Abstract
Purpose
The purpose of this study was to assess the efficacy (overall survival, local control, progression free survival (PFS) and toxicities between two dimension (2D) and three dimension (3D) CT guided brachytherapy without using interstitial needles in cervical cancer patients.
Material and Methods
A retrospective case-control study was performed in Figo stage IB-IVA cervical cancer patients treated between March 1990 and August 2018. Concurrent chemoradiation using external beam radiotherapy followed by brachytherapy (BT) was the treatment method used in all patients. Clinical endpoints were overall survival, local control, progression free survival, acute toxicities and late toxicities.
Results
A 102 cervical cancer patients were included,52 patients have been treated with 2D and 50 patients with 3D using CT scan brachytherapy without interstitial needles. Baseline characteristics were similar between both groups. External beam was used in all patients during concurrent chemoradiation period before brachytherapy. All patients completed the treatment. Similar 3-year overall survival and local control was reported between 2D and 3D techniques. Overall 3-year survival rate was 95.7% in 2D and 91.8% in 3D brachytherapy (P value = 0.188). Local control at the 3 year follow up was 88.6% in 2D and 93.3% in 3D (P value = 0.571). Progression free survival was better in 2D rather than 3D (86.13% in 2D vs 27.4% in 3D, p value = 0.006). No grade 3 or 4 toxicity in 3D technique was observed whereas there are 1.9% of grade 3 acute GI toxicity and grade 3 late GI and GU toxicities in 2D technique (7.7% and 5.8 %). The 3D brachytherapy significantly reduced acute grade 2-3 GI side effect and grade 2-3 late GU side effect (acute GI 25% in 2D vs 4% in 3D, late GU (56% in 2D vs 16% in 3D).
Conclusion
Using CT guided 3D brachytherapy in treatment of cervical cancer showed similar outcomes in survival and local control but reduced toxicity compared to the 2D technique. Disease progression including metastasis was found better in the 2D brachytherapy technique. CT guided brachytherapy helped reduce dose to organs at risk and long term follow up for survival outcome and toxicities was needed.
Author Contributions
Academic Editor: Sasho Stoleski, Institute of Occupational Health of R. Macedonia, WHO CC and Ga2len CC, Macedonia.
Checked for plagiarism: Yes
Review by: Single-blind
Copyright © 2020 Pitchaya Sakyanun
 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Competing interests
The authors have declared that no competing interests exist.
Citation:
Purpose
Cervical cancer was one of the most common female cancers especially in low- and middle- income countries. The treatment modalities included surgery, radiation therapy and systemic therapy depending on disease status (staging, histopathologic etc.), patient status (performance status, age etc.). Concurrent chemoradiation followed by brachytherapy was considered to be standard treatment of locally advanced cervical cancer stage IB2-IVA in Figo staging 2008 or IB3, IIA2 -IVA in Figo staging 2018 1, 2, 3, 4.
Boosting via brachytherapy was able to escalate high dose to control the cervical mass without increasing pelvic toxicities. Brachytherapy technique has evolved over time from using plain film imaging (2D technique) to using CT scan or MRI scan (3D technique).
In the 2D technique, the dose was prescribed to a virtual point A, fixed distance from the applicator. Pear shaped isodose configuration was done in this conventional brachytherapy. Rectal and bladder point dose was measured related to applicator location so the nearby organ dose measurement might be inexact 5.
In the 3D technique, using CT or MRI scan, cervical mass and nearby organs were obviously better seen than with plain film. Dose prescription was given to high risk target volume (HR CTV). Volume based measurement was reported of target dose and nearby normal organ. Interstitial needles may be added to brachytherapy applicators 6.
Nowadays, in many centers 3D techniques are used instead of the 2D brachytherapy which consumes much more resources. The aim of this study was to evaluate the different outcomes between the 2D and 3D brachytherapy without interstitial needles outcomes on overall survival(OS), progression free survival(PFS), local control(LC) and toxicities in locally advanced cervical cancer patients after treated with concurrent chemoradiation.
Material and Methods
Patient Selection
This retrospective cohort study included cervical cancer patients stage IB2-IVA in figo staging 2008 or IB3, IIA2-IVA in figo staging 2018. These patients were all treated with concurrent chemoradiation to pelvis (+/- paraaortic lymph nodes) followed by brachytherapy(low dose rate (LDR) and high dose rate(HDR)) between March 1990 and August 2018. Every cervical patient had to complete radiation therapy and chemotherapy sessions. All patients were Biopsy-proven to have cervical cancer, including: squamous cell carcinoma, adenosquamous cell carcinoma or adenocarcinoma. All patients were treated with conventional EBRT technique.
