Abstract
Religion and spirituality correlate positively with mental health. Although it is true generally spoken, it is too simplistic. On the basis of four reviews, from the period 1969-2013, the progress that was made and the achievements that were accomplished will be shown. In doing their empirical work the researchers managed to fit in with the evidence-based medicine approach. Thus, their work corresponded more and more to the standard scientific requirements. However, what are the consequences of that fit? And, in what sense could religion become part of ‘the most effective means of achieving health’? That asks for a critical ethical evaluation. Utilitarianism turns out to be the ethical basis of evidence-based medicine and achieving health is its central value. As a consequence, compared with religious traditions religion gets a different content with a strong experiential-expressive focus. That focus fits perfectly with modern Western values. Finally, the findings and discussions will enable us to plot four preliminary scenarios for the impact of research on religion and spirituality on psychiatry and mental health.
Author Contributions
Academic Editor: Wei Xu, School of Psychology, Nanjing Normal University
Checked for plagiarism: Yes
Review by: Single-blind
Copyright © 2017 Peter J. Verhagen, et al
 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Competing interests
The authors have declared that no competing interests exist.
Citation:
Introduction
Today professionals in the mental health professions (in particular in psychiatry, psychotherapy) are all familiar with reviews and meta-analyses according to the practice of evidence-based medicine and evidence based psychiatry. This practice is very helpful because the number of empirical studies on our special field of interest has become enormous. The research on religion and mental health is no exception to this rule. Important and informative reviews are available. For example, the second edition of Koenig’s Handbook of Religion and Health published in 2012 year is not just an updated version of the first edition published in 2001 1, 2, 3. It is in fact a second volume and together with the first edition both volumes cover more than three thousand empirical studies! So if one wants to have an overview of the field one should have a look at these volumes.
It is our aim to sketch the main line by discussing four reviews published between 1969 – 2013. The intention with this sketch is twofold. We want to highlight the improvements of this kind of research in the field of religion, spirituality and mental health. These improvements have very much contributed to the discussions about religion and spirituality in psychiatry in a positive way. However, there is still much controversy on this theme. Secondly, based on ethics of evidence-based psychiatry, it is our intention to reflect on the impact of this empirical research for the understanding and meaning of spirituality for mental health. About this impact not much has been said yet. Is it only profitable? Or are there any objections? What kind of objections are these then? We will see that criticism was already formulated from a theological perspective in 2003 4. The question was and is what kind of religion are we talking about.
The final question we want to answer is whether it would be possible to sketch scenarios of the requirements for research on religion and spirituality in psychiatry. Based on the certainties and uncertainties, the strengths and the weaknesses we have found, we will sketch four scenarios.
Review 1969 by Sanua
One of the first reviews, from the pre-evidence based era, was published by Sanua in the American Journal of Psychiatry in 1969. In fact he presented a quite original approach. He divided the studies he found according to five domains: religiousness and psychological adjustment, religiousness and deviancy, religiousness and authoritarianism, prejudice and religiousness, and religiousness and social values. He challenged the then common belief that religion would be a basis of sound mental health. And he claimed that he had not been able to find any empirical support for that claim. He concluded that religious education at that time did not seem to ensure healthier attitudes. He focused on the possible effects of religious education, and had to conclude that despite the fact that love is taught people tend to internalize the divisive role of religion.
It was a review from the pre-evidence based era, and therefore the interpretation appears to be more or less opinion based in our eyes today; no quantitative analysis of outcome measures, no information concerning how and on which grounds studies were selected and included or not, and so one. Therefore this review seems quite questionable today. However, his conclusion fitted very well in with the spirit of that time I guess, the sixties of the last century. Sanua stated: ‘The contention that religion as an institution has been instrumental in fostering general well-being, creativity, honesty, liberalism, and other qualities is not supported by empirical data.’ And he went on: ‘There are no scientific studies which show that religion is capable of serving mental health’ 5, 6. That was quite a statement in one of the leading Journals of Psychiatry, the American Journal of Psychiatry (AJP).
Batson & Ventis 7 commented on the findings of Sanua (and others). It is, as they write, as in the parable of the blind men describing an elephant. Therefore, Sanua is wrong and right at the same time. The reason for contradictory conclusions can be understood on basis of different conceptions the authors have of mental health and of different ways of being religious. That will prove to be a common thread in what follows (see also 8, 9, 10). (For a summary of characteristics of the four studies, see Table 1.)
