Abstract
Background
Traumatic brain injury in pediatrics is one of the commonest causes of morbidity, disability and mortality worldwide. In low- and middle-income countries Study showed that death of pediatrics from traumatic brain injury was 7.3%. However, there is limited data towards the outcome of traumatic brain injury and its associated factors in Ethiopia.
Objective
To assess the outcome of traumatic brain injury and associated factors among pediatrics patients in Amhara National Regional State Comprehensive Specialized Hospitals, Ethiopia.
Methods
An institution based retrospective cross-sectional study was conducted among 423 pediatrics patients from January 1, 2019 to December 30, 2021, and data extraction period was from May 16 to June15, 2022. Systematic random sampling technique was employed to select the study participants. Data were collected from patient charts and registry books by using a data extraction tool. Data were entered into the Epi-info version 7 and analysis was done by SPSS Version 25. Both Bi-variable and multi-variable analyses were employed to identify factors associated with outcome of traumatic brain injury.
Result
From 423 sampled study participant charts 404 of them had complete information with response rate of 95.5% and included in the final analysis. The overall unfavorable outcome of traumatic brain injury at discharge was found that 12.13% (95% CI: 9.1% - 15.7 %). Sever traumatic brain injury (AOR: 5.11(CI :1.8-14.48), moderate traumatic brain injury (AOR:2.44(CI:1.07-5.58), Hyperglycemia (AOR: 3.01 (CI:1.1-8.04), sign of increased intracranial pressure (AOR:7.4(CI:3.5-15.26), and medical comorbidity (AOR: 2.65(CI:1.19-5.91) were predicted of unfavorable outcome of traumatic brain injury pediatrics patient.
Conclusion and recommendations
twelve present of traumatic brain injury results unfavorable outcome. Sever and moderate form of traumatic brain injury, hyperglycemia, signs of increased intracranial pressure, and medical comorbidity were factors associated with unfavorable outcome of traumatic brain injury in children. Therefore, it is preferable to improve accesses to acute and post-acute care services to lower the unfavorable outcome of traumatic brain injury in children.
Author Contributions
Academic Editor: Gabriele Ronchetti, Neurosurgery at ASL Città di Torino
Checked for plagiarism: Yes
Review by: Single-blind
Copyright © 2023 Aytenew Getabalew, et al.
 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Competing interests
The authors have declared that no competing interests exist.
Citation:
Introduction
Traumatic brain injury is physical insult that happen once the brain is exposed to an excessive external force and the common clinical presentation after trauma is confusion, loss of consciousness, coma and seizure.1
Traumatic brain injury is more common in children. There are a variety of contributing factors that make children more vulnerable to TBI, including the size of their of head is larger than their body weight and other physiologic aspects 2. Fall from a height, road traffic accidents, and direct head trauma are the most prevalent causes of traumatic brain injury in children 3.
