Abstract
The medial calcaneal nerve (MCN) is the first branch of the posterior tibial nerve (PTN) in the porta pedis, enervates the skin of the heel and medial side of the foot. Heel pain is a common condition encountered by physicians, and this may have a significant clinical association with the MCN’s branching pattern. This study was to identify branching pattern variations in the medial calcaneal neurovascular bundle. This study was carried out using 60lower limbs of formalin-embalmed cadavers, using the tarsal tunnel dissection method for 30right and 30 left lower limbs. The medial calcaneal neurovascular bundle course was identified by exposing the PTN and its branches from the distal end of the leg toward the plantar surface beyond its bifurcation and resecting the skin and flexor retinaculum. Many MCN branching pattern variations (specifically concerning origins, numbers, and levels of branching) were observed. In the right foot a single branch was present in 21 specimens (70%), while two branches were observed in nine specimens (30%). In the left foot, a single branch was present in 22 specimens (73.3%) and two branches were present in 8 specimens (26.7%). In this study, two branches originate from lateral planter artery is the most common observation. This study concludes that a single MCN originating from the TN is the most common variant. Two medial calcaneal arteries (MCAs) originating from the LPA is also common.
Author Contributions
Academic Editor: Abdelmonem Awad Mustafa Hegazy, Professor and Former Chairman of Anatomy and Embryology Department, Faculty of Medicine, Zagazig University, Egypt.
Checked for plagiarism: Yes
Review by: Single-blind
Copyright © 2019 Khalid Musa Fadlelmula Awadelseid
 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Competing interests
The authors have declared that no competing interests exist.
Citation:
Introduction
The porta pedis is an area at the medial aspect of the ankle joint where the tendons of the flexor muscles extend from the leg to the sole of the foot. The tibial nerve (TN) and posterior tibial vessels are found between the tendons, fixed in their position by the flexor retinaculum 1. The roof of the tarsal tunnel (porta pedis) is the flexor retinaculum and its floor is formed by the medial surface of the talus (sustentaculum tali) as well as the superficial and deep aponeurosis of the leg. Anteriorly, the flexor retinaculum is attached to the anteromedial surface of the medial malleolus; posteriorly, it is attached to the medial tuberosity. The inferior border is the abductor hallucis muscle. The retinaculum becomes thicker at its lower margin, splitting to enclose the abductor hallucis muscle. Below this muscle, the two layers unite to become the plantar fascia. Then, the structures pass through the tarsal tunnel from the medial to lateral direction 3.
The neurovascular bundle in the tarsal tunnel consists of the TN, posterior tibial artery (PTA), and venae comitantes. It descends along the posterior border of the tibia and lies deep in the proximal part of the leg distally; however, it becomes superficial and is covered only by fascia and skin. 2.
The medial calcaneal nerve (MCN) is a cutaneous branch of the TN before its bifurcation into the medial plantar nerve (MPN) and lateral plantar nerve (LPN).The MCN enervates the heel skin (weight-bearing area) and medial side of the sole of the foot. Anatomical studies have described the TN and its terminal branches, the MPN and LPN .However, although it may have a clinical association with heel pain, which is a common complaint encountered by podiatric and orthopedic surgeons 4. The MCN has been less frequently described than the TN. The present study was designed to identify branching pattern variations of the MCN and medial calcaneal artery (MCA), which may provide anatomical data for diagnostic and therapeutic procedures of tarsal region conditions, such as entrapment of the TN or one of its branches in the tarsal tunnel, and podiatric instrumentation, such as the placement of percutaneous pins in the calcaneus used for introducing an external fixator 5.