Table 1. Summary of four reviews of empirical studies on religion/spirituality and mental health| Four reviews/meta-analyses | Sanua 1969 | Bergin 1983 | Hackney & Sanders 2003 | Bonelli &Koenig 2013 |
| Meta-analysis | - | + | + | + |
| Period | 1928-1967 (no explicit reason) | 1951-1979 | 1990-2001 (explicit choice) | 1990-2010 |
| (no explicit reason) | (explicit choice) | |||
| Selection criteria; Number of studies included | No selection procedure | Explicit procedure; 241 | Explicit and consistent procedure; 352 | Explicit and consistent procedure; 433 |
| Categorisation of studies theory based | 5 domains4 | Religion as religious involvement | Coding of six categories5 | Religious/spiritual involvement related to diagnostic groups according to ICD-10 |
| Quality of methods used in the studies found | Minimal description of methods | Analysis of effect sizes | Analysis of multiple effect sizes | Full assessment of quality (based on Cooper 11) |
| Level of evidence | - | - | - | + (based on Bonelli & Wenning 12) |
| Conclusion | No empirical support for a positive correlation. | Data ambiguities ask for better specifications of concepts and methods. | Depending on definitions different types and strengths of the correlations are found. | The available evidence (good, some, insufficient, no) differs by psychiatric disorder. |
Intermezzo I: Criticism and Worry
In 1986 an important paper was published in the same journal. The article was a clear and in a sense alarming signal. The authors presented a systematic analysis of research on religious variables in four major psychiatric journals, including AJP, in the period 1978-1982 13. One could say that publication trends on religion in leading journals were at that time a kind of genre, which Larson and colleagues joined 14, 15. In any case the recipe was known.
Larson and colleagues reviewed 2.348 psychiatric articles and were able to find 59 studies in which a religious variable was included. Without going into detail, at that time, religious variables were seldom used in research and religious research was seldom cited. There appeared to be a lack of knowledge and skills needed to evaluate religion, was the undeniable conclusion of the authors.
The reason for this study was a major concern. It was well known that there was and still is a disparity of religious beliefs and spirituality of mental health professionals and the general public. It should not influence psychiatric practice, but it inevitably did, not only in referral behavior but also in treatment choice. That disparity also meant a different appreciation of the function of religion and spirituality between the professionals and the public. This raises two questions. How does this lack of inclusion of religious variables disrupt the (at that time forthcoming) evidence-based practice? Because if religious or spiritual variables are not included what would that mean for the usefulness of research outcomes in certain cases? Secondly, how will the dialogue on values and preferences with regard to treatment recommendations between mental health professional and patient go on if there is such a difference in appreciation of the meaning of religion and spirituality? The risk of misunderstanding was and still is not imaginary. A potential conflict hung in the air. Unfortunately, another group of authors had to report in 1998 that there was no improvement 16.
Review 1983 by Bergin
Times changed. The second review was published in 1983, written by the at that time well-known psychotherapist Alan Bergin 17. He made it very clear that review of empirical data is not just an empirical matter! Other issues are involved. In the first place, values and ideology influence theoretical assumptions. For instance, what was true at that time and still is today is that main assumptions of dominant theories are naturalistic and humanistic rather than theistic and spiritual. That means that it might happen, and it obviously did happen, that ideological choices were taken as facts, which they certainly are not. Another influential aspect is the already mentioned religious noninvolvement of mental health professionals in contrast with the substantial involvement of the general population in religion and spirituality. It turned out to be true, religion did not disappear but it did change and is still changing. However, psychiatrists and other mental health professionals are still reluctant to recognize that reality. A third influential aspect Bergin brought out was that because of these conceptual and attitudinal biases religion and spirituality were excluded from measurement or included in such a way as to confirm prejudices with regard to religion and mental health. These three issues still deserve to be kept in mind when one studies empirical surveys on religion and mental health!
Bergin included 24 studies from 1951-1979; that covers more or less the period Sanua looked at, but they share just three references. Bergin also presented a quantitative sum of data. Therefore he included only studies that had at least one religiosity measure and one clinical pathology measure. His findings set the trend for the years to come. On a total of 30 outcome measures only 7 (23%) showed a negative relationship between religion and health. A positive relationship was shown by 47%, and the remaining 30% showed a neutral relationship. Bergin showed himself a modest man, nevertheless. He cleverly stated that he had not found support for the assumed overall negative relationship between religion and mental health, but he admitted at the same time that he had only found marginal support for the positive effect of religion. Part of the problem were the limitations of measurement and methodology, which actually still are problematic issues, despite the overall improvements. Another important improvement made by Bergin was his attempt to reckon with the fact that religion is a multidimensional concept, and that different aspects of religiosity are related to different aspects of mental health, and that therefore religiosity is not just a matter of healthy or unhealthy religiosity. In other words, measurement of religiosity is a complicated matter and asks for careful attention. That will be the next step forward. However, since Bergin’s publication the results of reviews have confirmed his outcome. There always appear to be mixed results, but the overall finding is a positive correlation between religion, spirituality and mental health (see also 4 p. 22). By the way, it was not Bergin’s first paper on religious values, psychotherapy and mental health 18. Just to realize the impact of his ‘coming out’: ‘A bombshell hit the world of empirical psychotherapy research in 1980 when Bergin argued that despite their reticence, psychotherapists had a set of values about a good life which could be called ‘religious’, and that such values correlated positively with mental health’ (19 p. 236; 20).
