi: 10.1097/MD.0000000000016147. PubMed PMID: 31277115; PubMed Central PMCID: PMC6635178 .
- 364.Stuart E C, Scandlyn M J, Rosengren R J. (2006) Role of epigallocatechin gallate (EGCG) in the treatment of breast and prostate cancer. Life Sci. Epub 2006 Aug 5. Review. PubMed PMID: 79(25), 2329-36.
- 365.Green. (2019) Tea Catechin Extract Supplementation Does Not Influence Circulating Sex Hormones and Insulin-Like Growth Factor Axis Proteins in a Randomized Controlled Trial of Postmenopausal Women at High Risk of Breast. PubMed PMID: 30926986; PubMed Central PMCID: PMC6461722 149(4), 619-627.
- 366.Khan N, Mukhtar H. (2018) Tea Polyphenols in Promotion of Human Health. Nutrients. E39. doi: 10.3390/nu11010039. Review. PubMed PMID: 30585192; PubMed Central PMCID: PMC6356332 11(1).
- 367.Schröder L, Marahrens P, Koch J G, Heidegger H, Vilsmeier T et al. (2019) Effects of green tea, matcha tea and their components epigallocatechin gallate and quercetin on MCF7 and MDA-MB-231 breast carcinoma cells. Oncol Rep. Jan;41(1): 387-396. doi: 10.3892/or.2018.6789. Epub 2018 Oct 12. PubMed PMID: 30320348.
- 368.Zhang J Y, Liao Y H, Lin Y, Liu Q, Xie X M et al. (2019) Effects of tea consumption and the interactions with lipids on breast cancer survival. Breast Cancer Res Treat. 176(3), 679-686.
- 369.Najaf, Salehi M, Ghazanfarpour M, Hoseini Z S, Khadem-Rezaiyan M. (2018) The association between green tea consumption and breast cancer risk: A systematic review and meta-analysis. Phytother Res. Oct;32(10): 1855-1864. doi: 10.1002/ptr.6124. Epub 2018 Jun 7. Review. PubMed PMID: 29876987.
- 370.Gianfredi V, Nucci D, Abalsamo A, Acito M, Villarini M et al. (2018) Tea Consumption and Risk of Breast Cancer and Recurrence-A Systematic Review and Meta-Analysis of Observational Studies. 3;10(12). pii: E1886. doi: 10.3390/nu10121886. PubMed PMID: 30513889; PubMed Central PMCID: PMC6316745 , Nutrients .
- 371.Cai Z Y, Li X M, Liang J P, Xiang L P, Wang K R et al.. Bioavailability of Tea Catechins and Its Improvement. Molecules. 2018 Sep 13;23(9). pii: E2346. doi: 10.3390/molecules23092346. Review. PubMed PMID: 30217074; PubMed Central PMCID: PMC6225109 .
- 372.Iwasaki M, Mizusawa J, Kasuga Y, Yokoyama S, Onuma H et al.Green tea consumption and breast cancer risk in Japanese women: a case-control study. Epub 2013 Nov 25. PubMed PMID: , Nutr Cancer 66(1), 57-67.
- 373.Shirakami Y, Shimizu M. (2018) Possible Mechanisms of Green Tea and Its Constituents against Cancer. Molecules. E2284. doi: 10.3390/molecules23092284. Review. PubMed PMID: 30205425; PubMed Central PMCID: PMC6225266 23(9).
- 374.Sahin I, Bilir B, Ali S, Sahin K, Kucuk O. (2019) Soy Isoflavones in Integrative Oncology: Increased Efficacy and Decreased Toxicity of Cancer Therapy. Integr Cancer Ther. PubMed PMID: 30897972; PubMed Central PMCID: PMC6431760 , Jan-Dec; 18, 1534735419835310-10.
- 375.Wu S Y, Wu A T, Yuan K S, Liu S H. (2016) Brown Seaweed Fucoidan Inhibits Cancer Progression by Dual Regulation of mir-29c/ADAM12 and miR-17-5p/PTEN Axes in Human Breast Cancer Cells. J Cancer.7(15): 2408-2419.eCollection 2016. PubMed PMID: 27994679; PubMed Central PMCID:. 5166552.
- 376.Moussavou G, Kwak D H, Obiang-Obonou B W, Maranguy C A, Dinzouna-Boutamba S D et al. (2014) Anticancer effects of different seaweeds on human colon and breast cancers. Mar Drugs. 10.3390/md12094898. Review. PubMed PMID: 25255129; PubMed Central PMCID: PMC4178489 12(9), 4898-911.
- 377.Montuori N, Pesapane A, Rossi F W, Giudice V. (2016) Urokinase type plasminogen activator receptor (uPAR) as a new therapeutic target in cancer. Transl Med UniSa. 15-21. eCollection 2016 Nov. PubMed PMID: 27896223; PubMed Central PMCID: PMC5120746 , De.
- 378.Teas J, Vena S, Cone D L, Irhimeh M. (2013) The consumption of seaweed as a protective factor in the etiology of breast cancer: proof of principle. Jun;25(3): 771-779. Epub 2012 Nov 10. PubMed PMID: 23678231; PubMed Central PMCID: PMC3651528 , J Appl Phycol.
- 379.Shamsabadi F T, Khoddami A, Fard S G, Abdullah R, Othman H H et al.Comparison of tamoxifen with edible seaweed (Eucheuma cottonii L.) extract in suppressing breast tumor. PubMed PMID: , Nutr Cancer 65(2), 255-62.
- 380.Jazzara M, Ghannam A, Soukkarieh C, Murad H.Anti-Proliferative Activity of λ-Carrageenan Through the Induction of Apoptosis in Human Breast Cancer Cells. , Int J Cancer Manag 9(4), 1-8.
- 381.Groult H, Cousin R, Chot-Plassot C, Maura M, Bridiau N et al.. λ-Carrageenan Oligosaccharides of Distinct Anti-Heparanase and Anticoagulant Activities Inhibit MDA-MB-231 Breast Cancer Cell Migration. Mar Drugs. 2019 Feb 27;17(3). pii: E140. doi: 10.3390/md17030140. PubMed PMID: 30818840; PubMed Central PMCID: PMC6471403 .
- 382.Losada-Echeberría M, Herranz-López M, Micol V, Barrajón-Catalán E. (2017) Polyphenols as Promising Drugs against Main Breast Cancer Signatures. Antioxidants. pii: E88. doi: 10.3390/antiox6040088. Review. PubMed PMID: 29112149; PubMed Central PMCID: PMC5745498 , (Basel) 6(4).
- 383.Antioxidant antiproliferative. (2013) and antiangiogenesis effects of polyphenol-rich seaweed (Sargassum muticum). Biomed Res Int. Epub 2013 Sep 4. PubMed PMID: 24078922; PubMed Central PMCID: PMC3776361 10-1155.
- 384.Niedzwiecki A, Roomi M W, Kalinovsky T, Rath M. (2016) Anticancer Efficacy of Polyphenols and Their Combinations. Nutrients. 9;8(9). pii: E552. doi: 10.3390/nu8090552. Review. PubMed PMID: 27618095; PubMed Central PMCID: PMC5037537 .
- 385.Kapinova A, Kubatka P, Golubnitschaja O, Kello M, Zubor P et al. (2018) Dietary phytochemicals in breast cancer research: anticancer effects and potential utility for effective chemoprevention. Environ Health Prev Med. Review. PubMed PMID: 30092754; PubMed Central PMCID: PMC6085646 23(36), 1-18.
- 386.Keating E, Martel F. (2018) Antimetabolic Effects of Polyphenols in Breast Cancer Cells: Focus on Glucose Uptake and Metabolism. Front Nutr. 16;5: 25. doi: 10.3389/fnut.2018.00025. eCollection 2018. Review. PubMed PMID: 29713632; PubMed Central PMCID: PMC5911477 .
- 387.Sudhakaran M, Sardesai S, Doseff A I. (2019) Flavonoids: New Frontier for Immuno-Regulation and Breast Cancer Control. Antioxidants (Basel). pii: E103. doi: 10.3390/antiox8040103. Review. PubMed PMID: 30995775; PubMed Central PMCID: PMC6523469 8(4).
- 388.Hui C, Qi X, Qianyong Z, Xiaoli P, Jundong Z et al.flavonoid subclasses and breast cancer risk: a meta-analysis of epidemiologic studies. 10.1371/journal.pone.0054318. Epub 2013 Jan 18. PubMed PMID: 23349849; PubMed Central PMCID: PMC3548848 , PLoS One 8(1).
- 389.Sak K. (2017) Epidemiological Evidences on Dietary Flavonoids and Breast Cancer Risk: A Narrative Review. Asian Pac J Cancer Prev. PubMed PMID: 28950673; PubMed Central PMCID: PMC5720631 18(9), 2309-2328.
- 390.Takemura H, Sakakibara H, Yamazaki S, Shimoi K.Breast cancer and flavonoids - a role in prevention. Review. PubMed PMID: , Curr Pharm Des 19(34), 6125-32.
- 391.Batra P, Sharma A K. (2013) Anti-cancer potential of flavonoids: recent trends and future perspectives. 3 Biotech. 3(6), 439-459.
- 392.Magne Nde CB, Zingue S, Winter E, Creczynski-Pasa T B, Michel T et al.Breast Cancer Chemopreventive and/or Chemotherapeutic Agents. Review. PubMed PMID: , Curr Med Chem 22(30), 3434-46.
- 393.Abotaleb M, Samuel S M, Varghese E, Varghese S, Kubatka P et al. (2018) Flavonoids in Cancer and Apoptosis. Cancers. pii: E28. doi: 10.3390/cancers11010028. Review. PubMed PMID: 30597838; PubMed Central PMCID: PMC6357032 , (Basel) 11(1).
- 394.Pang B B, Chu Y K, Yang H. (2018) [Anti-breast cancer mechanism of flavonoids]. Zhongguo Zhong Yao Za Zhi. Mar;43(5): 913-920. doi: 10.19540/j.cnki.cjcmm.20171211.005. Review. Chinese. PubMed PMID: 29676087.
- 395.Zhang H W, Hu J J, Fu R Q, Liu X, Zhang Y H et al. (2018) Flavonoids inhibit cell proliferation and induce apoptosis and autophagy through downregulation of PI3Kγ mediated PI3K/AKT/mTOR/p70S6K/ULK signaling pathway in human breast cancer cells. Sci Rep. PubMed PMID: 30050147; PubMed Central PMCID: PMC6062549 8, 1-13.
- 396.Rodríguez-García C, Sánchez-Quesada C, J Gaforio. (2019) Dietary Flavonoids as Cancer Chemopreventive Agents: An Updated Review of Human Studies. Antioxidants. pii: E137. doi: 10.3390/antiox8050137. Review. PubMed PMID: 31109072; PubMed Central PMCID: PMC6562590 , (Basel) 8(5).