Study Design
Patients were divided into two groups based on imaging type during brachytherapy, 2D or 3D technique brachytherapy data. Brachytherapy treatment was done with plain film in the 2D technique and CT scan in the 3D technique. The brachytherapy applicators were all without interstitial needles. Patient characteristics, cancer characteristics, cancer staging, treatments, outcomes and complications of treatment were collected retrospectively. This study was approved by the Phramongkutklao Hospital Ethics Committee.
Treatment Characteristics
Locally advanced cervical cancer stage IB2-IV in figo staging 2008 or IB3, IIA2 -IVA in figo staging 2018 was diagnosed based on physical examination and imaging data. Whole pelvic external beam radiation therapy was used concurrent with chemotherapy. Four field techniques with 45-50 Gray in 25 fractions and 10 MV photons were prescribed. After external beam radiation, high dose rate brachytherapy was performed once weekly. Radioactive use in low dose rate brachytherapy was cesium-137 during 1990-2006 and high dose rate Iridium-192 during 2007-2018.Almost all patients received platinum based chemotherapy such as Cisplatin and Carboplatin. The minority received Fluorouracil(FU) and Mitomycin. Radiation and chemotherapy were all completed followed by standard treatments. All patients had to complete the total treatment time within 8 weeks.
External Beam Radiation Therapy ( Whole Pelvis)
The whole pelvic radiation therapy was all used with four field conventional techniques. 10 MV photon was prescribed. Radiation dose was between 45-50 Gy. Field design for pelvic radiation therapy was AP-PA and lateral fields.
AP-PA field borders were defined as
Superior at L4-L5 vertebral interspace
Inferior at 2 cm below the obturator foramen or 3 cm inferior to distal disease, whichever is lower.
lateral at 1.5-2 cm alteral to the pelvic brim.
Lateral field borders were defined as
Superior at same as AP-PA field
Inferior at same as AP-PA field
Anterior at anterior to pubic symphysis
Posterior at 0.5 cm posterior to the anterior border of the S2/3 vertebral junction, may include the entire sacrum to cover the disease extent
If paraaortic LN field was added, the field would be up to T12-L1 interphase.
Concurrent Chemotherapy Details
Almost all patients received platinum based chemotherapy such as 40mg/m2 of Cisplatin weekly (N=92, 90%) or 100 mg/m2 of Carboplatin Auc 2 weekly (N=7, 6.86%). The minority received 1000 mg/m2/ Fluorouracil(FU) a day on days 1-4 and 29-32 and 10 mg/m2 of Mitomycin a day on day 1 and day 29 (N=3, 2.94%).
Brachytherapy Specifications
High dose rate brachytherapy using tandem and ovoids application without interstitial needles was used in both 2D and 3D techniques.
In the 2D technique, plain film of the lower abdomen was done after application insertion. According to ICRU 385, dose prescription was set 100% at point A. Dose fractionation such as 6.5Gy x 4 times,7.5 Gy x 3 times and 8.3 x 2 times was prescribed. Normal organ dose constraint was described as bladder and rectal point from plain film.
In the 3D technique, a CT scan without contrast media was done followed by applicators insertion. Pre-brachytherapy MRI scan was done in every case since 2017 to evaluate the disease extension. According to GEC-ESTRO guidelines 4, target volume, High risk clinical target volume (HR-CTV) and intermediate target volume (IR-CTV) were used in dose prescription instead of point A. HR-CTV was covered the gross tumor at the time of brachytherapy determined by both pre-brachytherapy MRI image and at the exam, the entire cervix and regions of indeterminate T2- weighted MRI signal and the gray zone. IR-CTV was determined of HR-CTV with an asymmetric expansion, not extending into OARs and including sites of initial involvement.
Dose distribution depended on the standard loading system of tandem and ovoids. Organs at risk (OAR) such as rectal and bladder radiation dose was measured using D2cc (minimal dose to the most irradiated 2 cc of OAR). A target dose volume histogram was used for dose to 90% and 95% of the target volume. The total dose was calculated including external beam radiation dose and brachytherapy dose using tumor equivalent dose (EQD210) and OAR equivalent dose (EQD2 3). Dose fractionation such as 6.5Gy x 4 times,7.5 Gy x 3 times and 8.3 x 2 times was prescribed.