Intermezzo II: DSM-IV
Meanwhile changes were coming on an entirely different front. In DSM-IV some major interventions were made with regard to religion and spirituality. The content of the DSM-IV glossary of technical terms had been rewritten in-depth. Larson and colleagues 21 found that in the DSM-III-R glossary religion was more frequently referred to. They could not conclude otherwise than that that glossary showed a bias against religion and a remarkable insensitivity in interpreting religion. The new glossary was an improvement. Secondly, the chapter on cultural sensitivity was introduced, including five items: cultural identity, cultural explanations of the illness, cultural factors related to the environment and level of functioning, cultural elements of the relationship between the individual and the clinician, cultural assessment for diagnosis and care 22. It is obvious that religion and spirituality are integral parts of these five items. The third major change was that a code Religious or Spiritual problem was introduced. That made it possible to take religious and spiritual problems into account and made it even possible to pay attention to these problems, if necessary. Let us conclude that DSM became less biased against, more sensitive to religion and spiritual issues; the changes were maintained in DSM-5™ 23, 24, 25.
Meta-Analysis: A Representative Example 2003 by Hackney and Sanders
Extensive research has been conducted and comprehensive data are available, but the relationship between religion, spirituality and mental health is still disputed. Indeed, there are some clear examples of a negative effect of spirituality or religion on mental health. Nevertheless, a majority of experts seem to agree that in general the relationship between religion, spirituality and mental health can be qualified as positive. A preponderance of studies indicates that religious individuals fare better than their secular counterparts in psychological disorders.
Instead of summarizing studies it is interesting to look in some detail at one of the frequently cited meta-analyses, done by Hackney and Sanders 26, 27. One of the main difficulties and an arena for disagreement is the fact that researchers deploy diverse definitions of scales of religion, spirituality and mental health. Religion, spirituality and mental health are multidimensional constructs and we still wrestle with a lack of (scholarly) consensus on how to define these constructs. The authors solved the problem in a rather elegant way. They looked at the way religion and mental health were defined in the studies they included (35 studies between 1990 and 2001) and developed a classification scheme along the following lines. Definitions found in these 35 studies that focused on the social and behavioral aspects of religion (e.g. attendance of services, participation in church activities) were coded as ‘institutional religion’. Definitions that focused on beliefs involved in religious activity (e.g. ideology, attitudes, belief salience, and fundamentalism) were coded as ‘ideological religion’. Definitions that focused on personal, internalized devotion (e.g. emotional attachment to God, devotional intensity) were coded as ‘personal devotion’.
Hackney and Sanders also coded definitions of mental health or psychological adjustment. Definitions focusing on the unhappy aspects of mental health (e.g. depression, anxiety) were coded as ‘psychological distress’. Definitions that focused on positive feelings regarding the self and one’s life in general (e.g. self-esteem, happiness) were coded as ‘life satisfaction’. Definitions of psychological adjustment focused on more growth oriented and humanistic aspects of mental health (e.g. identity integration, existential well-being) were coded as ‘self-actualization’.
The authors found 264 effect sizes, only 78 of them were negative; most of them near zero or non-significant. The results showed that variation in definition or type of religiosity is one systematic source of variation in the effect sizes. The results also showed that the religiosity main effect took the form of significant increases in mean effect size as one proceeds from institutional religiosity to ideology to personal devotion. Also the variation in definitions of mental health is a source of systematic variation. The main effect took the form of significant increases in mean effect size as one proceeds from definitions centered on low psychological distress to life satisfaction to self-actualization. The authors also focused on the issue of interaction between types of religiosity and types of mental health. For example, when religiosity is defined as personal devotion a very slight increase in mean effect size from lack of distress to life satisfaction is followed by a large increase as one proceeds to self-actualization.
To summarize, regardless of any consideration of religiosity or mental health definitions religiosity may be said to have a moderate positive overall, helpful, salutary relationship with mental health; a consistent finding over the years. Allen Bergin set the tone 15. At the same time each position that has been taken in the debate is supported: positive relationships (between personal devotion and self-actualization), negative relationships (between institutional religion and psychological distress), and non-significant (between ideological religion and psychological distress).