Materials and Methods
The materials for this study were collected from 60lower limbs of formalin-embalmed cadavers from the Department of Anatomy, Faculty of Medicine, Jazan University (60 specimens). The data were collected using the standard dissection method of the tarsal tunnels. The skin was reflected using a standard skin incision at the lower limb. Subcutaneous tissue was removed 15 cm proximal to the medial malleolus and distally to the midplantar surface in each foot. The deep fascia, along with the flexor retinaculum, was cut. Then the neurovascular bundle, which was wrapped in its own sheath, was then incised, and the vascular structures were separated from the nerve. The TN and posterior tibial artery, along with the venae comitantes, were exposed from the distal end of leg toward the plantar surface beyond its bifurcation by resecting the abductor hallucis muscle Figure 1. If present; tortuosity of vessels was also noted. Soft tissues, muscles attached to the medial malleolus of the tibia, and the medial tubercle of the calcaneus were resected to make the medial malleolus and medial tubercle of the calcaneus visible. The medial calcaneal branches (MCBs) of the TN were noted and counted, and their origins were detected. The number and origin of MCAs were also noted and counted.
Figure 1.Removal of the skin and subcutaneous tissues 15 cm proximal to the medial malleolus to the midplantar surface of the foot.
A checklist was designed, and the data were collected. The data were entered into the computer and analyzed using IBM SPSS software package version 20.0. Qualitative data were described using number and percent values, and quantitative data were described using range (minimum and maximum), mean, standard deviation, and median. Comparison between the left and right sides regarding categorical variables was conducted using the marginal homogeneity test, while the distributions of quantitative variables were tested for normality using the Kolmogorov–Smirnov, Shapiro–Wilk, and D'Agstino tests. If the results revealed a normal data distribution, parametric tests were applied. If the data were abnormally distributed, nonparametric tests were used. For normally distributed data, the paired t-test was used to analyze two paired data. For abnormally distributed data, the Wilcoxon signed-ranks test was used to analyze two paired data 6, 7.
Results
In the right foot, a single MCN was present in 21 specimens (70%) while in the left foot a single branch observed in 22 specimens (73.3%) (Table 1) Figure 2, Figure 3).
Table 1. Numbers of Medial Calcaneal Nerves (Mcns) in the Right and Left Foot| Number of MCNs | Foot | MHx2 | p | |||
| Right (n = 30) | Left (n = 30) | |||||
| No. | % | No. | % | |||
| One branch | 21 | 70.0 | 22 | 73.3 | 0.302 | 0.763 |
| Two branches | 9 | 30.0 | 8 | 26.7 | ||
| Three branches | 0 | 0.0 | 0 | 0.0 | ||
| Four branches | 0 | 0.0 | 0 | 0.0 | ||
| More than four | 0 | 0.0 | 0 | 0.0 | ||
Figure 2.Numbers of medial calcaneal nerves (MCNs).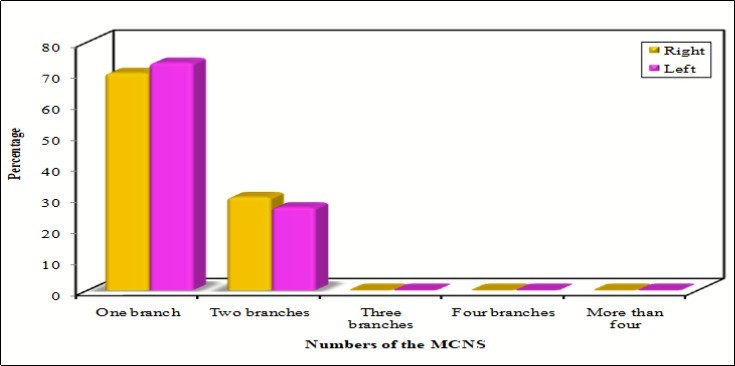
Figure 3.Photographs of the ankle region in (A) and (B) showing a single medial calcaneal nerve (MCN) originating from the tibial nerve (TN) deep in the tarsal tunnel.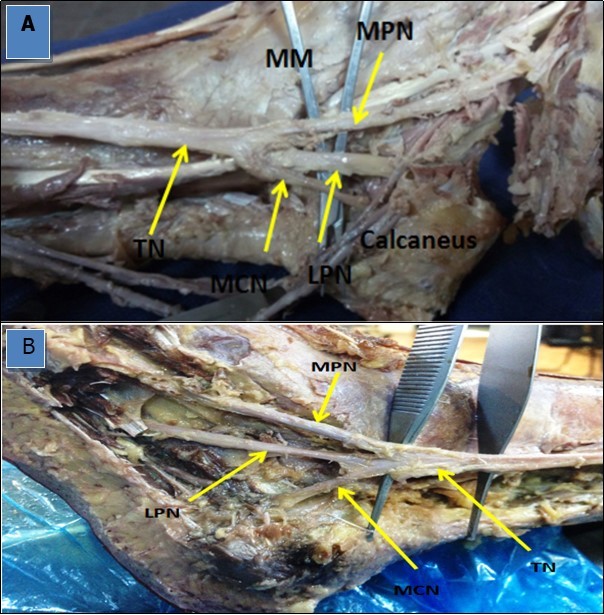
Two branches present in 9 specimens (30%) in right foot. and in 8 specimens (26.7% in the left foot. Figure 4.