Low dose rate brachytherapy delivers radiation at a dose of LDR brachytherapy at 0.55–0.65 Gy/h. Point A doses were 75 Gy in two fractions for LDR. Patients who received the intrauterine tandem and ovoids were hospitalized after placement of the applicator for 24–72 hours to allow radiation therapy treatment. Cs-137 low dose rate radioactive source was applied for intracavitary brachytherapy treatment has been determined using the Manchester System from 1990 to 2006.
High dose rate brachytherapy delivered a dose >12 Gy/hour and was in the outpatient setting. Short duration of brachytherapy treatment time, patient convenience were the advantages over low dose rate brachytherapy. 192 Ir HDR sources were used in high dose rate brachytherapy from 2007 to 2019.
At our institute, brachytherapy treatment planning system (Varian Medical Systems, Inc., Palo Alto, CA) has been used. The optimization process was equal times, geometric optimization (GO) and volume optimization (VO). In 3D brachytherapy, contouring of target volume and normal organs at risk were input. The GO was performed followed by isodose reshaping by manual adjustments of isodose lines. Adjusting the isodose lines was done to optimize between target volume dose and critical structures dose.
Endpoints
The primary endpoint of this retrospective cohort was overall survival, defined as from the first date of treatment to death from any cause. The secondary endpoints were local control (defined as absence of the local disease evidenced from physical examination, Imaging and biopsy (if performed), progression free survival (defined as no evidence of disease at any site of the body from physical examination, imaging or biopsy (If performed) , acute toxicities at least grade 2(defined toxicities during radiation therapy session to 3 months after radiation therapy and late toxicities at least grade 2 (defined toxicities more than 3 months after radiation therapy).Minimal follow-up required at least 2 years.
Statistics
Patient and disease characteristics were described with percentage, mean and standard deviation with differences using a chi-square test. Overall survival, local control and progression free survival were all calculated from the date of treatment to the date of events or loss follow up. Kaplan-Meier survival method and log rank test were used to calculate the time to event. Acute and late toxicities were measured using chi-square tests. P-values of less than 0.05 were defined significantly. Analysis using SPSS version 21.0 was performed.
Results
Patient and Treatment Characteristics
All 102 cervical cancer patients were retrospectively registered in this study. All patients completed the standard treatment (concurrent chemoradiation and brachytherapy). Of the total patients, the 2D technique was used on 52 patients and the 3D technique was used on the other 50 patients. All patients used high dose rate brachytherapy without interstitial needles insertion (Table 1). Patient characteristics (Figo staging, pathology, underlying disease and age at diagnosis) were described and compared between 2D and 3D techniques. All patient characteristics had no statistical significant difference between 2D and 3D technique (P value < 0.05) (Table 1).
Table 1. Baseline characteristics| Total (n=102) | Technique 2D (n=52) | Technique 3D (n=50) | p-value | |
| n (%) I Mean ± SD(Min- Max) | n (/o) I Mean ± SD(Min—Max) | n (%) I Mean ± SD (Min - Max) | ||
| stage Figo | 0.231 | |||
| stage 1-2 | 53 (51.96) | 24 (46.15) | 29 (58.00) | |
| stage 3-4 | 49 (48.04) | 28 (53.85) | 21 (42.00) | |
| Patho | 0.885t | |||
| Adenoca | 13 (12.75) | 7 (13.46) | 6 (12.00) | |
| Adenosquamous | 1 (0.98) | - | 1 (2.00) | |
| Scca | 88 (86.27) | 45 (86.54) | 43 (86.00) | |
| DM | 1.000t | |||
| No | 96 (94.12) | 49 (94.23) | 47 (94.00) | |
| Yes | 6 (5.88) | 3 (5.77) | 3 (6.00) | |
| HT | 0.127 | |||
| No | 91 (89.22) | 44 (84.62) | 47 (94.00) | |
| Yes | 11 (10.78) | 8 (15.38) | 3 (6.00) | |
| DLP | 0.495t | |||
| No | 100 (98.04) | 50 (96.15) | 50 (100.00) | |
| Yes | 2 (1.96) | 2 (3.85) | - | |
| CKD | 1.000t | |||
| No | 101 (99.02) | 51 (98.08) | 50 (100.00) | |
| Yes | 1 (0.98) | 1 (1.92) | - | |
| HIV | 0.0541 | |||
| No | 98 (96.08) | 52 (100.00) | 46 (92.00) | |
| Yes | 4 (3.92) | - | 4 (8.00) | |
| MDS | 1.000t | |||
| No | 101 (99.02) | 51 (98.08) | 50 (100.00) | |
| Yes | 1 (0.98) | 1 (1.92) | - | |
| Age at diag (year) | 51.3± 11.61 (26- 87) | 52.35± 11.26 (28- 87) | 50.22± 11.98 (26- 72) | 0.358$ |
| Age group | 0.139 | |||
| <=40 | 15 (14.71) | 5 (9.62) | 10 (20.00) | |
| >40 | 87 (85.29) | 47 (90.38) | 40 (80.00) |
Outcomes
The follow up time in the 2D technique was a range of 6-30 years and the 3D was 3-5 years. Loss follow up was measured in 13.7% of all populations (14 of 102 patients).