Previous study showed that worldwide prevalence and incidence of Traumatic brain injury in children is continuing to be a serious community health concern, with 47 to 280 traumatic brain injury cases per hundred thousand children.4
In USA, study showed that yearly 99,796 of children were die due to traumatic brain injury .5 As well as Study conducted in resource limited Low- and Middle-Income countries reveled that mortality among traumatic brain injury of children was 7.3% 6
Previous study in African study found that high burden of deaths due to trauma-related brain injury among children. According to those study, traumatic brain injury caused 41.8 %, 18.75 %, and 8% of deaths in Egypt, South Africa, and Sub-Saharan Africa, respectively. 3, 7, 8
In Ethiopia study suggest that trauma is one of major public health challenge and the most prevalent contributing reasons include RTAs, falls, and animal-related injuries, however there is scarcity of data towards outcome of TBI and associated factors in children. 9, 10
Different study shows that unfavorable outcome of traumatic brain injury in children is still higher and one of the major community heath challenges in worldwide. Such as, study conducted in Europe 10 % , Netherlands 5%, Germany 27.6% and in Singapore 30% .11, 12, 13, 14
A study conducted in India found that 10.6% of children who suffer traumatic brain injuries have unfavorable outcomes. 15 And other similar study done in China 12.6% death among all TBI and in Pakistan among decompressive craniotomy of severe TBI 36 % of children results unfavorable outcome of traumatic brain injury of children. 16, 17
Study conducted in Qatar National Trauma Center showed that 13% and Saudi Arabia 14.8% children was reported that unfavorable outcome from TBI. 18, 19
In resource limited setting of low- and middle-income country different study revealed that death of children’s from TBI are still high such as study done in south Africa 18.75% , in Togo at Sylvanus Olympio University Hospital 31.9 % , in Uganda 35% and in Egypt at Cairo University Hospitals 41.7% of TBI in children. 3, 7, 20, 21
Study conducted in Sub-Saharan Africa showed that the overall mortality from traumatic brain injury of children was report that 8% and other cross-sectional study done in age of under 14 children in south Ethiopia Hawassa University Compressive Specialized Hospital revealed that 15.8% of TBI children results unfavorable outcome .8, 10
According to WHO and other similar worldwide study revealed that age of less than four and male children was associated with unfavorable outcome pediatric TBI in children. 4, 22 Other study conducted by Centers for Disease Control and Prevention showed that rural residence is significantly higher in hospitalization and death among TBI children .23
Study done in France revealed that educational level of children and parental education level significantly associated with outcome of TBI. 24 However, study done on under age of 14 in Ethiopia Hawassa University Hospital showed parental education level were not associated with outcome of TBI of children. 10
Different Study revealed that RTA the most common Mechanism of traumatic brain injury of pediatrics traumatic brain injury such as, study in German , Sub-Saharan Africa and Ethiopia .8, 10, 25, 26.However ,study conducted in USA ,in Netherland , Hong Kong and India shows that fall down accident was the major cause of TBI among children 14, 27, 28, 29 Other study conducted in China reveled that assaults was the most common mechanism of traumatic brain injury in children 30.Study done in India reveled that TBI of children who had additional injury with chest and spinal cord significantly associated with unfavorable outcome.And other similar study in and chain showed that TBI children who had chest injury significantly associated with unfavorable outcome 15, 16 .
Early availability of TBI patient in hospital for neurotrauma management is very crucial for early privation of ongoing pathological brain injury. 31 study in Uganda and Pakistan revealed that let to hospital presentation more than four hours is associated with unfavorable outcome. 17, 32 And other study in United States reveled that short (< 1day) in hospital length of stay associated with unfavorable outcomes of traumatic brain injury. 33
Pathophysiology of TBI classified as Primary brain injury which occurs during at time of trauma includes soft tissue injury , bleeding in to extra axial (epidural ,sub Dural, subarachnoid space and intraventricular), skull fracture and intracranial lesions (DAI, cortical contusion and vascular injury) and were as secondary brain injury occurs after trauma due to hypotension, hypoxia and increased ICP which is significatively associated with unfavorable outcome. 29, 34, 35
A systematic study conducted in Europe, as well as other studies in, Hong Kong, Germany and Pakistan, showed that having a skull fracture on a CT scan finding were significantly associated with a unfavorable outcome of traumatic brain injury in children .17, 25, 26, 27
Immediate management of TBI needs multidisciplinary approach such as resuscitation, management airway , intubation when GCS < 8 TBI, monitoring ICP, prevention of secondary TBI and neurosurgical management. 36, 37
Study conducted in USA, Singapore, and Ethiopia reveled that Presence of ICP were significantly associated with unfavorable outcome of traumatic brain injury .10, 11, 38
In Germany Study conducted in short term outcome of severe TBI showed that decompressive craniotomy significantly associated with unfavorable outcome of TBI. 12 other similar study done in India shows that sever TBI and Fixed bilateral dilated pupil significantly associated with unfavorable outcome of TBI in children. 15
Study conducted in Singapore showed that clinical presentation of vomiting, severity of TBI , hypotension, use of inotropic and comorbid with anemia significantly associated with unfavorable outcome. 11And other similar Study in chain shows that SAH significantly associated with unfavorable outcome. 16 Study in Togo was reported that presence hypotension , comorbidity with anemia, hyperthermia and GCS of < 6 associated with unfavorable outcome of TBI. 21 Other similar study conducted in, Singapore , Ankara Turkey and Hawassa Ethiopia showed that hyperglycemia were significantly associated with unfavorable outcome of TBI 10, 39, 40.