Review 2013 by Bonelli & Koenig
The fourth and most recent review I want to highlight was published in 2013, written by Bonelli, Sigmund Freud University, Vienna, Austria, and Koenig, Duke University, Durham, USA 6, 28. They examined the period 1990-2010 and looked for original research in the top 25% of psychiatry and neurology journals according to the ISI (Inst Scientific Inf.) journals citation index 2010. They found 43 studies that met these criteria. They also used criteria for rating the quality of each study, which is an important addition and improvement given the usual criticism on studies on religion and mental health. These criteria look at 1) study design, 2) sampling method, 3) number of measures, 4) quality of measures, 5) quality of mental health outcome measures, 6) contamination between outcome and religion/spirituality measures, 7) inclusion of control variables, 8) statistical method.
The results were placed into six categories: 1) no association (NA), 2) at least one significant positive association and no significant negative associations (POS), 3) positive association, but significance level borderline, 4) at least one significant negative association with better mental health and no significant positive ones (NEG), 5) negative association, but significance level borderline, 6) mixed, that means both significant positive and negative associations (MIX).
They divided the results according to diagnostic groups following ICD-10 and concluded that 72% of the studies reported a positive relationship between religious involvement and better mental health. Of course one would like to know what is meant by ‘religious involvement’. Although more than 40 different measures of religion/spirituality were used in these studies, all assessed the degree of involvement. That does not say too much compared to what was stated in the third review, but that is what Bonelli and Koenig have to say on this.
Of the studies 2% showed a trend toward positive association, 2% showed no association, and 19 % demonstrated mixed results, 5 % showed a negative association. One could also formulate that 93% (72 + 2+ 19) found at least one positive association, whereas 23% reported at least one negative relationship. Regarding the diagnostics groups, all studies on dementia 2, suicide 3 and neurosis 3 found a positive association, 79% of the studies on depression 19 and 67 % of those on substance abuse 9. Most findings in schizophrenia 5 were mixed or positive, in bipolar disorder 2 mixed or negative.
They also make an important statement on the quality aspects of these studies. According to their rating of the quality of studies before and after 2000 they found an improvement in quality of methodology and design.
The authors compared their results with two earlier reviews published in 1986 (13; discussed in Intermezzo I) and 1992 29 in the AJP. Their review in fact serves as a follow-up of these two. The 1992 study paid special attention to aspects of religious involvement and found that dimensions like ceremony, social support, prayer and relationship with God do have positive associations with mental health. However, at that time the authors were surprised by the fact that even when a religious variable was specified in the majority of the cases there were no reported efforts either to formulate a hypothesis or to test the association between religious measures and mental health. In their case for only 22% of the measures a hypothesis was specified and of these 22% only 40% reported the results. Bonelli and Koenig conclude that their findings are similar to those reported by these earlier reviews, but that research has improved. That does not mean that there are no methodological issues left. To mention a few: Religion and spirituality are multidimensional constructs, and therefore it is necessary to specify which dimensions are assessed. Especially spirituality is a difficult concept if one wants to avoid an all too large similarity with religion or mental health. And what exactly is meant by non-religiousness, atheism or agnosticism? Another issue is the fact the most studies are cross-sectional, therefore giving no indication about causality. Religious factors may function in different ways across the life span. And one should always realize that it is not always clear for what reason people are religiously involved, including reasons that have nothing to do with religious beliefs (e.g. ‘risk avoidance’).
Evidence-Based Practice
We have no reason to doubt the results of these reviews. Given these outcomes, the next question is whether and how these findings become integrated in clinical practice. This brings us to the area of evidence-based practice. We already suggested some potential difficulties and we will now look for possible answers. However, these potential difficulties are real. We will first look at the evidence-based practice itself, and secondly we want to examine in what why the ethics of evidence-based medicine and psychiatry influence the concept of religion. Evidence-based medicine is about achieving health. However, endures the concept health itself with classical religious traditions or is a new type of religiosity more appropriate? And if so, what type?
In every guideline, handbook or recommendation on evidence-based practice one can find that at a certain moment the findings need to be summarized, after examining the literature, and then value judgments or preferences should be applied 30. For instance: ‘Having made estimates of the consequences of alternative strategies, value judgments about the relative desirability or undesirability of possible outcomes becomes necessary to allow treatment recommendations. We will use the term preferences synonymously with values or value judgments in referring to the process of trading off positive and negative consequences of alternative management strategies.’ (30 p. 1837). The final step is, after all, how to apply the results to the patient. With ignoring all sorts of aspects of this final step, an important point is the demand for the values and expectations of the patient. Of course, this means values and expectations with regard to the treatment that is recommended and the prevention of unwanted outcomes. Patient values in clinical decision making are of great importance, is said time and again (31 p. 119). At the same time it is not very clear how patients’ values are integrated in research evidence and clinical expertise of the professional. That is probably even more true for religious values. For instance, if religious or spiritual issues are important in any way, is the clinician prepared or willing to include a religious or spiritual aspect in the framing of the search question? And what has the patient to say to that? In other words who is the owner of the critical appraisal? Then, as Gupta brings forwards (31 p. 120), ‘what version of health is valued by the methods used and the outcomes measured?’ This is really an extremely important question and illustrates very clearly that values are implicitly or explicitly present from the very first step of the evidence-based recommendations process. In other words, is religion or spirituality or meaning making seen as integral part of (mental) health, on what grounds? And if not, on what grounds is it rejected?