- 397.Abudabbus A, Badmus J A, Shalaweh S, Bauer R, Hiss D.. Effects of Fucoidan and Chemotherapeutic Agent Combinations on Malignant and Non-malignant Breast Cell Lines. Curr Pharm Biotechnol 18(9), 748-757.
- 398.Zhang J, Riby J E, Conde L, Grizzle W E, Cui X et al. (2016) A Fucus vesiculosus extract inhibits estrogen receptor activation and induces cell death in female cancer cell lines. BMC Complement Altern Med. PubMed PMID: 27234961; PubMed Central PMCID: PMC4884380 16(151), 1-9.
- 399.Moussavou G, Kwak D H, Obiang-Obonou B W, Maranguy C A, Dinzouna-Boutamba S D et al. (2014) Anticancer effects of different seaweeds on human colon and breast cancers. Mar Drugs. 10.3390/md12094898. Review. PubMed PMID: 25255129; PubMed Central PMCID: PMC4178489 12(9), 4898-911.
- 400.Atashrazm F, Lowenthal R M, Woods G M, Holloway A F, Dickinson J L. (2015) Fucoidan and cancer: a multifunctional molecule with anti-tumor potential. Mar Drugs. 10.3390/md13042327. Review. PubMed PMID: 25874926; PubMed Central PMCID: PMC4413214 13(4), 2327-46.
- 401.Lu J, Shi K K, Chen S, Wang J, Hassouna A et al. (2018) Fucoidan Extracted from the New Zealand Undaria pinnatifida-Physicochemical Comparison against Five Other Fucoidans: Unique Low Molecular Weight Fraction Bioactivity in Breast Cancer Cell Lines. Mar Drugs. pii: E461. doi: 10.3390/md16120461. PubMed PMID: 30469516; PubMed Central PMCID: PMC6316445 16(12).
- 402.Zorofchian Moghadamtousi S, Karimian H, Khanabdali R, Razavi M, Firoozinia M et al.Anticancer and antitumor potential of fucoidan and fucoxanthin, two main metabolites isolated from brown algae. ScientificWorldJournal. 2014 Jan 2;2014: 768323. doi: 10.1155/2014/768323. eCollection 2014. Review. PubMed PMID: 24526922; PubMed Central PMCID: PMC3910333 .
- 403.Xue M, Ge Y, Zhang J, Wang Q, Hou L et al.Anticancer properties and mechanisms of fucoidan on mouse breast cancer in vitro and in vivo. PLoS One. 2012;7(8):e43483. doi: 10.1371/journal.pone.0043483. Epub 2012 Aug 20. PubMed PMID: 22916270; PubMed Central PMCID: PMC3423341 .
- 404.Pawar V K, Singh Y, Sharma K, Shrivastav A, Sharma A et al. (2019) Improved chemotherapy against breast cancer through immunotherapeutic activity of fucoidan decorated electrostatically assembled nanoparticles bearing doxorubicin. 10.1016/j.ijbiomac.2018.09.059. Epub 2018 Sep 13. PubMed PMID: , Int J Biol Macromol 122(1), 1100-1114.
- 405.He X, Xue M, Jiang S, Li W, Yu J et al.Fucoidan Promotes Apoptosis and Inhibits. PubMed PMID: , EMT of Breast Cancer Cells. Biol Pharm Bull 42(3), 442-447.
- 406.Xue M, Ge Y, Zhang J, Liu Y, Wang Q et al.Fucoidan inhibited 4T1 mouse breast cancer cell growth in vivo and in vitro via downregulation of Wnt/β-catenin signaling. PubMed PMID: , Nutr Cancer 65(3), 460-8.
- 407.Xue M, Ji X, Liang H, Liu Y, Wang B et al. (2018) The effect of fucoidan on intestinal flora and intestinal barrier function in rats with breast cancer. Food Funct. PubMed PMID: 9(2), 1214-1223.
- 408.Oliveira C, Neves N M, Reis R L, Martins A, Silva T H. (2018) Gemcitabine delivered by fucoidan/chitosan nanoparticles presents increased toxicity over human breast cancer cells. Nanomedicine (Lond). Epub 2018 Sep 7. PubMed PMID: 13(16), 2037-2050.
- 409.Gong X, Smith J R, Swanson H M, Rubin L P. (2018) Carotenoid Lutein Selectively Inhibits Breast Cancer Cell Growth and Potentiates the Effect of Chemotherapeutic Agents through ROS-Mediated Mechanisms. Molecules. 14;23(4). pii: E905. doi: 10.3390/molecules23040905. PubMed PMID: 29662002; PubMed Central PMCID: PMC6017803 .
- 410.Chang J, Zhang Y, Li Y, Lu K, Shen Y et al. (2018) NrF2/ARE and NF-κB pathway regulation may be the mechanism for lutein inhibition of human breast cancer cell. Future Oncol. PubMed PMID: 14(8), 719-726.
- 411.Mignone L I, Giovannucci E, Newcomb P A, Titus-Ernstoff L, Trentham-Dietz A et al. (2009) Dietary carotenoids and the risk of invasive breast cancer. 10.1002/ijc.24334. PubMed PMID: 19330841; PubMed Central PMCID: PMC3564658 , Int 124(12), 2929-37.
- 412.Li Y, Zhang Y, Liu X, Wang M, Wang P et al. (2018) Lutein inhibits proliferation, invasion and migration of hypoxic breast cancer cells via downregulation of HES1. Jun;52(6): 2119-2129. doi: 10.3892/ijo.2018.4332. Epub 2018 Mar 23. PubMed PMID: , Int 29620169.
- 413.Yan B, Lu M S, Wang L, Mo X F, Luo W P et al. (2016) Specific serum carotenoids are inversely associated with breast cancer risk among Chinese women: a case-control study. 10.1017/S000711451500416X. Epub 2015 Oct 20. PubMed PMID: , Br 115(1), 129-37.
- 414.DHA Rocha, AML Seca, DCGA Pinto. (2018) Seaweed Secondary Metabolites In Vitro and In Vivo Anticancer Activity. Mar Drugs. pii: E410. doi: 10.3390/md16110410. Review. PubMed PMID: 30373208; PubMed Central PMCID: PMC6266495 16(11).
- 415.Erfani N, Nazemosadat Z, Moein M. (2015) Cytotoxic activity of ten algae from the Persian Gulf and Oman Sea on human breast cancer cell lines; MDA-MB-231, MCF-7, and T-47D. Pharmacognosy Res. PubMed PMID: 25829786; PubMed Central PMCID: PMC4357963 7(2), 133-7.
- 416.Li Y X, Himaya S W, Dewapriya P, Zhang C, Kim S K. (2013) Fumigaclavine C from a marine-derived fungus Aspergillus fumigatus induces apoptosis in MCF-7 breast cancer cells. Mar Drugs. 10.3390/md11125063. PubMed PMID: 24351905; PubMed Central PMCID: PMC3877903 11(12), 5063-86.
- 417.Dyshlovoy S A, Honecker F. (2015) Marine Compounds and Cancer: Where Do We Stand? Mar Drugs. Sep;13(9): 5657-65. Epub 2015 Sep 2. PubMed PMID: 26540740; PubMed Central PMCID: PMC4584346 .
- 418.Vaikundamoorthy R, Krishnamoorthy V, Vilwanathan R, Rajendran R. (2018) Structural characterization and anticancer activity (MCF7 and MDA-MB-231) of polysaccharides fractionated from brown seaweed Sargassum wightii. May;111: 1229-1237. doi: 10.1016/j.ijbiomac.2018.01.125. Epub 2018 Feb 19. PubMed PMID: , Int J Biol Macromol 29415413.
- 419.Sithranga Boopathy N, Kathiresan K. (2010) Anticancer drugs from marine flora: an overview. J Oncol. Epub 2011 Feb 27. PubMed PMID: 21461373; PubMed Central PMCID: PMC3065217 21, 41-86.
- 420.Abd-Ellatef G F, Ahmed O M, Abdel-Reheim E S, Abdel-Hamid A Z. (2017) Ulva lactuca polysaccharides prevent Wistar rat breast carcinogenesis through the augmentation of apoptosis, enhancement of antioxidant defense system, and suppression of inflammation. , Breast Cancer (Dove Med Press); 9, 67-83.
- 421.Fedorov S N, Ermakova S P, Zvyagintseva T N, Stonik V A. (2013) Anticancer and cancer preventive properties of marine polysaccharides: some results and prospects. Mar Drugs. 10.3390/md11124876. PubMed PMID: 24317475; PubMed Central PMCID: PMC3877892 11(12), 4876-901.
- 422.Isolation. (2018) Structural characterization, and antiproliferative activity of phycocolloids from the red seaweed Laurencia papillosa on MCF-7 human breast cancer cells. Mar;108: 916-926. doi: 10.1016/j.ijbiomac.2017.11.001. Epub 2017 Nov 4. PubMed PMID: , Int J Biol Macromol 29113895.
- 423.Vishchuk O S, Ermakova S P, Zvyagintseva T N. (2011) Sulfated polysaccharides from brown seaweeds Saccharina japonica and Undaria pinnatifida: isolation, structural characteristics, and antitumor activity. Carbohydr Res. 10.1016/j.carres.2011.09.034. Epub 2011 Oct 5. PubMed PMID: 346(17), 2769-76.
- 424.Vaseghi G, Sharifi M, Dana N, Ghasemi A, Yegdaneh A. (2018) Cytotoxicity of Sargassum angustifolium Partitions against Breast and Cervical Cancer Cell Lines. Adv Biomed Res. 27;7: 43. doi: 10.4103/abr.abr_259_16. eCollection 2018. PubMed PMID: 29657928; PubMed Central PMCID: PMC5887695 .
- 425.Kim E K, Tang Y, Kim Y S, Hwang J W, Choi E J et al. (2015) First evidence that Ecklonia cava-derived dieckol attenuates MCF-7 human breast carcinoma cell migration. Mar Drugs. 10.3390/md13041785. PubMed PMID: 25830682; PubMed Central PMCID: PMC4413187 13(4), 1785-97.
- 426.Araghi M, Soerjomataram I, Jenkins M, Brierley J, Morris E et al. (2019) Global trends in colorectal cancer mortality: projections to the year 2035. Int. 10.1002/ijc.32055. Epub 2019 Jan 8. PubMed PMID: 144(12), 2992-3000.
- 427.Recio-Boiles A, Waheed A, Cagir B Cancer, Colon. (2019) In: StatPearls [Internet]. Treasure Island (FL): StatPearls, Available from:https://www.ncbi.nlm.nih.gov/books/NBK470380/.