Methods and materials
Study design and Period
Institutional-based cross-sectional study was conducted from May 16 to June 15, 2022 G.C.
Study area
This study was carried out in Comprehensive Specialized Hospitals of the Amhara National Regional State in Ethiopia. Amhara National regional state is one federal republics of Ethiopia with an approximate land area of 170000 square kilometers. 41 The territory is divided into 12 administrative zones, three city administrations, and 83 districts. The Amhara National Regional Health Bureau's Annual Performance Report shows the region has 81 Hospitals, 858 Health centers, and 3560 Health posts. Among Hospitals eight of them are Comprehensive Specialized Hospital these are University of Gondar, Dessie, Felege-Hiwot, Tibebe-Ghion, Debre-Markos, Waldiy, Debre Tabor, and Debebirhan Comprehensive Specialized Hospital which are serve for population within the region. 42 These Hospitals provide surgical, medical, pediatric, maternal, and other types of care to their patients. These hospitals have specialty units for cardiology, respiratory, neurology, dermatology, and sexually transmitted diseases, as well as gastroenterology, infectious diseases, orthopedics, gynecology and obstetrics, hematology, and intensive care units. Five Comprehensive Specialized Hospitals was chosen by simple random lottery methods from a total of eight Comprehensive Specialized Hospitals those are University of Gondar, Felege-Hiwot, Tibebe-Ghion, Debre-Markos, and Debre-Berhan Compressive Specialized Hospitals.
Objectives
General objective
To assess the outcome of traumatic brain injury and its associated factors among pediatrics patients treated in Amhara National Regional State Comprehensive Specialized Hospitals, Ethiopia 2022.
Specific objectives
To determine the outcome of traumatic brain injury among pediatrics patients treated in Amhara National Regional State Comprehensive Specialized Hospitals, Ethiopia 2022.
To identify the factors associated with outcome of traumatic brain injury among pediatrics patients treated in Amhara National Regional State Comprehensive Specialized Hospitals, Ethiopia 2022.
Population
Source population
All pediatric patients with traumatic brain injuries were treated in Amahera National Regional State Comprehensive Specialized Hospitals.
Study population
Study population was all selected traumatic brain injury pediatrics patients age of 1 month to 18 years who were treated at Amhara National Regional State Comprehensive Specialized Hospitals from January 1, 2019 and December 30, 2021.
Eligibility Criteria
This study includes traumatic brain injury pediatrics patients age of one month to 18 years who was treated in Amhara National Regional State Comprehensive Specialized Hospitals. However, TBI pediatrics patients who were died on arrival, referred to another institution and refused treatment after medical advice to their families was excluded from this study.
Sample Size Determination
The required sample size was calculated for the dependent variable by using the single population proportion formula. The anticipated proportion of outcome (P= 50%) was taken because no previous study was done in under 18 years of children in Ethiopia. By considering CI= 95% and the margin of error (D) = 5% in order to increase the precision of the study. Hence, the required sample size was:
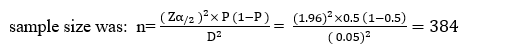
n = the minimum sample size required
P= estimated proportion (50%) = 0.5
Z = the standard value of confidence level of α=95%
D = the margin of error between the sample and the population (0.05).