This is one part of the problematic use of evidence-based medicine in psychiatry and religion and spirituality. There is another issue to ask questions about. Obviously the researchers in the field of religion and psychiatry intend to create greater awareness of the meaning of religion and spirituality in psychiatry and psychotherapy. And they tried to achieve this by conducting their research in accordance with current quality requirements. As we have seen, they have been quite successful in achieving this goal. But why? Is it worth it ? To answer these questions it is useful to look at the ethical basis of evidence-based medicine (31 pp. 117-148). According to the analysis of Gupta ‘we ought to pursue evidence-based medicine because that is the only way to pursue the most effective means of achieving health. Health is the central value and the justification for applying evidence-based medicine. Gupta convincingly explains that this approach means a consequentialist point of view. What counts is the actual consequence of an act. That is how it can be concluded whether an act is morally right or not. There must be a consequence that is good in itself: achieving, improving health is such a consequence. This type of ethical reasoning belongs to the school of utilitarianism. The slogan for utilitarianism is ‘the greatest good of the greatest number’ (32 p. 514).
The immediate question is does religion fit in such an approach? Is religion in that sense a (useful) element of the ‘most effective means of achieving health’? That is a difficult question, which cannot be answered just like that.
Yet it is difficult to say whether or to what extent medicine’s emergent alliance with religion is really good news for people of faith. Given the highly individualized character of religious belief in contemporary American culture, the religion that medicine has (re)discovered may be no more than a simulacrum of any one of those several ancient, historical traditions we typically think of as religions. While this point probably does not make much difference to those whose overarching concern is the physical well-being of the individual and the way religion can contribute positively to that health or to those concerned with meeting the needs of the medical consumer, it does matter theologically – at least to those of us who believe that theology has something to say about the way things really are. (4 p. 20)
This lengthy quotation draws on several discussion points. Most importantly, the authors draw our attention to a difference between religion and religious traditions. Religious traditions are about living and dying faithfully. Religion in its alliance with medicine is about living healthy. Living and dying faithfully is living and dying in fruitful relationships with the deity, oneself and other people, and the world around, ‘whether in sickness or in health’ (4 p. 21). So what kind of religion are we talking about? In fact, although participants in empirical studies belong to religious traditions, religion is understood in a more generic way. What does that mean? Shuman & Meador refer to the analysis by the theologian Lindbeck 33. He explains that in modern times propositional understanding of religion has lost its popularity and that what he calls an experiential-expressive understanding of religion is in the ascendency (33 p. 5). ‘Experiential-expressive’ means a focus on the experience of the religious person. Doctrines function as nondiscursive symbols of inner feelings, attitudes and existential orientations (33 pp. 2-3). It is my opinion that this individualized type of religion exactly fits within the cultural values of the modern world.
Cultural Values: Two Dimensions
The values surveys of the European and World Values Studies (EVS/WVS) are the largest investigations of attitudes, values and beliefs around the world and are designed to provide a comprehensive measurement of all major areas of human concern, including religion. The data show that on the one hand economic development is associated with a shift away from traditional values. Based on the work of Inglehart it is shown that the differences between advanced societies and low-income societies across a wide range of values can be plotted along two dimensions: traditional versus secular-rational values and survival versus self-expression values 34, 35. According to the view of the authors on modernization the traditional versus secular-rational dimension reflects changes linked with the transition from an agrarian to an industrial society, associated with rationalization and secularization. The second dimension is linked with the level of existential security and linked with the transition from industrial to post-industrial or knowledge societies. When survival is less secure survival strategies are more in the foreground. When survival can be taken for granted other goals and values become important.
The traditional versus secular-rational values dimension reflects the contrast between societies in which religion is important and those in which it is not. In traditional societies God and religion (belief in heaven and in hell) are very important along with work, children need to learn obedience and religious faith, absolute standards are emphasized (abortion, suicide, euthanasia, divorce are never justifiable) along with respect for authority and national pride. And people describe themselves as ‘religious persons’. Secular-rational values emphasize the opposite. The second dimension reflects the polarization between survival and self-expression values. Survival values are characterized by priority to economic and physical security over self-expression and quality-of-life. People who live survival oriented reject foreigners, homosexuals. Hard work is one of the most important things to teach children, imagination, tolerance and respect for others are not the most important things to teach children. And again, self-expression values emphasize the opposite.