Figure 4.Photographs of the ankle region in (A), (B), and (C) showing two medial calcaneal nerves (MCNs)originating from the lateral plantar nerve (LPN).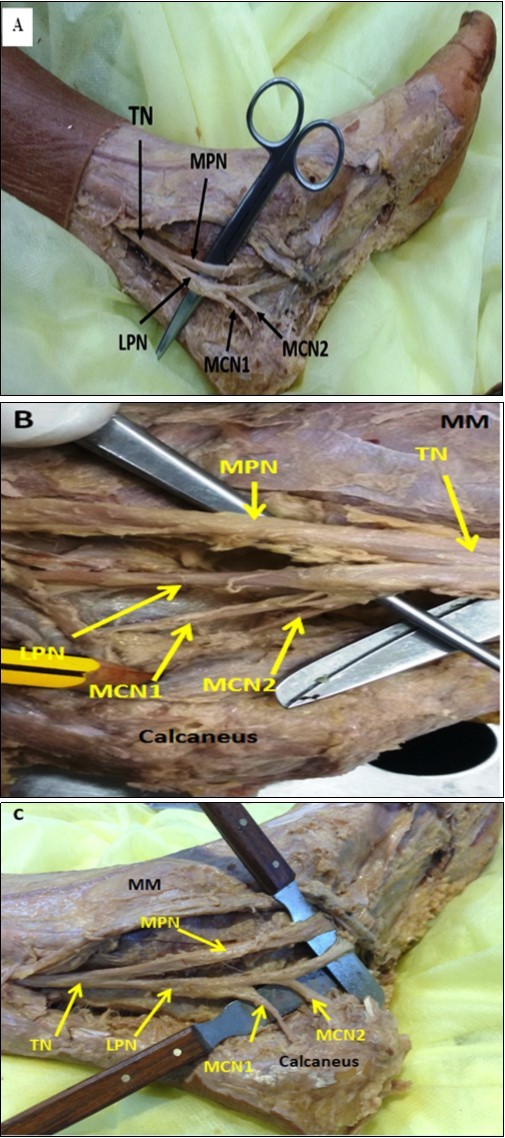
Concerning the level of the MCN origin, in one specimen, a single branch arose from the TN in the popliteal fossa Figure 5 and a single branch emerged from the TN outside the tarsal tunnel just proximal to the malleolar-calcaneal axes Figure 6.
Figure 5.Photograph of the left leg (A) showing one medial calcaneal nerve (MCN) originating from the tibial nerve (TN) high up in the back of the popliteal region.
Figure 6.Photograph of a left leg (B) Showing one medial calcaneal nerve (MCN) originating from the tibial nerve (TN) outside the tarsal tunnel.MM (Medial malleolus) ,MT (Medial tubercle)
The MCN originated from the trunk of the TN in 21specimens (70%) in both feet and from the LPN in 9 specimens (30%) in both feet. No branches were observed to originate from the MPN (Table 1).
Single MCA branches off from PTA observed in 9 specimens (30%) in the right foot and 11 specimens (36.7%) in the left foot. Furthermore, two branches originated from the LPA in 18 specimens (60%) in the right foot and 16 specimens (53.3%) in the left foot. Three branches were present in only three specimens (10%) in both feet, where one originated from the PTA and two from the LPA Figure 7, Figure 8, Figure 9, Figure 10, Figure 11. (Table 2).