- 428.Virk G S, Jafri M, Ashley C. (2019) Colonoscopy and colorectal cancer rates among octogenarians and nonagenarians: nationwide study of US veterans. , Clin Interv Aging.; 14, 609-614.
- 429.Screening PDQ, Prevention Editorial Board. (2019) Colorectal Cancer Prevention (PDQ®): Health Professional Version. PDQ Cancer Information Summaries [Internet]. Bethesda (MD): National Cancer Institute (US); Available from: https://www.ncbi.nlm.nih.gov/books/NBK65779/ .
- 430.Chen W, Zheng R, Baade P D, Zhang S, Zeng H et al. (2015) Cancer statistics in China. PubMed PMID: , CA Cancer 66(2), 115-32.
- 431.Araghi M, Soerjomataram I, Bardot A, Ferlay J, Cabasag C J et al. (2019) Changes in colorectal cancer incidence in seven high-income countries: a population-based study. Lancet Gastroenterol Hepatol. Aug;4(8):e8. PubMed PMID: 4(7), 511-518.
- 432.AJD Wray, Minaker L M. (2019) Is cancer prevention influenced by the built environment? A multidisciplinary scoping review. , Cancer 31287585.
- 433.Poirier A E, Ruan Y, Walter S D, Franco E L, Villeneuve P J et al. (2019) DR; ComPARe Study Team. The future burden of cancer in Canada: Long-term cancer incidence projections 2013-2042. Cancer Epidemiol. Apr;59: 199-207. doi: 10.1016/j.canep.2019.02.011. Epub 2019 Mar 1. PubMed PMID: 30831552.
- 434.Poirier A E, Ruan Y, Hebert L A, Grevers X, Walter S D et al. (2019) Friedenreich CM; ComPARe Study Team. Estimates of the current and future burden of cancer attributable to low fruit and vegetable consumption in Canada. Prev Med. May;122: 20-30. doi: 10.1016/j.ypmed.2019.03.013. Erratum in: Prev Med. 2019 Aug;125: 79. PubMed PMID: 31078169.
- 435.Feletto E, Yu X Q, Lew J B, St John DJB, Jenkins M A et al.. Trends in Colon and Rectal Cancer Incidence in Australia from 1982 to 2014: Analysis of Data on Over 375,000 Cases. Cancer Epidemiol Biomarkers Prev. 2019 Jan;28(1): 83-90.
- 436.Jenkins M A, Ait Ouakrim D, Boussioutas A, Hopper J L, Ee H C et al. (2018) Revised Australian national guidelines for colorectal cancer screening: family history. , Med 209(10), 455-460.
- 437.Glover M, Mansoor E, Panhwar M, Parasa S, Cooper G S. (2019) . Epidemiology of Colorectal Cancer in Average Risk Adults 20-39 Years of Age: A Population-Based National Study. Dig Dis Sci [Epub ahead of print] PubMed PMID: 1-8.
- 438.Siegel R L, Medhanie G A, Fedewa S A, Jemal A. (1995) State variation in early-onset colorectal cancer in the United States. 29. pii: djz098. doi: 10.1093/jnci/djz098. [Epub ahead of print] PubMed PMID: , J Natl Cancer Inst 31141602.
- 439.Mannucci A, Zuppardo R A, Rosati R, Leo M D, Perea J et al. (2019) Colorectal cancer screening from 45 years of age: Thesis, antithesis and synthesis. 10.3748/wjg.v25.i21.2565. Review. PubMed PMID: 31210710; PubMed Central PMCID: PMC6558439 25(21), 2565-2580.
- 440.Erdrich J, Zhang X, Giovannucci E, Willett W. (2015) Proportion of colon cancer attributable to lifestyle in a cohort of US women. Cancer Causes Control. 26(9), 1271-1279.
- 441.Aleksandrova K, Pischon T, Jenab M, Bueno-de-Mesquita H B, Fedirko V et al. (2014) Combined impact of healthy lifestyle factors on colorectal cancer: a large European cohort study. BMC Med. PubMed PMID: 25319089; PubMed Central PMCID: PMC4192278 12(168), 1-15.
- 442.Jeon J, Du M, Schoen R E, Hoffmeister M, Newcomb P A et al.. Colorectal Transdisciplinary Study and Genetics and Epidemiology of Colorectal Cancer Consortium. Determining Risk of Colorectal Cancer and Starting Age of Screening Based on Lifestyle, Environmental, and Genetic Factors. Gastroenterology. 2018 Jun;154(8): 2152-2164.e19. doi: 10.1053/j.gastro.2018.02.021. Epub 2018 Feb 17. PubMed PMID: 29458155; PubMed Central PMCID: PMC5985207 .
- 443.Oruç Z, Kaplan M A. (2019) Effect of exercise on colorectal cancer prevention and treatment. World J Gastrointest Oncol. 10.4251/wjgo.v11.i5.348. Review. PubMed PMID: 31139306; PubMed Central PMCID: PMC6522766 11(5), 348-366.
- 444.Bradbury K E, Murphy N, Key T J. (2019) Diet and colorectal cancer in UK Biobank: a prospective study. 17. pii: dyz064. doi: 10.1093/ije/dyz064. [Epub ahead of print] PubMed PMID: , Int 30993317.
- 445.Fedirko V, Tramacere I, Bagnardi V, Rota M, Scotti L et al. (2011) Alcohol drinking and colorectal cancer risk: an overall and dose-response meta-analysis of published studies. Ann Oncol. Sep;22(9): 1958-72. doi: 10.1093/annonc/mdq653. Epub 2011 Feb 9. Review. PubMed PMID: 21307158.
- 446.Vieira A R, Abar L, DSM Chan, Vingeliene S, Polemiti E et al. (2017) Foods and beverages and colorectal cancer risk: a systematic review and meta-analysis of cohort studies, an update of the evidence of the WCRF-AICR Continuous Update Project. Ann Oncol. doi: 10.1093/annonc/mdx171. Review. PubMed PMID: 28(8), 1788-1802.
- 447.Pericleous M, Mandair D, Caplin M E.Diet and supplements and their impact on colorectal cancer. Review. PubMed PMID: 24294513; PubMed Central PMCID: PMC3819783 , J Gastrointest Oncol 4(4), 409-23.
- 448.Chen Z, Wang P P, Woodrow J, Zhu Y, Roebothan B et al. (2015) Dietary patterns and colorectal cancer: results from a Canadian population-based study. PubMed PMID: 25592002; PubMed Central PMCID: PMC4326290 , Nutr 14(8), 1-9.
- 449.National Cancer Institute. Financial Burden of Cancer Care Available From:https://progressreport.cancer.gov/after/economic_burden (2019) .
- 450. (2019) American Cancer Society. Colorectal Cancer Facts & Figures. Available from:https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/colorectal-cancer-facts-and-figures/colorectal-cancer-facts-and-figures-2019.pdf.
- 451.Gellad Z F, Provenzale D.Colorectal cancer: national and international perspective on the burden of disease and public health impact. Gastroenterology. 2010 Jun;138(6): 2177-90. doi: 10.1053/j.gastro.2010.01.056. Review. PubMed PMID: 20420954.
- 452.Cancer World.Research Fund International. Colorectal cancer statistics. Available from:https://www.wcrf.org/dietandcancer/cancer-trends/colorectal-cancer-statistics.
- 453. (2003) . Rodriguez-Bigas MA, Lin EH, Crane CH. Stage IV Colorectal Cancer. In: Kufe DW, Pollock RE, Weichselbaum RR, et al., editors. Holland-Frei Cancer Medicine. 6th edition. Hamilton (ON): BC Decker; Available from: https://www.ncbi.nlm.nih.gov/books/NBK13267/
- 454.Lee S D, Choe J W, Lee B J, Kang M H, Joo M K et al. (2015) Butein effects in colitis and interleukin-6/signal transducer and activator of transcription 3 expression. 10.3748/wjg.v21.i2.465. PubMed PMID: 25593461; PubMed Central PMCID: PMC4292277 21(2), 465-74.
- 455.Yang Y, Zhang J, Weiss N S, Guo L, Zhang L et al. (2019) The consumption of chili peppers and the risk of colorectal cancer: a matched case-control study. World J Surg Oncol. PubMed PMID: 30995922; PubMed Central PMCID: PMC6472026 17(71), 1-7.
- 456.Bar-Shalom R, Bergman M, Grossman S, Azzam N, Sharvit L et al. (2019) Inula Viscosa Extract Inhibits Growth of Colorectal Cancer Cells in vitro and in vivo Through Induction of Apoptosis. Front Oncol. 10;9: 227. doi: 10.3389/fonc.2019.00227. eCollection 2019. PubMed PMID: 31024836; PubMed Central PMCID: PMC6469364 .
- 457.Tong J, Shen Y, Zhang Z, Hu Y, Zhang X et al. (2019) Apigenin inhibits epithelial-mesenchymal transition of human colon cancer cells through NF-κB/Snail signaling pathway. Biosci Rep. pii: BSR20190452. doi: 10.1042/BSR20190452. Print 39(5), 6522743.
- 458.Aggarwal B, Prasad S, Sung B, Krishnan S, Guha S. (2013) Prevention and Treatment of Colorectal Cancer by Natural Agents From Mother Nature. Curr Colorectal Cancer Rep. PubMed PMID: 23814530; PubMed Central PMCID: PMC3693477 9(1), 37-56.
- 459.Kumar S, Agnihotri N Piperlongumine. (2019) a piper alkaloid targets Ras/PI3K/Akt/mTOR signaling axis to inhibit tumor cell growth and proliferation in DMH/DSS induced experimental colon cancer. Biomed Pharmacother. Jan;109: 1462-1477. doi: 10.1016/j.biopha.2018.10.182. Epub 2018 Nov 13. PubMed PMID: 30551398.
- 460.Xu J, Long Y, Ni L, Yuan X, Yu N et al. (2019) Anticancer effect of berberine based on experimental animal models of various cancers: a systematic review and meta-analysis. BMC Cancer. PubMed PMID: 31208348; PubMed Central PMCID: PMC6580644 19(589), 1-20.
- 461.Dai W, Mu L, Cui Y, Li Y, Chen P et al.Berberine Promotes Apoptosis of Colorectal Cancer via Regulation of the Long Non-Coding RNA (lncRNA). Cancer Susceptibility Candidate 2 (CASC2)/AU-Binding Factor 1 (AUF1)/B-Cell CLL/Lymphoma 2 (Bcl-2) Axis. Med Sci Monit. 2019 Jan 25;25: 730-738. doi: 10.12659/MSM.912082. PubMed PMID: 30681073; PubMed Central PMCID: PMC6357823 .