By considering 10% incomplete data rate the final sample size was 423.
Sampling Technique and Procedure
From January 1, 2019 to December 30, 2021 G.C, the total estimated number of TBI pediatric patients who visited at selected Amhara National Regional State Comprehensive Specialized Hospitals, Ethiopia was 3,384. Our study participants were chosen by using a systematic random sampling technique after proportional allocation for each selected hospital at every k interval: K=N/n= 3,384/423, K=8. The first MRN of study participants was identified from each hospital's registry books to select sampled study participants during the study period, and then every k patient chart was selected until reached to the desired sample size and the first participant was chosen by lottery methods. As a result, the diagram below depicts how study participants were chosen, with proportional allocation from each hospital (See Figure 1).
Figure 1. Sampling procedure for the outcome of TBI among pediatrics TBI who vested in Amhara National Regional State CSHs from January 1,2019 to December 30,2021.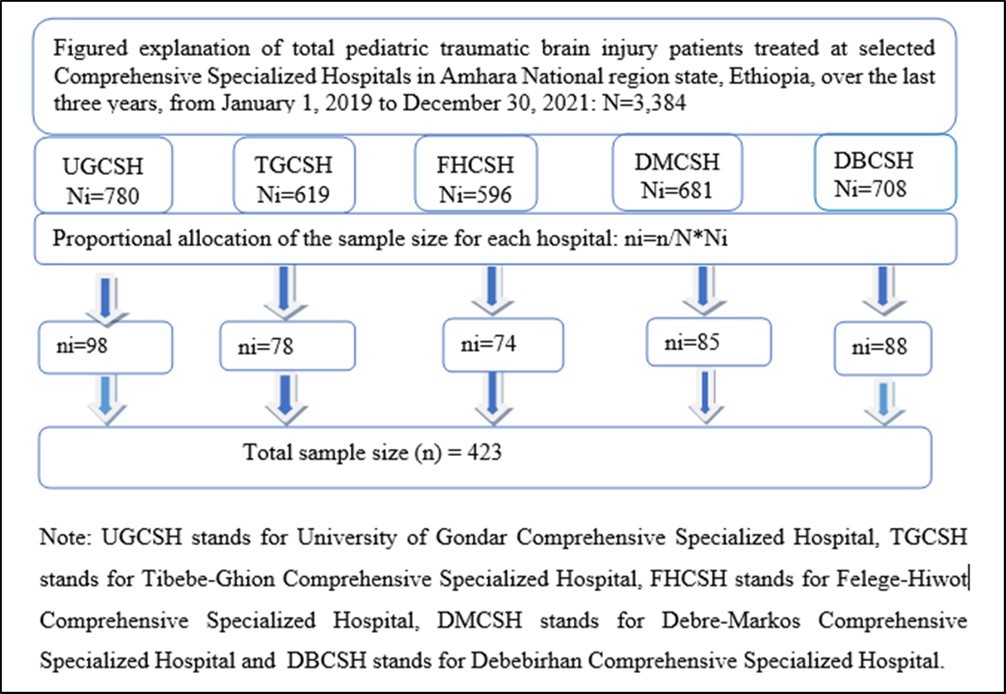
Operational definitions
Pediatrics age patients: age of younger than 18 years old .22, 43, 44
Glasgow coma scale: It is Generated Clinical Standards that objectively measure a patient's neurological status based on their Motor Response graded out of 6, Eye Opening graded out of 4, Verbal Response graded out of 5, and total out of 15 .45
Severity of traumatic brain injury: Mild, moderate, and severe traumatic brain injuries are classified as GCS 13-15, 9-12, and 3-8, respectively 11
Glasgow outcome scale: is a global scale for measuring functional outcome in patients with traumatic brain injury that rates patient status on a five-point : Dead, vegetative state, severe disability, moderate disability, and good recovery . 47, 48
Outcome of TBI : Based on the Glasco outcome scale at the time of discharge, which is unfavorable outcome (GOS 1 - 3) and favorable outcome (GOS 4 and 5). 18, 43, 44
Additional injury: when there is more than one body system involved in the injury.49
Hypothermia and Hyperthermia: by axillary measurement hypothermia < 36.5°C and hyperthermic >37.5°C. 50
Hypoxia: is defined as inadequate oxygen in tissues for normal cell and organ function. It can happen even when circulation is normal not or occurs when Sap02 < 90 %. 51
Hypertension and Hypotension: considered as based on with respective age and sex of pediatrics population ≥95th percentile and below the 5th percentile respectively.52
Hyperglycemia and Hypoglycemia: consideration of random blood glucose on admission >200mg/dl and <70 mg/dl respectively40
Data collection procedures and Tools
The outcome and other explanatory data of traumatic brain injury in children were collected by using data extraction tools that were developed aftera deeply review of different literature. 13, 16, 17, 23, 28, 50, 51.Data were collected from patient charts and medical records of sampled study participants after obtaining MRN from the hospital registration logbooks. Five BSC nurses and two MSC nurse supervisors with prior data collection experience participated in data collection procedures. Five parts of the data extraction check list were used to assess all important variables. These are sociodemographic variables, pattern of injury related variables, clinical and management related variables, time-related variables, and traumatic brain injury outcome variables. Outcome of traumatic brain injury was assessed by Glasgow outcome scale . 47, 48, 51