Figure 7.Number of medial calcaneal arteries (MCAs).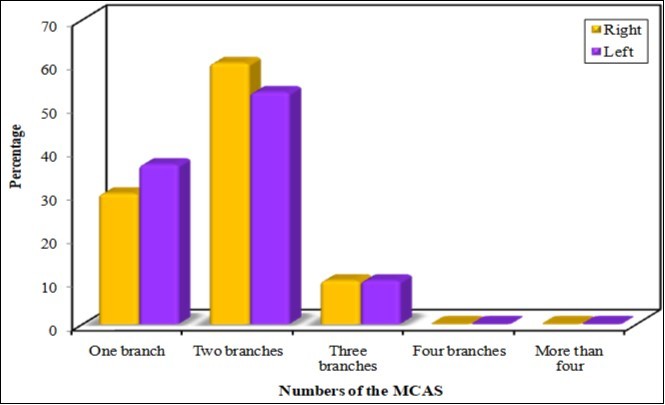
Figure 8.Photograph of the left ankle region showing double medial calcaneal arteries (MCAs) branching from the posterior tibial artery (PTA). MPA: Medial plantar artery, LPA: lateral plantar artery, TN: tibial nerve, MPN: medial plantar nerve.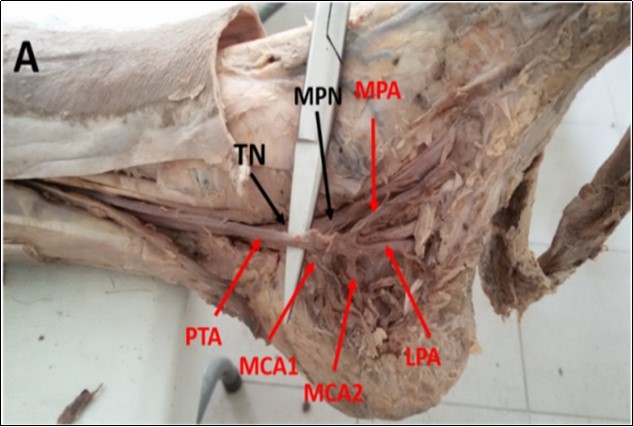
Figure 9.Photograph of the right ankle region (B) showing double medial calcaneal arteries (MCAs) branching from the lateral plantar artery (LPA). PTA: Posterior tibial artery, MPA: medial plantar artery, MM: medial malleolus.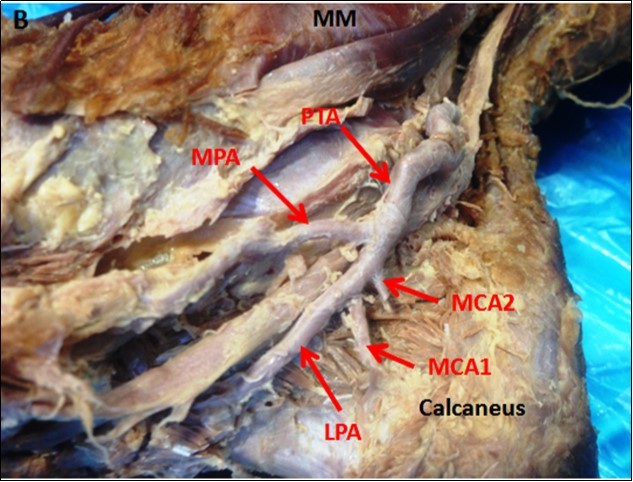
Figure 10.Photograph showing three medial calcaneal arteries (MCAs) branching from the lateral plantar artery (LPA) in a left foot. PTA: Posterior tibial artery, MPA: medial plantar artery.
