Abstract
Intrathoracic foreign bodies secondary to penetrating wounds are rare in children. We report the observation of a 10-year-old patient who presented an intrapulmonary metallic foreign body following a playful accident. Its migratory aspect, highlighted by imaging, required urgent extraction which was performed by thoracotomy, with good clinical outcome. The interest of the question lies in the circumstances of the incident, the type of foreign body and the terrain.
Author Contributions
Academic Editor: Raul Isea, Fundación Instituto de Estudios Avanzados -IDEA
Checked for plagiarism: Yes
Review by: Single-blind
Copyright © 2022 Marème Soda Mbaye, et al.
 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Competing interests
The authors have declared that no competing interests exist.
Citation:
Introduction
Intrathoracic foreign bodies are common in children and usually secondary to accidental ingestion or inhalation1,2. Penetrating chest trauma is rarely the cause. Their clinical picture can range from simple pain to severe chest lesions1. Sharp or pointed metallic foreign bodies must be removed urgently as well as if a migratory character is noted2,3. We report a case of retention of an intrapulmonary metallic foreign body in a child, secondary to a neglected penetrating wound, which occurred during a playful accident. On this unusual occasion, the literature is reviewed to make an update in the epidemiological, clinical and therapeutic data.
Observation
AD, aged 10, with no particular pathological history, was referred to us for the management of a post-traumatic intrapulmonary foreign body. The traumatism would have occurred one month earlier, during a playful accident. He would have received from his brother, at the level of the left hemithorax, a blow with the metal tail of a comb. The latter would then have been torn off by the child but without the tail. This would have caused a minimal wound, associated with an intense chest pain, without dyspnea, or cough, justifying local care and treatment with analgesics. The incident was withheld from parents. On admission, there was a punctiform scar in the 2nd left intercostal space, about 5 cm from the sternal border. The pulmonary fields were free. The rest of the exam was normal. The biological results were normal. A first chest x-ray showed a metal rod, oblique downwards, backwards and inwards, going from the 5th to the 11th left costal arch (Figure 1). The computed tomography scan of the chest showed the metal rod in the lung parenchyma. It was approximately 105 mm long and stayed away from the heart and the great vessels. There was no pulmonary parenchymal abnormality, pleural effusion or obvious bone lesion (Figure 2). Two subsequent X-rays showed its migration downwards, inwards and backwards with an upper pole sitting opposite the posterior arch of the 8th rib. A left posterolateral thoracotomy approach allowed the removal of the metal rod lodged in the lower lobe of the lung (Figure 3). The postoperative period was unremarkable. The ablation of the drains was carried out on the5th postoperative day. The patient was discharged on the 8th day. Reviewed in the6th postoperative month, his examination was normal.
Figure 1.A. Frontal chest X-ray showing the foreign body; B: Foreign body sparing the diaphragm on the lateral chest X-ray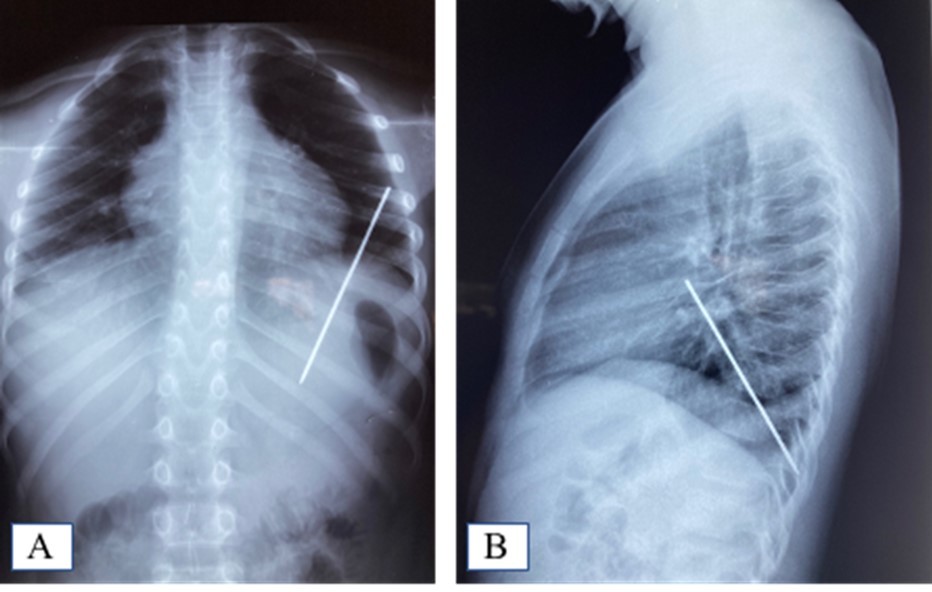