Iglehart and Baker 34 found evidence that orientations have shifted from traditional toward secular-rational values in almost all industrial societies. And when a society starts to become a knowledge society a new shift appears, from survival to self-expression values. Self-expression tends to interpersonal trust, tolerance, subjective well-being, quality of life and self expression. That focus on self-expression is what we immediately recognize in the analysis of the kind of religion we are looking for. That type of religion fits perfectly into this cultural profile. In that sense is the alliance between medicine and religion, and between psychiatry and religion accompanied by a culturally modern understanding of religion, at least in the western world. We recognize it especially in the approach of the third review 26.
How to Proceed? Uncertainties and Scenarios!
In this final paragraph I will give a preliminary sketch of a foresight based on the literature by identifying certainties and uncertainties and their impact with regard to the research on religion and spirituality and (mental) health (Fig. 1; 2, 10, 27, 36, 37, 38. Secondly, I will formulate possible scenarios and desired developments (Fig. 2).
In what follows I use the so-called scenario method 39, 40. This method has been developed for strategic planning.Strategic planning could be very useful to help forward the research field and clinical
practice of religion and spirituality in psychiatry. First we need to have a pictiure of the developments in the field, then we have to decide which of these developments are certain and which are uncertain. The next step is to choose two key uncertainties based on their level of uncertainty and their impact in the field. Of course in a regular procedure of the scenario method inventory making and decision making is based on analysis of research and documents and on interviews with experts and stakeholders. In my proposal the material I have presented in this paper is leading.
Fig 1 shows two axis and four quadrants. In the left upper quadrant the advances are plotted. However, their impact in research and clinical practice is still low. In the left lower quadrant I plotted the problematic issues that still surround the field of inquiry and that contribute to high uncertainty, but still have low impact. On the right upper side we see that professional development and policy making certainly make the difference because of their high impact. In the right lower quadrant we see the most problematic fourth part. Unawareness and lack of consensus in professional documents and scientific journals will continue to have high impact and great uncertainty in the field will be maintained.
Fig 1.Identification of uncertainties with regard to the impact of research on religion/spirituality on psychiatry and mental health care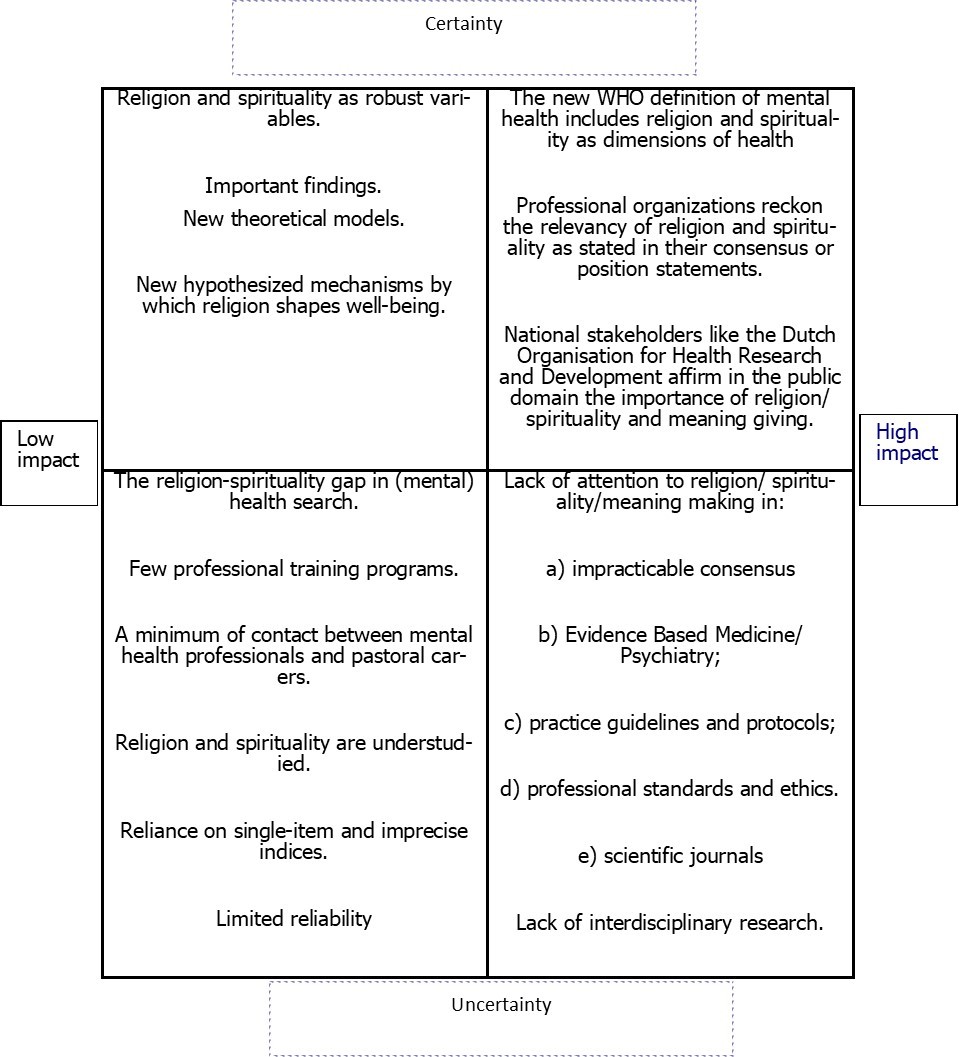
In line with the reasoning in this contribution two key uncertainties can be identified: attention to religion and spirituality by evidence based medicine/psychiatry and consensus on religion and spirituality in psychiatry (Fig 2). If consensus is impracticable then attention to religion and spirituality in psychiatry will remain dependent on the interest of individual professionals and a few interested research groups. If consensus remains impracticable and interest is low then all sorts of biases will continue to play their disturbing role at the expense of good research, and in the end at the expense of the welfare of the patient. On the other hand, in case of high consensus and high attention the application of data in clinical practice will include values and preferences among which religion and spirituality. In case evidence based medicine/psychiatry falls short with attention to religion and spirituality in psychiatry despite consensus, unmet need for data and their proper application will remain.