Figure 11.Photograph of the right ankle region (D) showing a single medial calcaneal artery (MCA) branching from the lateral plantar artery (LPA). PTA: Posterior tibial artery, MPA: medial plantar artery, MM: medial malleolus.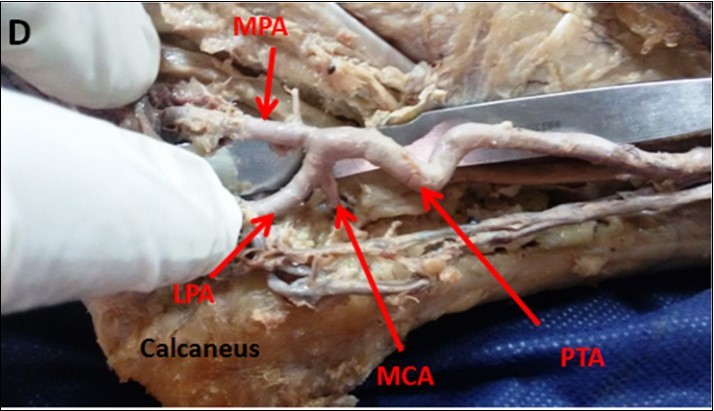
| Numbers of MCAS | Foot | MHx2 | p | |||
| Right (n = 30) | Left (n = 30) | |||||
| No. | % | |||||
| One branch | 9 | 30.0 | 11 | 36.7 | 0.707 | 0.480 |
| Two branches | 18 | 60.0 | 16 | 53.3 | ||
| Three branches | 3 | 10. | 3 | 10.0 | ||
| Four branches | 0 | 0.0 | 0 | 0.0 | ||
| More than four | 0 | 0.0 | 0 | 0. | ||
Discussion
Anatomical studies on the porta pedis and variations of structures passing through it were initiated by Lam and Kick 8 establishing and defining the TN’s compression pathology in the tarsal tunnel. Concerning the branching pattern of the MCN, this study shows variations in both number and origin. In the present study, a single MCN was present in 70% of right feet and 73.3% of left feet. These results nearly match with those of Torres and Ferreira et al 9, who reported a single branch in 56% of specimens, Dellon and Mackinnon et al 10. (75%), Havel et al 11 (79%), and Ndiaye et al 12 80% Furthermore, in this study, two branches were found in 30% and 26.7% in the right and left foot, respectively, in agreement with Moraes et al 13. who reported the existence of two branches in 41.96% of specimens, Fernandes et al 14. 46.66%), Louisia and Masquelet et al. 15 (60%), and Govsa et al 16. (41%). Joshi et al 17.reported four branches, while Fernandes et al 14 reported five branches in some cases. The present study maximum number of MCN is two branches.
As for the origin of the MCN, the present study verified the greater frequency of its origin from the trunk of the TN in 21 specimens (70%) in both right and left feet and from the LPN in 9 specimens (30%) in both feet, in conformity with Joshi et al 17, Moraes et al 13 and Govsa et al 16 except Horwitz 18, who reported 96% origin from the LPN . this discrepancy the author may have confused the MCN with the lower calcaneal branch of the LPN at a more distal level. The origin of the MCN from the MPN presented by Davis and Schon et al 19 .in 15% of cases, as well as Dellon et al 10 (46%) , Havel et al. 11 (5.9%), Govsa et al. 16 (32%), and Moraes et al. 13 (1.22%). However, in this study there was no one arising from the MPN. Another aspect concerning the location of the MCN origin in this study is that the MCN was observed originating inside the tarsal tunnel in all cases except two, in which it originated from the TN high up in the popliteal region (important variant) and the TN just above the Malleolar calcaneal axes outside the porta pedis. The details of the anatomy of the MCN, concerning the variations in the number and origin of the nerve highlighted in this study, has great clinical importance regarding the nerve’s anesthesia, diagnosis, heel pain treatment, and electrode cuff design.
In this study, two MCAS originating from the LPA was the most common frequency in the right foot (60%) and left foot (53.3%). A single branch originating from the PTA was found in 30% of right feet and 36.7% of left feet. Three branches, present in only 10% of both feet, one originated from the PTA and two from the LPA. The results agree with those of Andermahr et al 20, who reported the presence of two branches in 45% in right feet and 47% of left feet and three branches from the PTA in 15% of both feet. These branches supply the calcaneus bone and soft tissue on the medial aspect of the bone. There is a shortage in the data concerning the variations of the branching patterns of the PTA in the porta pedis. Most authors studying the anatomy of the porta pedis concentrated on the branching pattern of the TN. Thus, there is no enough data with which results can be compared. Additional studies on branching pattern of MCA may provide important clinical data that may give clue on blood supply of the ankle region.