- 462.González-Sarrías A, MÁ Núñez-Sánchez, Tomé-Carneiro J, Tomás-Barberán F A, García-Conesa M T et al. (2016) Comprehensive characterization of the effects of ellagic acid and urolithins on colorectal cancer and key-associated molecular hallmarks: MicroRNA cell specific induction of CDKN1A (p21) as a common mechanism involved. Mol Nutr Food Res. Apr;60(4): 701-16. doi: 10.1002/mnfr.201500780. Epub 2015 Dec 29. PubMed PMID: 26634414.
- 463.Nuñez-Sánchez M A, Dávalos A, González-Sarrías A, Casas-Agustench P, Visioli F et al. (2015) MicroRNAs expression in normal and malignant colon tissues as biomarkers of colorectal cancer and in response to pomegranate extracts consumption: Critical issues to discern between modulatory effects and potential artefacts. Mol Nutr Food Res. Oct;59(10): 1973-86. doi: 10.1002/mnfr.201500357. Epub 2015 Jul 20. PubMed PMID: 26105520.
- 464.Nuñez-Sánchez M A, González-Sarrías A, García-Villalba R, Monedero-Saiz T, García-Talavera N V et al. (2017) Gene expression changes in colon tissues from colorectal cancer patients following the intake of an ellagitannin-containing pomegranate extract: a randomized clinical trial. J Nutr Biochem. Apr;42: 126-133. doi: 10.1016/j.jnutbio.2017.01.014. Epub PubMed PMID: 28183047.
- 465.Navy. (2018) Beans Impact the Stool Metabolome and Metabolic Pathways for Colon Health in Cancer Survivors. pii: E28. doi: 10.3390/nu11010028. PubMed PMID: 30583518; PubMed Central PMCID: PMC6356708 , Nutrients 11(1).
- 466.Bogachek M V, Park J M, De Andrade JP, Lorenzen A W, Kulak M V et al.. Inhibiting the SUMO Pathway Represses the Cancer Stem Cell Population in Breast and Colorectal Carcinomas. Stem Cell Reports. 2016 Dec 13;7(6): 1140-1151. doi: 10.1016/j.stemcr.2016.11.001. Epub 2016 Dec 1. PubMed PMID: 27916539; PubMed Central PMCID: PMC5161532 .
- 467.Gong X, Chen Z, Han Q, Chen C, Jing L et al. (2018) Sanguinarine triggers intrinsic apoptosis to suppress colorectal cancer growth through disassociation between STRAP. PubMed PMID: 29783958; PubMed Central PMCID: PMC5963096 18(578), 1-15.
- 468.Zeng A, Hua H, Liu L, Zhao J. (2019) Corrigendum to 'Betulinic acid induces apoptosis and inhibits metastasis of human colorectal cancer cells in vitro and in vivo'. Bioorg Med Chem. 2019 Aug 12: 115024. doi: 10.1016/j.bmc.2019.07.040. [Epub ahead of print] PubMed PMID: , Bioorg. Med. Chem 27, 2546-2552.
- 469.Dutta D, Paul B, Mukherjee B, Mondal L, Sen S et al. (2019) Nanoencapsulated betulinic acid analogue distinctively improves colorectal carcinoma in vitro and in vivo. Sci Rep. PubMed PMID: 31395908; PubMed Central PMCID: PMC6687831 9(11506), 1-20.
- 470.Toden S, Okugawa Y, Buhrmann C, Nattamai D, Anguiano E et al. (2015) Novel Evidence for Curcumin and Boswellic Acid-Induced Chemoprevention through Regulation of miR-34a and miR-27a in Colorectal Cancer. Cancer Prev Res (Phila). 8(5), 431-43.
- 471.Leu J D, Wang B S, Chiu S J, Chang C Y, Chen C C et al. (2016) Combining fisetin and ionizing radiation suppresses the growth of mammalian colorectal cancers in xenograft tumor models. Oncol Lett. Dec;12(6): 4975-4982. doi: 10.3892/ol.2016.5345. Epub 2016 Nov 2. PubMed PMID: 28105204; PubMed Central PMCID: PMC5228362 .
- 472.Huang Y T, Lin C I, Chien P H, Tang T T, Lin J et al. (2014) The depletion of securin enhances butein-induced apoptosis and tumor inhibition in human colorectal cancer. Chem Biol Interact. 5;220: 41-50. doi: 10.1016/j.cbi.2014.06.006. Epub 2014 Jun 12. PubMed PMID: 24931875.
- 473.Yit C C, Das N P. (1994) Cytotoxic effect of butein on human colon adenocarcinoma cell proliferation. Cancer Lett. PubMed PMID: 82(1), 65-72.
- 474.Zhang L, Yang X, Li X, Li C, Zhao L et al. (2015) Butein sensitizes HeLa cells to cisplatin through the AKT and ERK/p38 MAPK pathways by targeting. FoxO3a. Int J Mol Med. 2015 Oct;36(4): 957-66. doi: 10.3892/ijmm.2015.2324. Epub 4564095.
- 475.Jin J, Lin G, Huang H, Xu D, Yu H et al. (2014) Capsaicin mediates cell cycle arrest and apoptosis in human colon cancer cells via stabilizing and activating p53. , Int J Biol Sci 10(3), 285-95.
- 476.Lee S H, Clark R.Anti-Tumorigenic Effects of Capsaicin in Colon Cancer. , J Food Chem Nanotechnol 2016, 162-167.
- 477.Yang J, Li T Z, Xu G H, Luo B B, Chen Y X et al.Low-concentration capsaicin promotes colorectal cancer metastasis by triggering ROS production and modulating Akt/mTOR and STAT-3 pathways. PubMed PMID: , Neoplasma 60(4), 364-72.
- 478.Ozmen N, Kaya-Sezginer E, Bakar-Ates F.The Cellular Uptake and Apoptotic Efficiency of Colchicine is. Correlated with Downregulation of MMP-9 mRNA Expression in SW480 Colon Cancer Cells. Anticancer Agents Med Chem 18(13), 1927-1933.
- 479.Huang Z, Xu Y, Peng W. (2015) Colchicine induces apoptosis in HT29 human colon cancer cells via the AKT and c-Jun N-terminal kinase signaling pathways. Mol Med Rep. Oct;12(4): 5939-44. doi: 10.3892/mmr.2015.4222. Epub 2015 Aug 12. PubMed PMID: 26299305.
- 480.Zhang T, Chen W, Jiang X, Liu L, Wei K et al. (2019) Anticancer effects and underlying mechanism of Colchicine on human gastric cancer cell lines in vitro and in vivo. Biosci Rep. 15;39(1). pii: BSR20181802. doi: 10.1042/BSR20181802. Print 6331673.
- 481.Saud S M, Li W, Morris N L, Matter M S, Colburn N H et al. (2014) Resveratrol prevents tumorigenesis in mouse model of Kras activated sporadic colorectal cancer by suppressing oncogenic Kras expression. Carcinogenesis. Dec;35(12): 2778-86. doi: 10.1093/carcin/bgu209. Epub 2014 Oct 3. PubMed PMID: 25280562; PubMed Central PMCID: PMC4247523 .
- 482.Altamemi I, Murphy E A, Catroppo J F, Zumbrun E E, Zhang J et al. (2014) Role of microRNAs in resveratrol-mediated mitigation of colitis-associated tumorigenesis. in Apc(Min/+) mice. J Pharmacol Exp Ther. 2014 Jul;350(1): 99-109. doi: 10.1124/jpet.114.213306. Epub 4056272.
- 483.Chung S S, Wu Y, Okobi Q, Adekoya D, Atefi M et al.. Proinflammatory Cytokines IL-6 and TNF-α Increased Telomerase Activity through NF-κB/STAT1/STAT3 Activation, and Withaferin A Inhibited the Signaling in Colorectal Cancer Cells. Mediators Inflamm. 2017;2017: 5958429. doi: 10.1155/2017/5958429. Epub 2017 Jun 6. PubMed PMID: 28676732; PubMed Central PMCID: PMC5476880 .
- 484.Reddivari L, Charepalli V, Radhakrishnan S, Vadde R, Elias R J et al. (2016) Grape compounds suppress colon cancer stem cells in vitro and in a rodent model of colon carcinogenesis. PubMed PMID: 27506388; PubMed Central PMCID: PMC4977641 , BMC Complement Altern Med 16(278), 1-12.
- 485.Kumazaki M, Noguchi S, Yasui Y, Iwasaki J, Shinohara H et al. (2013) Anti-cancer effects of naturally occurring compounds through modulation of signal transduction and miRNA expression in human colon cancer cells. J Nutr Biochem. Nov;24(11): 1849-58. doi: 10.1016/j.jnutbio.2013.04.006. Epub 2013 Aug 16. PubMed PMID: 23954321.
- 486.Raja S B, Rajendiran V, Kasinathan N K, A P, Venkatabalasubramanian S et al. (2017) Differential cytotoxic activity of Quercetin on colonic cancer cells depends on ROS generation through COX-2 expression. Food Chem Toxicol. Aug;106(Pt A): 92-106. doi: 10.1016/j.fct.2017.05.006. Epub 2017 May 4. PubMed PMID: 28479391.
- 487.Yang L, Liu Y, Wang M, Qian Y, Dong X et al. (2016) Quercetin-induced apoptosis of HT-29 colon cancer cells via inhibition of the Akt-CSN6-Myc signaling axis. Mol Med Rep. Nov;14(5): 4559-4566. doi: 10.3892/mmr.2016.5818. Epub 2016 Oct 10. PubMed PMID: 27748879; PubMed Central PMCID: PMC5101998 .
- 488.Kim H J, Kim S K, Kim B S, Lee S H, Park Y S et al. (2010) Apoptotic effect of quercetin on HT-29 colon cancer cells via the AMPK signaling pathway. J Agric Food Chem. PubMed PMID: 58(15), 8643-50.
- 489.Refolo M G, D'Alessandro R, Malerba N, Laezza C, Bifulco M et al. (2015) Anti Proliferative and Pro Apoptotic Effects of Flavonoid Quercetin Are Mediated by CB1 Receptor in Human Colon Cancer Cell Lines. J Cell Physiol. Dec;230(12): 2973-80. doi: 10.1002/jcp.25026. PubMed PMID: 25893829.
- 490.Zhang X A, Zhang S, Yin Q, Zhang J. (2015) Quercetin induces human colon cancer cells apoptosis by inhibiting the nuclear factor-kappa B Pathway. Pharmacogn Mag. PubMed PMID: 25829782; PubMed Central PMCID: PMC4378141 11(42), 404-9.
- 491.James S, Aparna J S, Paul A M, Lankadasari M B, Mohammed S et al. (2017) Cardamonin inhibits colonic neoplasia through modulation of MicroRNA expression. Sci Rep. PubMed PMID: 29066742; PubMed Central PMCID: PMC5655681 7(1), 13945-10.