Fig.2. Scenarios for the impact of research on religion/spirituality on psychiatry and mental health care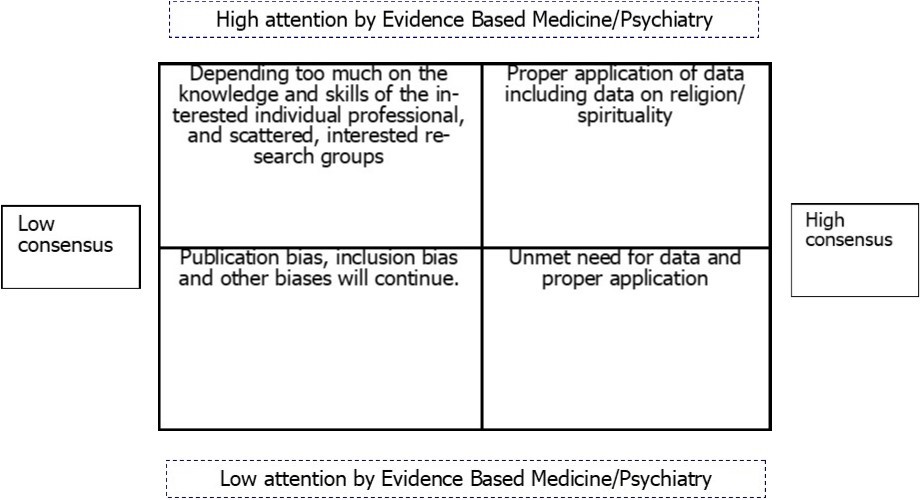
Conclusion
In other words and to summarize, the first aim of the historical overview was to show that empirical research improved over the years, and research syntheses improved as well. There is good evidence, that religious involvement is correlated with mental health in three major domains of psychiatry: depressions, substance abuse and suicide. There is some evidence for two other domains: stress related disorders and organic mental disorder. There is insufficient evidence for bipolar disorder and schizophrenia, and no evidence for a lot of other disorders, which of course means that more at research is needed. Most important is the finding thatat least in 20years, but even longer, the findings are fairly consistent. The majority of studies do show positive associations between religious involvement and mental health. However, one should not close one’s eyes for the fact that also mixed and negative results reappear every time.
The second aim was to show that within the context of evidence-based medicine the pursuit of health has consequences, perhaps unexpected, for our understanding of religion in contrast with what we call the classical religious traditions. The general matter of ethics with regard to evidence based psychiatry turned out to be important for the evaluation of evidence on religion and spirituality in psychiatry. What kind of religion are we talking about within this perspective of evidence? A critical theological evaluation and the use of the European and World Values Studies helped us to find an explanation.
Finally, based on our findings and discussions we were able to sketch four scenarios with regard to the impact of research on religion and spirituality on psychiatry and mental health care. Our most important conclusion is that we have to work towards an ethical consensus 3.
References
- 2.H G Koenig, D E King, V B Carson. (2012) Handbook of religion and health. Second Edition. , Oxford
- 3.P J Verhagen. (2013) Psychiatry and religion: Values. , Research Data and Professionalism. Minerva Psichiatr 54, 149-164.
- 4.J, K G Meador. (2003) Heal thyself. Spirituality, medicine, and the distortion of Christianity. , Oxford
- 5.V D Sanua. (1969) Religion, Mental health, and personality: A review of empirical studies. , Am J Psychiatry 125, 1203-1213.