Data quality assurance
To maintain the quality of data, pretest was done on 5% of samples at University of Gondar Comprehensive Specialized Hospital. The pre-test of data extraction tools Cronbach alpha result was 0.75. After the pretest was done ambiguous words and concepts were corrected accordingly. Training was given to data collectors and supervisors regarding to the data collection methods, checklist content, instruction, and includes practical demonstration. During data collection close supervision, and fast feedback was given by both principal investigator and supervisors. Necessary adjustments were done consistently on daily based and before starting data entry the collected data were checked for Inconsistencies, coding errors, completeness, correctness, clarity, missing values thoroughly and data entry was done.
Data processing and analysis
After the data was collected from patient charts by using a data extraction tools and data quality assurance was assured the data were cleaned, coded and enter to Epi-info version 7 then transfer data to SPSS version of 25, for descriptive and analytic Statistical analysis. Then after the data cleaning, coding and recoding was done and cross-tabulation to assess the distribution of unfavorable and favorable outcomes of TBI in pediatrics and the data was processed by carrying out simple descriptive statistics. For categorical variable frequency with percentage distribution were employed. Box plot graphs were used to check outliers for continuous data, and the variance inflation factor (VIF) was used to determine whether there were any multi-collinear. Association of TBI related variables and demographic characteristics with the outcome of TBI in pediatrics patient at discharge were analyzed by Chi square and Binary logistic regression analysis. model goodness-of-fit was checked by using the Hosmer-Lemeshow tests (P= 0.514). Those variables with a p-value < 0.25 in bi-variable analysis were entered into multi-variable analysis with back ward stepwise method. Then, in multivariable analysis, variables of P-value ≤ 0.05 were declared as significantly associated factors with the outcome of traumatic brain injury in pediatrics. The odds ratio was used to determine the strength of association between dependent and independent variables.
Ethical clearances
The study was approved by the University of Gondar, College of Medicine and Health Sciences, School of Nursing Ethical and Research Review Committee on behalf of the Institutional Review Board (IRB) with an ethical clearance number S/N/237/2014 was given to the principal investigator to preceding the study implementation. since the study was done by retrospectively chart review without contacting patients the official letters were sent for each respective comprehensive specialized hospitals of Amhara national regional state in which the study was conducted. After supportive letter was obtained from each respective Hospital Medical Director’s office data was retrieved from the patient’s chart and records. Confidentially of all information were kept and no individual identifiers were collected.