- 492.Park S, Gwak J, Han S J, Oh S.Cardamonin suppresses the proliferation of colon cancer cells by promoting β-catenin degradation. Epub 2013 Mar 29. PubMed PMID: , Biol Pharm Bull 36(6), 1040-4.
- 493.Lu S, Lin C, Cheng X, Hua H, Xiang T et al. (2018) Cardamonin reduces chemotherapy resistance of colon cancer cells via the TSP50/NF-κB pathway in vitro. Oncol Lett. Jun;15(6): 9641-9646. doi: 10.3892/ol.2018.8580. Epub 2018 Apr 26. PubMed PMID: 29928339; PubMed Central PMCID: PMC6004643 .
- 494.Jiang Z, Cao Q, Dai G, Wang J, Liu C et al. (2019) Celastrol inhibits colorectal cancer through TGF-β1/Smad signaling. Onco Targets Ther. 9;12: 509-518. doi: 10.2147/OTT.S187817. eCollection 2019. PubMed PMID: 30666129; PubMed Central PMCID: PMC6331187 .
- 495.Gao Y, Zhou S, Pang L, Yang J, Li H J et al. (2019) Celastrol suppresses nitric oxide synthases and the angiogenesis pathway in colorectal cancer. Free Radic Res. Epub 2019 Feb 18. PubMed PMID: 53(3), 324-334.
- 496.Moreira H, Szyjka A, Gąsiorowski K. (2018) Chemopreventive activity of celastrol in drug-resistant human colon carcinoma cell cultures. Oncotarget. 9(30), 21211-21223.
- 497.Bufu T, X Yilin Z Di, Gege L, Xi C, Ling W. (2018) Celastrol inhibits colorectal cancer cell proliferation and migration through suppression of MMP3 and MMP7 by the PI3K/AKT signaling pathway. Anticancer Drugs. Jul;29(6): 530-538. doi: 10.1097/CAD.0000000000000621. PubMed PMID: 29553945.
- 498.Xiao-Pei H, Ji-Kuai C, Xue W, Dong Y F, Yan L et al. (2018) Systematic identification of Celastrol-binding proteins reveals that Shoc2 is inhibited by Celastrol. Biosci Rep. 20; 38(6). pii: BSR20181233. doi: 10.1042/BSR20181233. Print 2018 Dec 21. PubMed PMID: 30333251; PubMed Central PMCID: PMC6246769 .
- 499.Chen L, Jiang K, Chen H, Tang Y, Zhou X et al. (2018) Deguelin induces apoptosis in colorectal cancer cells by activating the p38 MAPK pathway. , Cancer Manag Res.; 11, 95-105.
- 500.Murillo G, Salti G I, Kosmeder JW 2nd, Pezzuto J M, Mehta R G. (2002) Deguelin inhibits the growth of colon cancer cells through the induction of apoptosis and cell cycle arrest. Dec;38(18): 2446-54. PubMed PMID: , Eur 12460790.
- 501.Lokhande K B, Nagar S, Swamy K V. (2019) Molecular interaction studies of Deguelin and its derivatives with Cyclin D1 and Cyclin E in cancer cell signaling pathway: The computational approach. Sci Rep. PubMed PMID: 30741976; PubMed Central PMCID: PMC6370771 9(1), 1-13.
- 502.Kang W, Zheng X, Wang P, Guo S. (2018) Deguelin exerts anticancer activity of human gastric cancer MGC-803 and MKN-45 cells in vitro. Jun;41(6): 3157-3166. doi: 10.3892/ijmm.2018.3532. Epub 2018 Mar 5. PubMed PMID: 29512685; PubMed Central PMCID: PMC5881843 , Int J Mol Med.
- 503.Diosgenin. (2007) a naturally occurring steroid [corrected] saponin suppresses 3-hydroxy-3-methylglutaryl CoA reductase expression and induces apoptosis in HCT-116 human colon carcinoma cells. Cancer Lett. PubMed PMID: 255(2), 194-204.
- 504.Lepage C, Léger D Y, Bertrand J, Martin F, Beneytout J L et al. (2011) Diosgenin induces death receptor-5 through activation of p38 pathway and promotes TRAIL-induced apoptosis in colon cancer cells. Cancer Lett. 10.1016/j.canlet.2010.12.003. Epub 2010 Dec 30. PubMed PMID: 301(2), 193-202.
- 505.Jesus M, Martins A P, Gallardo E, Silvestre S. (2016) Diosgenin: Recent Highlights on Pharmacology and Analytical Methodology. Epub 2016 Dec 28. Review. PubMed PMID: 28116217; PubMed Central PMCID: PMC5225340 , J Anal Methods Chem; 1-16.
- 506.Sethi G, Shanmugam M K, Warrier S, Merarchi M, Arfuso F et al. (2018) . Pro-Apoptotic and Anti-Cancer Properties of Diosgenin: A Comprehensive and Critical Review. Nutrients; 10(5). pii: E645. doi: 10.3390/nu10050645. Review. PubMed PMID: 29783752; PubMed Central PMCID: PMC5986524 .
- 507.Dai G, Ding K, Cao Q, Xu T, He F et al.Emodin suppresses growth and invasion of colorectal cancer cells by inhibiting VEGFR2. Eur J Pharmacol. 2019 Sep 15;859: 172525. doi: 10.1016/j.ejphar.2019.172525. Epub 2019 Jul 6. PubMed PMID: 31288005.
- 508.Gu J, Cui C F, Yang L, Wang L, Jiang X H. (2019) Emodin Inhibits Colon Cancer Cell Invasion and Migration by Suppressing Epithelial-Mesenchymal Transition via the Wnt/β-Catenin Pathway. Oncol Res. 10.3727/096504018X15150662230295. Epub 2018 Jan 4. PubMed PMID: 27(2), 193-202.
- 509.Saunders I T, Mir H, Kapur N, Singh S. (2019) Emodin inhibits colon cancer by altering BCL-2 family proteins and cell survival pathways. Cancer Cell Int. PubMed PMID: 31011292; PubMed Central PMCID: PMC6466701 1-18.
- 510.Wang Y, Luo Q, He X, Wei H, Wang T et al. (2018) Emodin Induces Apoptosis of Colon Cancer Cells via Induction of Autophagy in a ROS-Dependent Manner. Oncol Res. 10.3727/096504017X15009419625178. Epub 2017 Jul 25. PubMed PMID: 26(6), 889-899.
- 511.Wu T, Wang C, Wang W, Hui Y, Zhang R et al.Embelin impairs the accumulation and activation of MDSCs in colitis-associated tumorigenesis. Oncoimmunology. 2018 Aug 24;7(11):e1498437. doi: 10.1080/2162402X.2018.1498437. eCollection 2018. PubMed PMID: 30377563; PubMed Central PMCID: PMC6205065 .
- 512.Dai Y, Jiao H, Teng G, Wang W, Zhang R et al. (2014) Embelin reduces colitis-associated tumorigenesis through limiting IL-6/STAT3 signaling. Mol Cancer Ther. PubMed PMID: 13(5), 1206-16.
- 513.Wu T, Dai Y, Wang W, Teng G, Jiao H et al.Macrophage targeting contributes to the inhibitory effects of embelin on colitis-associated cancer. Oncotarget. 2016 Apr 12;7(15): 19548-58. doi: 10.18632/oncotarget.6969. PubMed PMID: 26799669; PubMed Central PMCID: PMC4991400 .
- 514.Cheng C, Dong W. (2018) Aloe-Emodin Induces Endoplasmic Reticulum Stress-Dependent Apoptosis in Colorectal Cancer Cells. 10.12659/MSM.908400. PubMed PMID: 30199885; PubMed Central PMCID: PMC6142869 , Med Sci Monit; 24, 6331-6339.
- 515.Bedi D, Henderson H J, Manne U, Samuel T. (2019) Camptothecin Induces PD-L1 and Immunomodulatory Cytokines in Colon Cancer Cells. Medicines. pii: E51. doi: 10.3390/medicines6020051. PubMed PMID: 31022845; PubMed Central PMCID: PMC6631458 , (Basel) 6(2).
- 516.Yang N, Zhao Y, Wang Z, Liu Y, Zhang Y. (2017) Scutellarin suppresses growth and causes apoptosis of human colorectal cancer cells by regulating the p53 pathway. Mol Med Rep. Feb;15(2): 929-935. doi: 10.3892/mmr.2016.6081. Epub 2016 Dec 28. PubMed PMID: 28035355.
- 517.Kang K A, Piao M J, Ryu Y S, Hyun Y J, Park J E et al. (2017) Luteolin induces apoptotic cell death via antioxidant activity in human colon cancer cells. Oct;51(4): 1169-1178. doi: 10.3892/ijo.2017.4091. Epub 2017 Aug 2. PubMed PMID: , Int 28791416.
- 518.A Di Francesco, Falconi A, C Di Germanio, MV Micioni Di Bonaventura, Costa A et al. (2015) Extravirgin olive oil up-regulates CB tumor suppressor gene in human colon cancer cells and in rat colon via epigenetic mechanisms. J Nutr Biochem. Mar;26(3): 250-8. doi: 10.1016/j.jnutbio.2014.10.013. Epub 2014 Dec 3. PubMed PMID: 25533906.
- 519.Huang G M, Sun Y, Ge X, Wan X, Li C B. (2015) Gambogic acid induces apoptosis and inhibits colorectal tumor growth via mitochondrial pathways. 10.3748/wjg.v21.i20.6194. PubMed PMID: 26034354; PubMed Central PMCID: PMC4445096 21(20), 6194-205.
- 520.Tsoukas M A, Ko B J, Witte T R, Dincer F, Hardman W E et al. (2015) Dietary walnut suppression of colorectal cancer in mice: Mediation by miRNA patterns and fatty acid incorporation. J Nutr Biochem. Jul;26(7): 776-83. doi: 10.1016/j.jnutbio.2015.02.009. Epub 2015 Apr 1. PubMed PMID: 25882694.
- 521.Kim J, Lee J, Oh J H, Chang H J, Sohn D K et al. (2019) Associations among dietary seaweed intake, c-MYC rs6983267 polymorphism, and risk of colorectal cancer in a Korean population: a case-control study. [Epub ahead of print] PubMed PMID: , Eur 12, 10-1007.
- 522.Zhao Y, Zheng Y, Wang J, Ma S, Yu Y et al. (2018) Fucoidan Extracted from Undaria pinnatifida: Source for Nutraceuticals/Functional Foods. Mar Drugs. 9;16(9). pii: E321. doi: 10.3390/md16090321. Review. PubMed PMID: 30205616; PubMed Central PMCID: PMC6164441 .