Overall Survival
96 of the 102 patients were alive at the time of analysis. The overall survival rate was 96% at the 3-year follow-up. 2 patients (1.96%) died from cervical cancer while 4 patients (3.9%) died from other conditions such as UTI septicemia, or other underlying disease conditions.
The overall survival rate of the 2D technique was 95.65 % (83.58 - 98.90) and 3D technique was 91.79 (79.57 - 96.84) without statistical significant difference (Figure 1).
Figure 1.Kaplan-Meier survival estimates for overall survival rate (OS) between 2D technique conventional brachytherapy (blue line) and 3D technique Image guided brachytherapy using CT simulation ( red line) showed no statistical significant difference.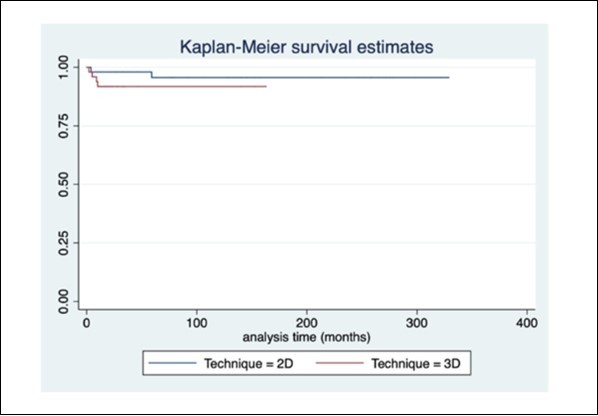
Local Control
94 of the 102 patients achieved the 3-year local control. Local recurrence was observed in 8 patients. Overall local control was 92.16 % at the 3-year mark. Between the 2D and the 3D technique, there was no difference of 3 year local control rate (2D - 88.59% (74.53 - 95.13) and 3D - 93.33% (80.67 - 97.81) (P value = 0.571). (Figure 2)
Figure 2.Kaplan-Meier survival estimates for local control rate (LC) between 2D technique conventional brachytherapy (blue line) and 3D technique Image guided brachytherapy using CT simulation ( red line) showed no statistical significant difference.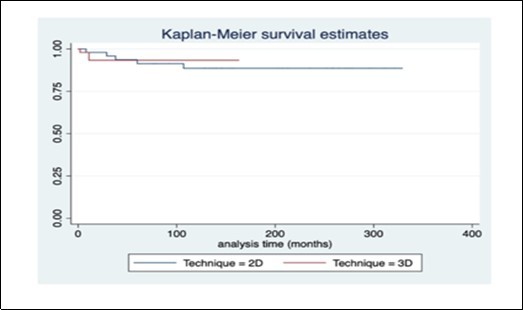
Progression Free Survival
Overall progression free survival was 85.29% (87 of the 102 patients). The 3-year progression free survival rate was 86.13% in 2D and 27.14% in 3D ( P value =0.006). In this analysis, 2D technique seemed to have better progression free survival than 3D technique (Figure 3).
Figure 3.Kaplan-Meier survival estimates for three-year progression free survival (PFS) between 2D technique conventional brachytherapy (blue line) and 3D technique Image guided brachytherapy using CT simulation (red line) show better outcome in 2D technique compared to 3D technique.
Toxicities
Acute Toxicities
Acutegrade 2-3 hematologic, genitourinary and skin toxicity were comparable between the 2D and the 3D technique but gastrointestinal toxicity was significantly better in the 3D technique (4% in 3D vs 25 % in 2D, P value = 0.003).
There was 1 patient (1.9%) using the 2D technique who suffered from grade3 GI toxicity but without grade 3 or 4 in the 3D technique.