Figure 2.Foreign body in the left lower pulmonary lobe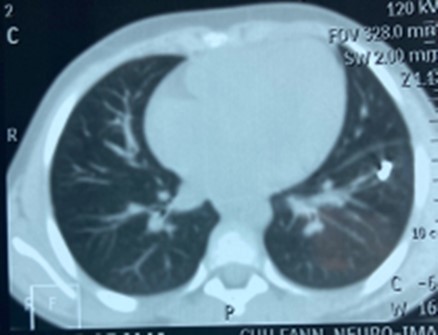
Figure 3.Foreign body visible within left lower pulmonary lobe through posterolateral thoracotomy
Discussion
Intrathoracic foreign bodies are relatively common in children. In an ivorian series, 10% of the children treated in thoracic surgery had an intrabronchial foreign body4. All types of intrathoracic metallic foreign bodies have been reported2. Their causes related to penetrating thoracic traumatism are rare in children. In our patient, the mechanism is all the rarer since it is a penetrating wound that occurred in a child during a playful accident. The classic clinical pictures of a penetrating wound are pleural effusions [5]. Isolated chest pain, linked to an unrecognized foreign body in the chest, as for our patient, is rarely reported1, 6 The diagnosis is usually made on the basis of a well-conducted clinical examination, supplemented by imaging. The interrogation is a capital time and must be extensive, particularly in children. In our case, they concealed the accident. The presence of a scar is valid evidence, but its absence does not rule out the diagnosis. The first-line paraclinical workup is chest X-ray very often supplemented by computed tomography which specifies the exact location of the foreign body and the presence of complications1,6. These can be pericardial tamponade, false aneurysm, aorto-pulmonary fistula, pleural effusion, empyema, mediastinitis. 2, 7 In our patient, no complications were present due in particular to the location of the foreign body. The indications for the removal of an intrathoracic foreign body are manifestations of sepsis, the migratory aspect, signs of lead poisoning, or complications mentioned earlier3. Traditionally, a thoracotomy is performed. Thoracoscopy has also been used. Its advantages include more aesthetic scarring, less post-operative pain and pulmonary complications, shorter recovery time and hospital stay.2, 6 It is reserved for stable patients with benign foreign bodies8. For our patient, we recommended a thoracotomy, given the migratory aspect of the comb tail and the possibility of adhesions linked to the chronicity.
Conclusion
Intrathoracic foreign bodies by penetrating wound are rare in children. Their diagnosis goes through a well-conducted clinical examination, supplemented by imaging. They can occur during play, which calls for more attention in supervising children.
References
- 1.Rabiou S, Ouadnouni Y, Ammor F Z, Belliraj L, Issoufou I et al. (2015) Corps étranger intrathoracique méconnu : cause inhabituelle de douleur thoracique chronique chez l’adulte. Chirurgie Thoracique et Cardio-Vasculaire. 19(4), 239-240.
- 2.Dave N, Oak S N. (2007) Metallic foreign body in the lung: a case report. , J Pediatr Surg 42(7), 1282-3.
- 3.Ndiaye A, Gaye M, Ba P S, Diatta S, Diop M S et al. (2017) Penetrating chest injuries caused by swordfish sword used as a weapon. Asian Cardiovasc Thorac Ann. 25(3), 229-232.
- 4.Kendja F, Demine B, Ouede R, Ehounoud H, Yapo P et al.Chirurgie thoracique pédiatrique à Abidjan. une expérience : à propos de 112 cas. , Ann. Afr. Chir. Thor. Cardiovasc 7(2), 54-8.
- 5.Apiliogullari B, Duzgun N, Kurtipek E, Esme H. (2014) Retained foreign body after chest stab wound. BMJ Case Rep. 2014203598.
- 6.Akkas Y, Yazici U E, Aydin E. (2016) Metallic foreign body migrating to the chest wall. J Case Rep Images Surg. 2, 88-91.