- 523.Tsai H L, Tai C J, Huang C W, Chang F R, Wang J Y. (2017) Efficacy of Low-Molecular-Weight Fucoidan as a Supplemental Therapy in Metastatic Colorectal Cancer Patients: A Double-Blind Randomized Controlled Trial. Mar Drugs. 21;15(4). pii: E122. doi: 10.3390/md15040122. PubMed PMID: 28430159; PubMed Central PMCID: PMC5408268 .
- 524.Wang S K, Li Y, White W L, Lu J. (2014) Extracts from New Zealand Undaria pinnatifida Containing Fucoxanthin as Potential Functional Biomaterials against Cancer in Vitro. J Funct Biomater. 10.3390/jfb5020029. PubMed PMID: 24956438; PubMed Central PMCID: PMC4099972 5(2), 29-42.
- 525.Han Y S, Lee J H, Lee S H. (2015) Fucoidan inhibits the migration and proliferation of HT-29 human colon cancer cells via the phosphoinositide-3 kinase/Akt/mechanistic target of rapamycin pathways. Mol Med Rep. Sep;12(3): 3446-3452. doi: 10.3892/mmr.2015.3804. Epub 4526071.
- 526.Han Y S, Lee J H, Lee S H. (2015) Antitumor Effects of Fucoidan on Human Colon Cancer Cells via Activation of Akt Signaling. Biomol Ther (Seoul). May;23(3): 225-32. doi: 10.4062/biomolther.2014.136. Epub 4428714.
- 527.Chen L M, Liu P Y, Chen Y A, Tseng H Y, Shen P C et al. (2017) Oligo-Fucoidan prevents IL-6 and CCL2 production and cooperates with p53 to suppress ATM signaling and tumor progression. Sci Rep. PubMed PMID: 28928376; PubMed Central PMCID: PMC5605496 7(11864), 1-12.
- 528.Kim S-K, Karagozlu M Z. (2011) Chapter 17. Marine algae: Natural Product Source for the gastrointestinal Cancer Treatment. In: Marine Medicinal Foods: Implications and Applications. Macro and Microalgae, Volume 64 of Advances in Food and Nutrition Research, ISSN 1043-4526. Editors: Se-Kwon Kim, Steve , ISBN 0123876699, 9780123876690.
- 529.Bakunina I, Chadova O, Malyarenko O, Ermakova S. (2018) The Effect of Fucoidan from the Brown Alga Fucus evanescence on the Activity of α-N-Acetylgalactosaminidase of Human Colon Carcinoma Cells. Mar Drugs. 10;16(5). pii: E155. doi: 10.3390/md16050155. PubMed PMID: 29748462; PubMed Central PMCID: PMC5983286 .
- 530.Kim I H, Kwon M J, Nam T J. (2017) Differences in cell death and cell cycle following fucoidan treatment in high-density HT-29 colon cancer cells. Mol Med Rep. Jun;15(6): 4116-4122. doi: 10.3892/mmr.2017.6520. Epub 5436236.
- 531.Tsai C F, Yeh W L, Chen J H, Lin C, Huang S S et al.Osthole suppresses the migratory ability of human glioblastoma multiforme cells via inhibition of focal adhesion kinase-mediated matrix metalloproteinase-13 expression. Int J Mol Sci. 2014 Mar 4;15(3): 3889-903. doi: 10.3390/ijms15033889. PubMed PMID: 24599080; PubMed Central PMCID: PMC3975374 .
- 532.Kim H Y, Kim Y M, Hong S. (2019) Astaxanthin suppresses the metastasis of colon cancer by inhibiting the MYC-mediated downregulation of microRNA-29a-3p and microRNA-200a. Sci Rep. PubMed PMID: 31263239; PubMed Central PMCID: PMC6603017 9(9457), 1-10.
- 533.Nagendraprabhu P, Sudhandiran G. (2011) Astaxanthin inhibits tumor invasion by decreasing extracellular matrix production and induces apoptosis in experimental rat colon carcinogenesis by modulating the expressions of ERK-2, NFkB and COX-2. Invest New Drugs. 29(2), 207-24.
- 534.Hormozi M, Ghoreishi S, Baharvand P. (2019) Astaxanthin induces apoptosis and increases activity of antioxidant enzymes in LS-180 cells. Artif Cells Nanomed Biotechnol. Dec;47(1): 891-895. doi: 10.1080/21691401.2019.1580286. PubMed PMID: 30873887.
- 535.Yasui Y, Hosokawa M, Mikami N, Miyashita K, Tanaka T. (2011) Dietary astaxanthin inhibits colitis and colitis-associated colon carcinogenesis in mice via modulation of the inflammatory cytokines. Chem Biol Interact. PubMed PMID: 193(1), 79-87.
- 536.Liu X, Song M, Gao Z, Cai X, Dixon W et al. (2016) Stereoisomers of Astaxanthin Inhibit Human Colon Cancer Cell Growth by Inducing G2/M Cell Cycle Arrest and Apoptosis. J Agric Food Chem. 10.1021/acs.jafc.6b03636. Epub 2016 Oct 11. PubMed PMID: 64(41), 7750-7759.
- 537.Wayakanon K, Rueangyotchanthana K, Wayakanon P, Suwannachart C. (2018) The inhibition of Caco-2 proliferation by astaxanthin from Xanthophyllomyces dendrorhous. Apr;67(4): 507-513. doi: 10.1099/jmm.0.000710. Epub 2018 Mar 5. PubMed PMID: , J Med Microbiol 29504932.
- 538.Tanaka T, Kawamori T, Ohnishi M, Makita H, Mori H et al. (1995) Suppression of azoxymethane-induced rat colon carcinogenesis by dietary administration of naturally occurring xanthophylls astaxanthin and canthaxanthin during the postinitiation phase. Carcinogenesis. Dec;16(12): 2957-63. PubMed PMID: 8603470.
- 539.Terasaki M, Iida T, Kikuchi F, Tamura K, Endo T et al. (2019) Fucoxanthin potentiates anoikis in colon mucosa and prevents carcinogenesis in AOM/DSS model mice. J Nutr Biochem. Feb;64: 198-205. doi: 10.1016/j.jnutbio.2018.10.007. Epub 2018 Oct 25. PubMed PMID: 30530259.
- 540.Terasaki M, Masaka S, Fukada C, Houzaki M, Endo T et al.Salivary Glycine Is a Significant Predictor for the Attenuation of Polyp and Tumor Microenvironment Formation by Fucoxanthin in AOM/DSS Mice. In Vivo. 2019 Mar-Apr;33(2): 365-374. doi: 10.21873/invivo.11483. PubMed PMID: 30804114; PubMed Central PMCID: PMC6506301 .
- 541.Terasaki M, Matsumoto N, Hashimoto R, Endo T, Maeda H et al. (2018) Fucoxanthin administration delays occurrence of tumors in xenograft mice by colonospheres, with an anti-tumor predictor of glycine. , J Clin Biochem Nutr 64(1), 52-58.
- 542.Das S K, Hashimoto T, Shimizu K, Yoshida T, Sakai T et al. (2005) Fucoxanthin induces cell cycle arrest at G0/G1 phase in human colon carcinoma cells through up-regulation of p21WAF1/Cip1. Biochim Biophys Acta. Epub 2005 Oct 3. PubMed PMID: 1726(3), 328-35.
- 543.Hosokawa M, Kudo M, Maeda H, Kohno H, Tanaka T et al. (2004) Fucoxanthin induces apoptosis and enhances the antiproliferative effect of the PPARgamma ligand, troglitazone, on colon cancer cells. Biochim Biophys Acta. PubMed PMID: 1675(1), 113-9.
- 544.Kim J M, Araki S, Kim D J, Park C B, Takasuka N et al. (1998) Chemopreventive effects of carotenoids and curcumins on mouse colon carcinogenesis after 1,2-dimethylhydrazine initiation. Carcinogenesis. Jan;19(1): 81-5. PubMed PMID: 9472697
- 545.Konishi I, Hosokawa M, Sashima T, Kobayashi H, Miyashita K. (2006) Halocynthiaxanthin and fucoxanthinol isolated from Halocynthia roretzi induce apoptosis in human leukemia, breast and colon cancer cells. Comp Biochem Physiol C Toxicol Pharmacol. Jan-Feb;142(1-2): 53-9. Epub 2005 Dec 7. PubMed PMID: 16337836.
- 546.Kim J, Lee J, Oh J H, Chang H J, Sohn D K et al.. Dietary Lutein Plus Zeaxanthin Intake and DICER1 rs3742330 A Polymorphism Relative to Colorectal Cancer Risk. Sci Rep. 2019 Mar 4;9(1): 3406. doi: 10.1038/s41598-019-39747-5. PubMed PMID: 30833603; PubMed Central PMCID: PMC6399314 .
- 547.Reynoso-Camacho R, González-Jasso E, Ferriz-Martínez R, Villalón-Corona B, Loarca-Piña G F et al.Dietary supplementation of lutein reduces colon carcinogenesis in DMH-treated rats by modulating K-ras, PKB, and β-catenin proteins. PubMed PMID: , Nutr Cancer 63(1), 39-45.
- 548.Grudzinski W, Piet M, Luchowski R, Reszczynska E, Welc R et al. (2018) Different molecular organization of two carotenoids, lutein and zeaxanthin, in human colon epithelial cells and colon adenocarcinoma cells. Spectrochim Acta A Mol Biomol Spectrosc. 5;188: 57-63. doi: 10.1016/j.saa.2017.06.041. Epub 2017 Jul 5. PubMed PMID: 28689079.
- 549.Kohler L N, Harris R B, Oren E, Roe D J, Lance P et al.. Adherence to Nutrition and Physical Activity Cancer Prevention Guidelines and Development of Colorectal Adenoma. Nutrients. 2018 Aug 16;10(8). pii: E1098. doi: 10.3390/nu10081098. PubMed PMID: 30115827; PubMed Central PMCID: PMC6115749 .
- 550.Wang Z J, Ohnaka K, Morita M, Toyomura K, Kono S et al. (2013) Dietary polyphenols and colorectal cancer risk: the Fukuoka colorectal cancer study. 10.3748/wjg.v19.i17.2683. PubMed PMID: 23674876; PubMed Central PMCID: PMC3645387 19(17), 2683-90.
- 551.Alam M N, Almoyad M, Huq F. (2018) Polyphenols in Colorectal Cancer: Current State of Knowledge including Clinical Trials and Molecular Mechanism of Action. Biomed Res Int. 5820674.
- 552.Murphy N, Achaintre D, Zamora-Ros R, Jenab M, Boutron-Ruault M C et al. (2018) A prospective evaluation of plasma polyphenol levels and colon cancer risk. Int J Cancer. doi: 10.1002/ijc.31563. [Epub ahead of print] PubMed PMID: 29696648; PubMed Central PMCID:. 6175205.
