Author Contributions
Academic Editor: Mona Hassan, Department of Human Anatomy and Embryology, Faculty of Medicine, Suez Canal University, Ismailia, Egypt.
Checked for plagiarism: Yes
Review by: Single-blind
Copyright © 2020 Joseph Bruno Bidin Brooks, et al.
 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Competing interests
The authors have declared that no competing interests exist.
Citation:
Introduction
Behcet's disease (BD) is a multisystem relapsing inflammatory immune-mediated disorder of unknown cause. The Central Nervous System can be affected involving parenchymal and/or vascular topography, such as brainstem, basal ganglia, thalamus, cortex and white matter, spinal cord and cranial nerves.Peripheral nervous system involvement is rare. The neurologic presentations are uncommon, around 10% of historical cases, may present as a primary manifestation or in systemic involvement and more prevalent in younger male patients. Neurobehcet is also associated with abnormalities in complementary exams, like in imaging studies, laboratory and cerebrospinal fluid analysis. 1, 2, 3, 4, 5
Methods
The report of this case was submitted and approved by local ethics committee.
Case Presentation
The present case refers to a 49-year-old caucasian woman admitted to local hospital with a 3-month history of progressive holocranial headache, gait instability and diplopia. Her medical history included recurrent oral and genital ulcers, uveitis and erythema nodosum in both legs. Presence of a pathergy phenomenon and HLA-B51 were confirmed. Hematological and serum biochemistry tests were within normal-range values.
Family medical background was unremarkable. Brain T2-FLAIR magnetic resonance imaging (MRI) showed an expansive mass lesion at the left capsular nucleus region, with mesencephalic extension (Figure 1A). Cerebrospinal fluid analyses showed 15 cells, all of them lympho-monocytes, and protein of 45mg/dL (lumbar puncture). All other tests on spinal fluid were normal.
The patient was also referred to a neurosurgery department, where a brain biopsy was planned for diagnostic clarification. Meanwhile, the possible clinical diagnosis of BD was postulated and started treatment with 1 gram of methylprednisolone intravenously and for a period of 5 days with satisfactory results. Neurosurgery was then discarded. Therapeutic follow-up was instituted with azathioprine and after 2 months of treatment, due to abnormal liver function, anti-TNF-alpha (Infliximab) was was administered at 0, 2nd and 6th weeks and then every eight weeks; Despite cerebral atrophy, stable neurological evolution was found after 18 months of anti-TNF-alpha therapy (Figure 1B).
Figure 1.Brain Axial-FLAIR-MRI- (A) Expansive mass lesion with hyperintense signal in the left capsular nucleus region, with mesencephalic extension and enhancement by the paramagnetic agent (white arrows). (B) Complete improvement of the expansive mass lesion with the presence of brain atrophy.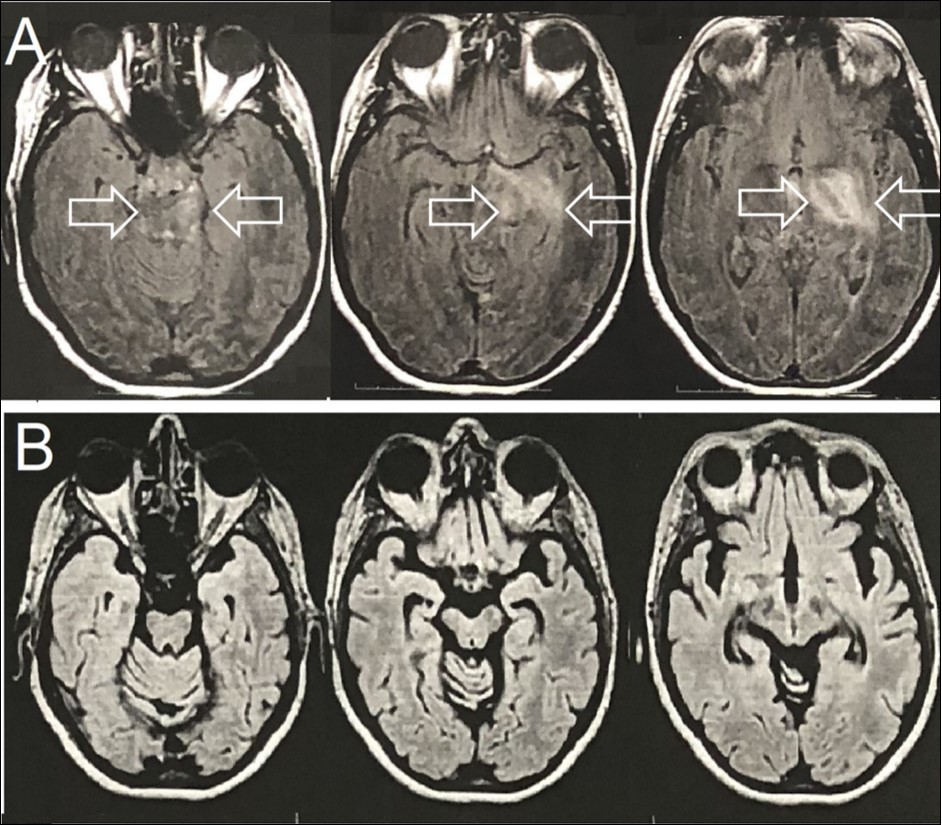
Discussion
Neurological involvement occurs in approximately 10% of BD patients and is characterized by an interval of 5 years since the onset of systemic and the neurological symptoms. Clinical and neuroimaging findings suggest parenchymal and extra-parenchymal inflammatory involvement. Pseudotumoral lesion of the Central Nervous System demonstrates inflammatory activity; Brain atrophy can coexist since the beginning of the inflammatory course and demonstrates neurodegeneration. 6 We reported a patient with BD associated with a pseudotumoral lesion of the Central Nervous System, a rare neurological involvement. The patient presented adverse effect to conventional immunosuppressive treatment, with azathioprine and had sustained clinical response with infliximab.
The present case highlights the difficulties in diagnosing BD, which may leave incorrect diagnosis and therapeutic delay.
References
- 1.H U Behcet. (1937) ber residivierende, aphto¨se durch ein Virus verursachtes Geschwu¨re am Mund, am Auge und an der Genitalien. Derm Wschr;. 105, 1152-1157.
- 2. (1990) International StudyGroup for BehcetsDisease. Criteria for diagnosis of Behcets disease. Lancet;335: 1078-1080.
- 3.Akman-Demir G, Serdaroglu P, Tasci B. (1999) Clinical patterns of neurological involvement in Behcets disease: evaluation of 200 patients. , The Neuro-Behcet Study Group. Brain; 122, 2171-2182.
- 4.Borhani-Haghighi A, Kardeh B, Banerjee S, Yadollahikhales G. (2019) Neuro-Behcet's disease: An update on diagnosis, differential diagnoses, and treatment. Mult Scler Relat Disord;. 23(39), 101906.