Results
There were 3,384 TBI in pediatrics visited in Amhara National Regional State Comprehensive Specialized Hospitals during the past three years, from January 1, 2019 G.C to December 30, 2021G.C. Data were gathered by using data extraction tools, and 404 charts had complete documentation from 423 randomly selected charts, with a response rate of 95.5 %.
Socio-demographic characteristics of respondent
The Mean age of study participant was 9.2 ± 5.4 years and the majority of victims were age range of 5-12 years, 150(37.1%). Male accounts higher proportion of TBI, 264(65.3%) with male to female ratio of 2:1. More than half of TBI cases were come from rural 251(62.1%). The majority of traumatic brain injury case children comes from the scene 173(42.8%) and the commonest way of transportation was ambulance 173 (42.8%). (See Table 1).
Table 1. Socio-demographic characteristics of TBI among pediatrics patients in CSHs of Amhara regional state, Ethiopia from January 1,2019 to December 30, 2021G.C(N=404).| Variables | Category | Outcome of TBI in children | Total N (%) | |
| unfavorable | Favorable | |||
| Age in years | <5 | 15 | 112 | 127(31.4%) |
| 5-12 | 18 | 132 | 150(37.1%) | |
| 13-18 | 16 | 111 | 127(31.4%) | |
| sex | Male | 28 | 236 | 264(65.3%) |
| Female | 21 | 119 | 140(34.7%) | |
| Resident | Rural | 35 | 216 | 251(62.1%) |
| Urban | 14 | 139 | 153(37.9%) | |
| Origin of referral | From health center | 15 | 109 | 124(30.7%) |
| From hospital | 16 | 63 | 79(19.6%) | |
| From the scene | 17 | 156 | 173(42.8%) | |
| Others | 1 | 27 | 28(6.9%) | |
| Mode of arrival | Ambulance | 30 | 88 | 118(29.2%) |
| Bajaj | 0 | 102 | 102(25.2%) | |
| Taxi | 4 | 107 | 111(27.5%) | |
| Other * | 15 | 58 | 73(18.1%) | |
Pattern of injury related characteristics of respondent
In this study, fall down accident was the commonest mechanism of traumatic brain injury in children 190(47%), followed by road traffic accident 97(24%). (See Figure 2)
Figure 2. mechanism of injury among pediatrics TBI who visited in Amhara regional state CSHs from January 1,2019 to December 30,2021 GC.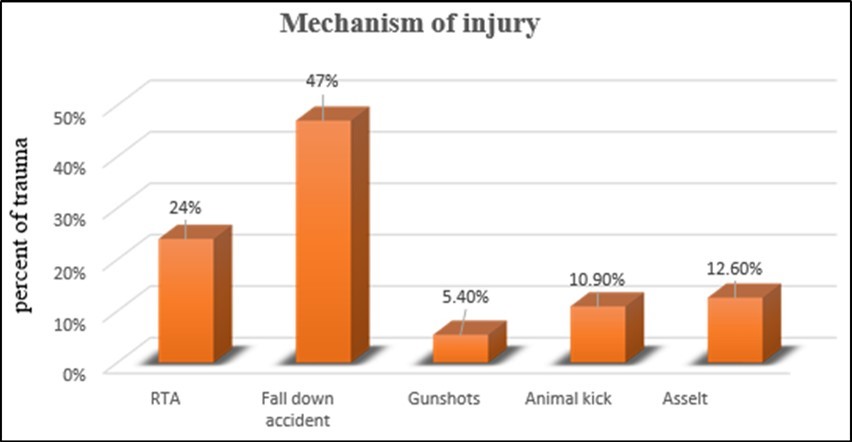