- 553.Mileo A M, Nisticò P, Miccadei S. (2019) Polyphenols: Immunomodulatory and Therapeutic Implication in Colorectal Cancer. Front Immunol. 11;10: 729. doi: 10.3389/fimmu.2019.00729. eCollection 2019. Review. PubMed PMID: 31031748; PubMed Central PMCID: PMC6470258 .
- 554.Zamora-Ros R, Cayssials V, Jenab M, Rothwell J A, Fedirko V et al. (2018) Dietary intake of total polyphenol and polyphenol classes and the risk of colorectal cancer in the European Prospective Investigation into Cancer and Nutrition (EPIC) cohort. Eur. 33(11), 1063-1075.
- 555.Ishida Y, Gao R, Shah N, Bhargava P, Furune T et al. (2018) Anticancer Activity in Honeybee Propolis: Functional Insights to the Role of Caffeic Acid Phenethyl Ester and Its Complex With γ-Cyclodextrin. Integr Cancer Ther. Sep;17(3): 867-873. doi: 10.1177/1534735417753545. Epub 2018 Feb 2. PubMed PMID: 29390900; PubMed Central PMCID: PMC6142091 .
- 556.Stähli A, Maheen C U, Strauss F J, Eick S, Sculean A et al. (2019) Caffeic acid phenethyl ester protects against oxidative stress and dampens inflammation via heme oxygenase 1. Int J Oral Sci. PubMed PMID: 30783082; PubMed Central PMCID: PMC6381107 11(6), 1-8.
- 557.Murtaza G, Karim S, Akram M R, Khan S A, Azhar S et al. (2014) Caffeic acid phenethyl ester and therapeutic potentials. Biomed Res Int. Epub 1-9.
- 558.Robertson J, Raizer J, Hodges J S, Gradishar W, Allen J A. (2018) Risk factors for the development of paclitaxel-induced neuropathy in breast cancer patients. J Peripher Nerv Syst. 2018 Jun;23(2): 129-133. doi: 10.1111/jns.12271. Epub 29696771.
- 559.Zang X, Lee J B, Deshpande K, Garbuzenko O B, Minko T et al. (2019) Prevention of paclitaxel-induced neuropathy by formulation approach. J Control Release. 10.1016/j.jconrel.2019.04.013. Epub 2019 Apr 11. PubMed PMID: 30981814; PubMed Central PMCID: PMC6708409 10, 109-116.
- 560.Vahdat L, Papadopoulos K, Lange D, Leuin S, Kaufman E et al. (2001) Reduction of paclitaxel-induced peripheral neuropathy with glutamine. Clin Cancer Res. May;7(5): 1192-7. PubMed PMID: 11350883.
- 561.Kaur S, Muthuraman A. (2019) Ameliorative effect of gallic acid in paclitaxel-induced neuropathic pain in mice. 10.1016/j.toxrep.2019.06.001. eCollection 2019. PubMed PMID: 31211096; PubMed Central PMCID: PMC6562321 , Toxicol Rep; 6, 505-513.
- 562.Chou C K, Huang H W, Yang C F, Dahms H U, Liang S S et al. (2019) Reduced camptothecin sensitivity of estrogen receptor-positive human breast cancer cells following exposure to di(2-ethylhexyl)phthalate (DEHP) is associated with DNA methylation changes. Environ Toxicol. Apr;34(4): 401-414. doi: 10.1002/tox.22694. Epub 2019 Feb 5. PubMed PMID: 30720231.
- 563.Xu H, Krystal G W. (2010) Actinomycin D decreases Mcl-1 expression and acts synergistically with ABT-737 against small cell lung cancer cell lines. Clin Cancer Res. 16(17), 4392-400.
- 564.Merkel O, Wacht N, Sifft E, Melchardt T, Hamacher F et al.. Actinomycin D induces p53-independent cell death and prolongs survival in high-risk chronic lymphocytic leukemia. Leukemia. 2012 Dec;26(12): 2508-16. doi: 10.1038/leu.2012.147. Epub 2012 Jun 1. PubMed PMID: 22743622.
- 565.Ishii M, Iwai M, Harada Y, Kishida T, Asada H et al. (2007) Soluble TRAIL gene and actinomycin D synergistically suppressed multiple metastasis of TRAIL-resistant colon cancer in the liver. Cancer Lett. 245(12), 134-43.
- 566.Pinto A, Pocard M. (2019) Hyperthermic intraperitoneal chemotherapy with cisplatin and mitomycin C for colorectal cancer peritoneal metastases: A systematic review of the literature. Pleura Peritoneum. 4(2), 1-11.
- 567.Symer M M, Yeo H L.Recent advances in the management of anal cancer. F1000Res. 2018 Sep 28;7. pii: F1000 Faculty Rev-1572. doi: 10.12688/f1000research.14518.1. eCollection 2018. Review. PubMed PMID: 30345012; PubMed Central PMCID: PMC6173125 .
- 568.Tan L T, Chan K G, Pusparajah P, Yin W F, Khan T M et al. (2019) Mangrove derived Streptomyces sp. MUM265 as a potential source of antioxidant and anticolon-cancer agents. BMC Microbiol. PubMed PMID: 30760201; PubMed Central PMCID: PMC6375222 1, 10-1186.
- 569.Sakamoto K, Ito S, Hashimoto N, Hasegawa Y. (2017) Pirfenidone as salvage treatment for refractory bleomycin-induced lung injury: a case report of seminoma. BMC Cancer. PubMed PMID: 28784103; PubMed Central PMCID: PMC5547483 17(526), 1-4.
- 570.Yu H, Zhang Z, Huang H, Wang Y, Lin B et al. (2019) Inhibition of bleomycin-induced pulmonary fibrosis in mice by the novel peptide EZY-1 purified from Eucheuma. Food Funct. PubMed PMID: 10(6), 3198-3208.
- 571.Lan C, Wolf S L, Tsang W W. (2013) Tai chi exercise in medicine and health promotion. Evid Based Complement Alternat Med. Epub 2013 Nov 11. PubMed PMID: 24319474; PubMed Central PMCID: PMC3844234 1-3.
- 572.Streckmann F, Balke M, Lehmann H C, Rustler V, Koliamitra C et al. (2018) The preventive effect of sensorimotor- and vibration exercises on the onset of Oxaliplatin- or vinca-alkaloid induced peripheral neuropathies - STOP. BMC Cancer. PubMed PMID: 29316888; PubMed Central PMCID: PMC5761113 18(62), 1-10.
- 573.Elkins G, White J, Patel P, Marcus J, Perfect M M et al. (2006) Hypnosis to manage anxiety and pain associated with colonoscopy for colorectal cancer screening: Case studies and possible benefits. Int J Clin Exp Hypn. Oct;54(4): 416-31. PubMed PMID: 16950684.
- 574.Cossu G, Saba L, Minerba L, Mascalchi M. (2018) Colorectal Cancer Screening: The Role of Psychological, Social and Background Factors in Decision-making Process. Review. PubMed PMID: 29643929; PubMed Central PMCID: PMC5872199 , Clin Pract Epidemiol Ment Health; 14, 63-69.
- 575.Montgomery G H, Schnur J B, Kravits K. (2013) Hypnosis for cancer care: over 200 years young. Jan;63(1): 31-44. doi: 10.3322/caac.21165. Epub 2012 Nov 20. Review. PubMed PMID: 23168491; PubMed Central PMCID: PMC3755455 , CA Cancer.
- 576.Miller S J, Schnur J B, Montgomery G H, Jandorf L.AFRICAN-AMERICANS' AND LATINOS'. PERCEPTIONS OF USING HYPNOSIS TO ALLEVIATE DISTRESS BEFORE A COLONOSCOPY. Contemp Hypn Integr Ther. 2011 Sep;28(3): 196-203. PubMed PMID: 26566440; PubMed Central PMCID: PMC4640674 .
- 577.Umezawa S, Higurashi T, Uchiyama S, Sakai E, Ohkubo H et al. (2015) Visual distraction alone for the improvement of colonoscopy-related pain and satisfaction. 10.3748/wjg.v21.i15.4707. PubMed PMID: 25914482; PubMed Central PMCID: PMC4402320 21(15), 4707-14.
- 578.Lee D W, Chan A C, Wong S K, Fung T M, Li A C et al. (2004) Can visual distraction decrease the dose of patient-controlled sedation required during colonoscopy? A prospective randomized controlled trial. Endoscopy. Mar;36(3): 197-201. PubMed PMID: 14986215.
- 579.Xiaolian J, Xiaolin L, Lan Z H. (2015) Effects of visual and audiovisual distraction on pain and anxiety among patients undergoing colonoscopy. Gastroenterol Nurs. Jan-Feb;38(1): 55-61. doi: 10.1097/SGA.0000000000000089. PubMed PMID: 25636013.
- 580.Leung F W. (2008) Methods of reducing discomfort during colonoscopy. Dig Dis Sci. Jun;53(6): 1462-7. Review. PubMed PMID: 17999189.
- 581.De Silva AP, Niriella M A, Nandamuni Y, Nanayakkara S D, Perera K R et al.Effect of audio and visual distraction on patients undergoing colonoscopy: a randomized controlled study. Endosc Int Open. 2016 Nov;4(11):E1211-E1214. Epub 2016 Oct 20. PubMed PMID: 27853748; PubMed Central PMCID: PMC5110335 .
- 582.Sun H, Huang H, Ji S, Chen X, Xu Y et al. (2019) The Efficacy of Cognitive Behavioral Therapy to Treat Depression and Anxiety and Improve Quality of Life Among Early-Stage Breast Cancer Patients. Integr Cancer Ther. Jan-Dec;18: 1534735419829573. doi: 10.1177/1534735419829573. PubMed PMID: 30791739; PubMed Central PMCID: PMC6432673 .
- 583.Eichler C, Pia M, Sibylle M, Sauerwald A, Friedrich W et al.Cognitive behavioral therapy in breast cancer patients--a feasibility study of an 8 week intervention for tumor associated fatigue treatment. PubMed PMID: , Asian Pac J Cancer Prev 16(3), 1063-7.
- 584.Ye M, Du K, Zhou J, Zhou Q, Shou M et al.A meta-analysis of the efficacy of cognitive behavior therapy on quality of life and psychological health of breast cancer survivors and patients. Psychooncology. 2018 Jul;27(7): 1695-1703. doi: 10.1002/pon.4687. Epub 2018 Mar 26. PubMed PMID: 29500842.
- 585.Kucherer S, Ferguson R J. (2017) Cognitive behavioral therapy for cancer-related cognitive dysfunction. Curr Opin Support Palliat Care. Mar;11(1): 46-51. doi: 10.1097/SPC.0000000000000247. Review. PubMed PMID: 27898511; PubMed Central PMCID: PMC5285475 .