Late Toxcities
There were no differences in grade 2-3 late toxicities between the 2 techniques in hematologic, gastrointestinal and skin toxicities. 4 patients (7.7%) suffering from grade 3 gastrointestinal toxicities and 3 patients (5.77 %) suffering from genitourinary toxicities were observed in the 2D technique. No late grade 3 or 4 toxicity was detected in the 3D technique. Furthermore grade 2-3 genitourinary toxicities were significantly better using the 3D brachytherapy technique (16% in 3D vs 55.77% in 2D, P value < 0.001) such as severe radiation cystitis, urinary obstruction or hydronephrosis. (Table 2).
Table 2. showed grade 2-3 acute and late toxicities between 2D conventional brachytherapy and 3D technique Image guided brachytherapy using CT simulation.| Acute | 2D | 3D | P value | ||
| grade 1-2 | grade 3 | grade 1-2 | grade 3 | ||
| hemato | 0.495t | ||||
| No | 50 (96.15) | - | 50(100.00) | - | |
| Yes | 2 (3.85) | - | - | - | |
| Gi | 0.003 | ||||
| No | 39 (75.00) | 48 (96) | - | ||
| Yes | 12 (23.08) | 1 (1.92) | 2 (4.00) | - | |
| GU | 0.1181- | ||||
| No | 48 (92.31) | - | 50(100.00) | - | |
| Yes | 4 (7.69) | - | - | - | |
| skin | 0.243t | ||||
| No | 49 (94.23) | - | 50(100.00) | - | |
| Yes | 3 (5.77) | - | - | ||
| Late | 2D | 3D | P-value | ||
| grade 1-2 | grade 3 | grade 1-2 | grade 3 | ||
| hemato | NA | ||||
| No | 52 (100.00) | - | 50(100.00) | - | |
| Yes | - | - | - | ||
| Gi | 0.479 | ||||
| No | 42 (80.77) | 43 (86.00) | - | ||
| Yes | 6 (11.53) | 4 (7.7) | 7 (14.00) | - | |
| GU | <0.001 | ||||
| No | 23 (44.23) | 42 (84.00) | - | ||
| Yes | 26 (50.00) | 3 (5.77) | 8 (16.00) | - | |
| skin | 0.495t | ||||
| No | 50 (96.15) | - | 50(100.00) | - | |
| Yes | 2 (3.85) | - | - | - | |
Discussion
This study compared the 2 techniques of brachytherapy (2D vs 3D) in terms of the efficacy and toxicities in locally advanced cervical cancer patients with definite concurrent chemoradiation. The tandem and ovoids without interstitial needles were used in all patients. Image guided brachytherapy using CT scan was applied in all 3D technique cases.
The overall results of this study were comparable with other IGRT brachytherapy studies of other centers in aspects of overall survival, local control and toxicities.
Overall Survival
The overall survival was 96 % at the 3-year follow-up comparable with other data from previous studies which range from 68% to 94 %. Between the 2D and the 3D techniques, there seemed to be no overall difference in the survival rate (range from 79.6 to 98.9 %). Completion of concurrent chemoradiation with acceptable overall treatment time in all patients in this study might relate to a good outcome of overall survival. Death from non-cancer causes were twice as much as cancer causes as referred to in the standard treatment of cervical cancer.
Local Control
Overall local control was 92.16 % for 3 years. Between the 2D and the 3D techniques, there was no difference of the 3-year local control rate (2D - 88.59% (74.53 - 95.13) and 3D - 93.33% (80.67 - 97.81). Other studies showed a 3-year local control range from 78.5 - 97.9 % which were comparable to our study. Compared to other interstitial needles using brachytherapy studies, no difference in outcome was seen in local control rate. Ongoing results from prospective studies using MRI and interstitial needles brachytherapy are still being waited for.
Progression Free Survival
Surprisingly, progression free survival (PFS) of the 2D technique from this retrospective study was statistically better than the 3D technique (86.13% vs 27.4 %, P value= 0.006). Because of low event rate and low sample sizes from this retrospective study, the PFS might not represent the exact survival. Using the 2D brachytherapy technique also showed excellent results in progression free survival.
Toxicities
The 3D brachytherapy technique showed significant reduction of acute and late grade-3 toxicities compare to 2D technique (acute gastrointestinal toxicities, 2D 1.92 % vs 3D 0%), (Late gastrointestinal toxicities 2D 7.7% vs 3D 0%, genitourinary toxicities 2D - 5.77% vs 3D - 0%). Moreover, reduction of acute grade 1-2 gastrointestinal toxicities and late genitourinary toxicities were statistically observed in 3D technique compared to 2D (acute 4% in 3D vs 23.08 % in 2D, late 16% in 3D vs 50 % in 2D).