- 6.R M Bonelli, H G Koenig. (2013) Mental disorders, religion and spirituality. , J Relig Health 52, 657-673.
- 7.C D Batson.and Ventis, W.L.(1982) The religious experience. A social-psychological perspective. , Oxford
- 10.Dengah H J F. (2017) Religion as cultural models: Developing an emic measure of religiosity. , J Sci Study Relig 56, 104-125.
- 11.Cooper H. (2010) research synthesis and meta-analysis. A step-by step approach. 4th Edition , Sage, Los Angeles .
- 12.R M Bonelli, G K Wenning. (2010) Pharmacological management of Huntington’s disease: An evidence based review. Curr Pharm Des. 12, 2701-2720.
- 13.D B Larson, E M Pattison, D G Blazer, A R Omaran, B H Kaplan. (1986) Systematic analysis of research on religious variables in four major psychiatric journals. , Am J Psychiatry 143, 1978-1982.
- 14.A. (1970) A study of articles on religion in major sociology journals: Some preliminary findings. , J Sci Study Relig 11, 165-170.
- 15.Capps D, Ransohoff P, Rambo L. (1976) Publication trends in the psychology of religion to. , J Sci Study Relig 15, 15-28.
- 16.A J Weaver, J A Samford, D B Larson, L A, H G Koenig et al. (1998) A systematic review of research on religion in four major psychiatric journals:. , J Nerv Ment Dis 186, 187-189.
- 17.A E Bergin. (1983) Religiosity and mental health: a critical reevaluation and meta-analysis. Prof Psychol Res Pr 14, 170-184.
- 19.Holmes J. (1999) Ethical aspects of the psychotherapies. Psychiatric ethics, 3rd Ed In S. Bloch, P. Chodoff, and A. Green (eds.) , Oxford 225-243.
- 20.Richards Scott, P. (2016) Psychotherapy and religious values: Remembering Allen E. Bergin’s legacy. , Open Theology 2, 876-880.
- 21.D B Larson, S B Thielman, M A Greenwold, J S Lyons, Post. (1993) Religious content in the DSM-III-R glossary of technical terms. , Am J Psychiatry 150, 1884-1885.
- 23.American Psychiatric Association (2014) Diagnostic and statistical manual of mental disorders. Fifth Edition. DSM-5™, American Psychiatric Publishing , Washington .
- 24.Lukoff D, C R, D M Gellerman, Glickman L, H G Koenig. (2010) Religious and spiritual considerations in psychiatric diagnosis: Considerations for the DSM-V. In. , Wiley-Blackwell, Chichester 423-444.
- 25.J R Peteet, G F Lu, W E Narrow. (2011) Religious and spiritual issues in psychiatric diagnosis. A research agenda for DSM-V, American Psychiatric Association. , Arlington
- 26.C H Hackney, G S Sanders. (2003) Religiosity and mental health: A Meta-Analysis of recent studies. , J Sci Study Relig 42, 43-55.
- 27.C H Hackney. (2010) Religion and mental health: What do you mean when you say ‘religion’? What do you mean when you say ‘mental health’? In.
- 28.Bonelli M. (2014) Religiosität in der Psychiatrie – zum aktuellen Wissensstand [Religion in psychiatry – the current state of knowledge]. In.
- 29.D B Larson, K A Sherrill, J S Lyons, F C Craigie, S B Thielman. (1992) Associations between dimensions of religious commitment and mental health reported. in the American Journal of Psychiatry and Archives of General Psychiatry: 1978-1989. Am J Psychiatry,.149 557-559.
- 30.G H, Sinclair J, D J Cook, Glasziou P. (1999) Users’ guides to the medical literature. XVI. How to use a treatment recommendation. , J Am Med Assoc 281, 1836-1843.
- 32.Fulford K W M, Thornton T, Graham G. (2006) Oxford textbook of philosophy and psychiatry. , Oxford
- 33.G A Lindbeck. (2009) The nature of doctrine. Religion and theology in a postliberal age. , Westminster
- 34.Inglehart R, W E Baker. (2000) Modernization, cultural change, and the persistence of traditional values. , Am Sociol Rev 65.
- 35.Inglehart R, Welzel C. (2010) Changing mass priorities: The link between modernization and democracy. , Perspectives on Politics 8, 551-567.
- 36.P C Hill, K I Pargament. (2003) Advances in the conceptualization of measurement of religion and spirituality. , Am Psychol 58, 64-74.
- 37.Dein S, Cook C C H, Koenig H. (2012) Religion, spirituality, and mental health. Current controversies and future directions. , J Nerv Ment Dis 200, 852-855.
- 38.Dein S. (2014) Religion and mental health: A critical appraisal of the literature. World Cult Psychiatry Res Rev. 9, 42-46.