- 586.Qiu H, Ren W, Yang Y, Zhu X, Mao G et al. (2018) Effects of cognitive behavioral therapy for depression on improving insomnia and quality of life in Chinese women with breast cancer: results of a randomized, controlled, multicenter trial. , Neuropsychiatr Dis Treat; 14, 2665-2673.
- 587.McCarthy M S, Matthews E E, Battaglia C, Meek P M. (2018) Feasibility of a Telemedicine-Delivered Cognitive Behavioral Therapy for Insomnia in Rural Breast Cancer Survivors. Oncol Nurs Forum. PubMed PMID: 45(5), 607-618.
- 588.Wal M van de, Servaes P, Berry R, Thewes B, Prins J. (2018) Cognitive Behavior Therapy for Fear of Cancer Recurrence: A Case Study. J Clin Psychol Med Settings. PubMed PMID: 29468568; PubMed Central PMCID: PMC6209054 25(4), 390-407.
- 589.Daniels S. (2015) Cognitive Behavior Therapy for Patients With Cancer. J Adv Pract Oncol. Jan-Feb;6(1): 54-6. Review. PubMed PMID: 26413374; PubMed Central PMCID: PMC4577033 .
- 590.Yi J C, Syrjala K L. (2017) Anxiety and Depression in Cancer Survivors. Med Clin North Am. Nov;101(6): 1099-1113. doi: 10.1016/j.mcna.2017.06.005. Epub 2017 Aug 18. Review. PubMed PMID: 28992857; PubMed Central PMCID: PMC5915316 .
- 591.Silva N M, MAD Santos, Rosado S R, Galvão C M, Sonobe H M. (2017) Psychological aspects of patients with intestinal stoma: integrative review. Rev Lat Am Enfermagem. Review. English, Portuguese, Spanish. PubMed PMID: 29236836; PubMed Central PMCID: PMC5738853 25(0), 2950-10.
- 592.Mosher C E, Winger J G, Given B A, Shahda S, Helft P R. (2017) A systematic review of psychosocial interventions for colorectal cancer patients. Support Care Cancer. 25(7), 2349-2362.
- 593.Sandler C X, Goldstein D, Horsfield S, Bennett B K, Friedlander M et al. (2017) Randomized Evaluation of Cognitive-Behavioral Therapy and Graded Exercise Therapy for Post-Cancer Fatigue. J Pain Symptom Manage. Jul;54(1): 74-84. doi: 10.1016/j.jpainsymman.2017.03.015. Epub 28502786.
- 594.Arch J J, Mitchell J L, Genung S R, Fisher R, Andorsky D J et al. (2019) A randomized controlled trial of a group acceptance-based intervention for cancer survivors experiencing anxiety at re-entry ('Valued Living'): study protocol. BMC Cancer. PubMed PMID: 30658621; PubMed Central PMCID: PMC6339433 1-11.
- 595.Zhu G, Zhang X, Wang Y, Xiong H, Zhao Y et al. (2016) Effects of exercise intervention in breast cancer survivors: a meta-analysis of 33 randomized controlled trails. Onco Targets Ther; 9 : 2153-68. doi: 10.2147/OTT.S97864. eCollection 2016. PubMed PMID: 27110131; PubMed Central PMCID:. 4835133.
- 596.Okuyama S, Jones W, Ricklefs C, Tran Z V. (2015) Psychosocial telephone interventions for patients with cancer and survivors: a systematic review. Psychooncology. Aug;24(8): 857-70. doi: 10.1002/pon.3704. Epub 2014 Oct 18. Review. PubMed PMID: 25328103.
- 597.Dong B, Xie C, Jing X, Lin L, Tian L. (2019) Yoga has a solid effect on cancer-related fatigue in patients with breast cancer: a meta-analysis. Breast Cancer Res Treat. Review. PubMed PMID: 177(1), 5-16.
- 598.El-Hashimi D, Gorey K M. (2019) Yoga-Specific Enhancement of Quality of Life Among Women With Breast Cancer: Systematic Review and Exploratory Meta-Analysis of Randomized Controlled Trials. J Evid Based Integr Med. Jan-Dec;24: 2515690X19828325. doi: 10.1177/2515690X19828325. PubMed PMID: 30791697; PubMed Central PMCID: PMC6388460 .
- 599.Wei C W, Wu Y C, Chen P Y, Chen P E, Chi C C et al. (2019) Effectiveness of Yoga Interventions in Breast Cancer-Related lymphedema: A systematic review. Complement Ther Clin Pract. Aug;36: 49-55. doi: 10.1016/j.ctcp.2019.05.004. Epub 2019 May 25. Review. PubMed PMID: 31383443.
- 600.Sohl S J, Danhauer S C, Birdee G S, Nicklas B J, Yacoub G et al. (2016) A brief yoga intervention implemented during chemotherapy: A randomized controlled pilot study. Complement Ther Med. Apr;25: 139-42. PubMed PMID: 26977123; PubMed Central PMCID: PMC4788038 .
- 601.Cramer H, Pokhrel B, Fester C, Meier B, Gass F et al. (2016) A randomized controlled bicenter trial of yoga for patients with colorectal cancer. Psychooncology. 10.1002/pon.3927. Epub 2015 Jul 29. PubMed PMID: 25(4), 412-20.
- 602.Durrani S, Contreras J, Mallaiah S, Cohen L, Milbury K. (2019) The Effects of Yoga in Helping Cancer Patients and Caregivers Manage the Stress of a Natural Disaster: A Brief Report on Hurricane Harvey. Integr Cancer Ther. Jan-Dec;18: 1534735419866923. doi: 10.1177/1534735419866923. PubMed PMID: 31364416; PubMed Central PMCID: PMC6669833 .
- 603.Zhang X, Wang X, Zhang B, Yang S, Liu D. (2019) Effects of acupuncture on breast cancer-related lymphoedema: a systematic review and meta-analysis of randomised controlled trials. Acupunct Med. PubMed PMID: 37(1), 16-24.
- 604.Bao T, Iris Zhi W, Vertosick E A, Li Q S, DeRito J et al. (2018) Acupuncture for breast cancer-related lymphedema: a randomized controlled trial. Breast Cancer Res Treat. 170(1), 77-87.
- 605.Zhu H, Li J, Peng Z, Huang Y, Lv X et al. (2017) Effectiveness of acupuncture for breast cancer related lymphedema: protocol for a single-blind, sham-controlled, randomized, multicenter trial. BMC Complement Altern Med. PubMed PMID: 28934950; PubMed Central PMCID: PMC5609040 17(467), 1-9.
- 606.Pan Y, Yang K, Shi X, Liang H, Shen X et al. (2018) Clinical Benefits of Acupuncture for the Reduction of Hormone Therapy-Related Side Effects in Breast Cancer Patients: A Systematic Review. Integr Cancer Ther. PubMed PMID: 30117343; PubMed Central PMCID: PMC6142070 17(3), 602-618.
- 607.Hasenoehrl T, Keilani M, Palma S, Crevenna R. (2019) Resistance exercise and breast cancer related lymphedema - a systematic review update. Disabil Rehabil. [Epub ahead of print] PubMed PMID: 1-10.
- 608.Duyur Cakıt B, Pervane Vural S, Ayhan F F. (2019) Complex Decongestive Therapy in Breast Cancer-Related Lymphedema: Does Obesity Affect the Outcome Negatively? Lymphat Res Biol. Feb;17(1): 45-50. doi: 10.1089/lrb.2017.0086. Epub 2018 Oct 3. PubMed PMID: 30281384.
- 609.Jeffs E, Ream E, Taylor C, Bick D. (2018) Clinical effectiveness of decongestive treatments on excess arm volume and patient-centered outcomes in women with early breast cancer-related arm lymphedema: a systematic review. JBI Database System Rev Implement Rep. PubMed PMID: 29419623; PubMed Central PMCID: PMC5828398 16(2), 453-506.
- 610.Myers J S, Mitchell M, Krigel S, Steinhoff A, Boyce-White A et al. (2019) Qigong intervention for breast cancer survivors with complaints of decreased cognitive function. Support Care Cancer. 27(4), 1395-1403.
- 611.Cifu G, Power M C, Shomstein S, Arem H. (2018) Mindfulness-based interventions and cognitive function among breast cancer survivors: a systematic review. BMC Cancer. PubMed PMID: 30477450; PubMed Central PMCID: PMC6260900 18(1163), 1-13.
- 612.Smith L, Gordon D, Scruton A, Yang L. (2016) The potential yield of Tai Chi in cancer survivorship. Future Sci OA. PubMed PMID: 28116134; PubMed Central PMCID: PMC5242198 20, 2-4.
- 613.Dennis D L, Waring J L, Payeur N, Cosby C, Daudt H M. (2013) Making lifestyle changes after colorectal cancer: insights for program development. Curr Oncol. Dec;20(6):e493-511. doi: 10.3747/co.20.1514. PubMed PMID: 24311950; PubMed Central PMCID: PMC3851346 .
- 614.Fong S S, Ng S S, Luk W S, Chung J W, Chung L M et al. (2013) Shoulder Mobility, Muscular Strength, and Quality of Life in Breast Cancer Survivors with and without Tai Chi Qigong Training. Evid Based Complement Alternat Med; doi: 10.1155/2013/787169. Epub. 3655570.
- 615.Shin E S, Seo K H, Lee S H, Jang J E, Jung Y M et al. (2016) Massage with or without aromatherapy for symptom relief in people with cancer. Cochrane Database Syst Rev. 3;(6):CD009873. doi: 10.1002/14651858.CD009873.pub3. Review. PubMed PMID: 27258432.
- 616.Imanishi J, Kuriyama H, Shigemori I, Watanabe S, Aihara Y et al. (2009) Anxiolytic effect of aromatherapy massage in patients with breast cancer. Evid Based Complement Alternat Med. Mar;6(1): 123-8. doi: 10.1093/ecam/nem073. Epub 2007 Jul 4. PubMed PMID: 18955225; PubMed Central PMCID: PMC2644279 .
- 617.Fiorelli A, Morgillo F, Milione R, Pace M C, Passavanti M B et al.Control of post-thoracotomy pain by transcutaneous electrical nerve stimulation: effect on serum cytokine levels, visual analogue scale, pulmonary function and medication. Eur J Cardiothorac Surg. 2012 Apr;41(4): 861-8; discussion 868. doi: 10.1093/ejcts/ezr108. Epub 2011 Dec 16. PubMed PMID: 22219414.
- 618.Chubak J, Hawkes R. (2016) Animal-Assisted Activities: Results From a Survey of Top-Ranked Pediatric Oncology Hospitals. J Pediatr Oncol Nurs. Epub 2015 Nov 20. PubMed PMID: 26589356; PubMed Central PMCID: PMC4874916 33(4), 289-96.