Compared to the study from the Netherlands 7, which compared between 2D and 3D techniques. The difference between the studies was that some patients of the Netherland study used interstitial brachytherapy and some patients underwent MRI rather than CT scan in image guided radiation therapy. Although, the results were almost similar to our studies in aspects of overall survival, local control and toxicities.
RetroEMBRACE study 8 was the image guided brachytherapy study included IA-IVB cervical cancer patients. Using definitive EBRT +/- concurrent chemotherapy followed by IGBT was all used. The 3/5-year local control, pelvic control, cancer specific survival, overall survival were 91%/89%, 87%/84%, 79%/73%, 74%/65%.
According to the oncologic results, local control was similar to our study. Our study showed better survival which may be from including only completing definitive CCRT and IGBT patients. In Retro EMBRACE, IGBT consisted of using CT or MRI scan which resulted in 5-year G3–G5 morbidity was 5%, 7%, 5% for bladder, gastrointestinal tract, vagina. In comparison, 3D based brachytherapy in our study used pre-brachytherapy MRI scan which might help identify the exact volume of HR-CTV and IR-CTV and reduce the toxicities but longer follow up time are needed in our study’s 3D technique.
The 2D technique represented good results in overall survival, local control and progression free survival but had more toxicities compared to the 3D brachytherapy technique. Acute and late toxicities might be related to the destruction of contemporary or permanent quality of life. Some patients had disease free conditions but may suffer for the rest of their lifetime from the side effects.
However, our results should be interpreted with caution because of the retrospective manner and shorter follow up time of the 3D technique, compared to the 2D technique. While figo staging was different between the era of the 2D and the 3D techniques which have some variations on the cancer evaluation such as imaging modalities, staging. Low event rate was the limitation of the survival and local control comparison between the 2D and the 3D technique. A larger number of patients and a longer follow up time were needed to investigate the 2 techniques. Further ongoing multicenter randomized EMBRACE II study which uses the most advanced techniques is being used to further exploit the results.
Conclusions
In locally advanced cervical cancer patients treated by concurrent chemoradiation followed by brachytherapy, the three-year overall survival and local control were similar between the 2D and the 3D technique while the 2D improved progression free survival. The 3D brachytherapy technique showed significant reduction in both acute and late toxicities. Because of the retrospective manner and small population of this study, this is the subject of ongoing prospective EMBRACE II study.
Contribution
Pitchaya Sakyanun contributed to overall data collection, management of the program, data analysis, writing the manuscript and management of the study (100%)
Acknowledgements
This study was approved and funded by Phramongkutklao College of medicine and Phramongkutklao Hospital.
References
- 1.Whitney C W, Sause W, Bundy B N. (1999) Randomized compari- son of fluorouracil plus cisplatin versus hydroxyurea as an adjunct to radiation therapy in stage llB-IVA carcinoma of the cervix with negative para-aortic lymph nodes: A Gynecologic Oncology Group and Southwest Oncology Group study. , J Clin Oncol 17, 1339-1348.
- 2.Morris M, Eifel P J, Lu J. (1999) Pelvic radiation with concurrent chemo- therapy compared with pelvic and para-aortic radiation for high-risk cervical cancer. , N Engl J Med.;3 40, 1137-1143.
- 3.Rose P G, Bundy B N, Watkins E B. (1999) Concurrent cisplatin-based radiotherapy and chemotherapy for locally advanced cervical cancer. , N Engl J Med 340, 1144-1153.
- 4.Keys H M, Bundy B N, Stehman F B. (1999) Cisplatin, radiation, and adjuvant hysterectomy compared with radiation and adjuvant hysterectomy for bulky stage IB cervical carcinoma. , N Engl J Med 340, 1154-1161.
- 5. (1985) International Commission on Radiation Units and Measurements (ICRU) Report 38. Dose and volume specification for reporting intracavitary brachytherapy in gynecology.
- 6.Potter R, Haie-Meder C, E Van Limbergen. (2006) Recommendations from gynaecological (GYN) GEC ESTRO working group (II): Concepts and terms in 3D image-based treatment planning in cervix cancer brachytherapy – 3D dose volume parameters and aspects of 3D image-based anatomy, radiation physics, radiobiology. , Radiother Oncol 78, 67-77.