Conclusion
From the results of the present study, it could be concluded that there are many variations of the medial calcaneal neurovascular bundle. A single MCN originating from the TN is the most common variant, the level of the nerve branching is highly variable it can branch off from TN at any level from popliteal fossa to the porta pedis. Two MCAs arise from LPA represent the most common presentation.
Recommendations
Clinicians should be aware of the MCN variations when diagnosing and treating conditions related to this nerve, such as tarsal tunnel syndrome, bone fixation at the ankle region, and arthroscopy of the ankle joint. More studies are required to study MCA variations.
Acknowledgments
The author wish to thank Dr: Mohammed Akeel (Head of anatomy department) for his permission to dissect the needed specimens for this paper and Gratitude thank to the donors who give their bodies to enrich medical education and research. The author would like to thank Mr.: Aziz Moazam the lab technician for his assistance in preparing specimens for dissection.
Abbreviations
References
- 1.Standring S. (2008) Gray's Anatomy. The anatomical basis of clinical practice. 40th ed London: Churchill Livingstone. 1425-30.
- 2.Snell R. (2012) Clinical anatomy by regions. 9th ed. , Baltimore, Md: Lippincott Williams 479-481.
- 4.Schon L C, Baxter D E. (1990) Neuropathies of the foot and ankle in athletes. Clinics in Sports Medicine 9(2), 489-509.
- 5.Apaydin N, Loukas M, Kendir S, Tubbs R, Jordan R et al. (2008) precise localization of distal motor branches of the tibial nerve in the deep posterior compartment of the leg.Surgical and Radiologic. , Anatomy 30(4), 291-295.
- 6.Kirkpatrick L A. (2013) Feeney BC.A simple guide to IBM SPSS statistics for version 20.0. Student ed. , Belmont, CA:
- 7.Kotz S, Balakrishnan N, Read C B, Vidakovic B. (2006) Encyclopedia of statistical sciences. 2nd ed. , Hoboken, NJ:
- 9.Torres A L, Ferreira M C. (2012) Study of the anatomy of the tibial nerve and its branches in the distal medial leg. ActaOrtop Bras. 20(3), 157-64.
- 10.Dellon A L, Mackinnon S E. (1984) Tibial nerve branching in the tarsal tunnel. Arch Neurol. 41(6), 645-6.
- 11.Havel P E, Ebraheim N A, Clark S E, Jackson W T, Didio L. (1988) Tibial nerve branching in the tarsal tunnel. Foot Ankle. 9(3), 117-9.
- 12.Ndiaye A, Dia A, Konate I, Diop M, Sow M L. (2003) Topographic anatomy of the tibial nerve in the medial malleolus: Application to the effect of nerve block anesthesia. Morphology. 87(277), 25-7.
- 13.Moraes D C, Carvalho A E, Fialho H S, Galbiatti J A, Carvalho D E. (2007) Nervotibial: variaçõesanatômicas do ramocalcâneo medial. Rev ABTPé. 1(2), 31-40.
- 14.RMP Fernandes, Mozella A, Dias M, Carvalho R, Andrade F et al. (2006) Estudoanatômico do nervotibial no túnel do tarso. Rev Bras de Ortop. 41(7), 272-7.
- 15.Louisia S, Masquelet A C. (1999) The medial and inferior calcaneal nerves: An anatomic study. Surg Radiol Anat. 21(3), 169-73.
- 16.Govsa F, Bilge O, Ozer M A. (2006) Variations in the origin of the medial and inferior calcaneal nerves. Arch Orthop Trauma Surg. 126(1), 6-14.
- 17.Joshi S S, Joshi S D, Athavale S A. (2006) Anatomy of tarsal tunnel and its applied significance. , Journal of the Anatomical Society of India 55(1), 52-6.
- 18.Horwitz M T. (1938) Normal anatomy and variations of the peripheral nerve of the leg and foot: Application in operations for vascular diseases: Study of one hundred specimens. , Arch Surg 36(4), 626-36.