Additional injury with traumatic brain injury of children
At the time of admission, 160 (39.5 %) of the total study participants had additional injuries. The most common additional injuries in children with traumatic brain injury were chest/abdominal injuries 59(36.8%) followed by soft tissue injuries 55(34.38%), maxillofacial injuries 31(19.38%) and vertebral bone fractures 15(9.38%). (See Figure 3)
Figure 3. Additional injury among pediatrics TBI patients treated in Amhara National Regional State CSHs from January 1,2019 to December 30,2021.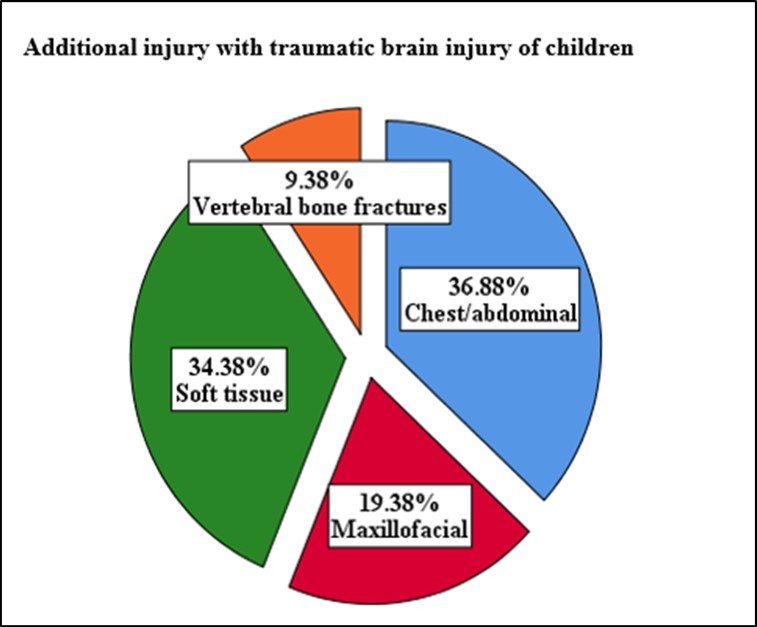
Clinical characteristics respondent
From the total study subjects 221(54.7%),147(36.4%) and 36(8.9%) mild, moderate and sever traumatic brain injury respectively. concerning vital sign on admission Body temperature half of the study subjects had normal body temperature 204(50.5%) and more than one-fourth of study subjects had hypoxia on addition ,112(27.7%), nearly half of case 185(45.8%) had history of Loss of consciousness and 40(9.9%) study participant had Convulsion at presentation. (See Table 2).
Table 2. Clinical characteristics of TBI among pediatrics traumatic brain injury who vested in Amhara national regional state CSHs from January 1,2019 to December 30, 2021G.C(N=404).| Variable | Category | Outcome of TBI in children | Total N (%) | |
|---|---|---|---|---|
| unfavorable | Favorable | |||
| GCS score | Mild (13-15) | 12 | 209 | 221(54.7%) |
| Moderate (9-12) | 22 | 125 | 147(36.4%) | |
| Sever (3-8) | 15 | 21 | 36(8.9%) | |
| Blood pressure | Hypertension | 9 | 15 | 24(5.9%) |
| Hypotension | 16 | 13 | 29(7.2%) | |
| Normal | 12 | 111 | 123(30.4%) | |
| Not investigated | 12 | 216 | 228(56.4%) | |
| Blood glucose | <70 mg/dl | 10 | 50 | 60(14.9%) |
| level | >200 mg/dl | 15 | 47 | 62(15.3%) |
| 70-200 mg/dl | 17 | 125 | 142(35.7%) | |
| Not investigated | 7 | 133 | 140(34.7%) | |
| Body To on | Hyperthermic | 13 | 69 | 82(20.3%) |
| admission | Hypothermic | 15 | 103 | 118(29.2%) |
| Normothermic | 21 | 183 | 204(50.5%) | |
| O2 saturation on | Hypoxia | 24 | 88 | 112(27.7%) |
| admission | Normal | 25 | 267 | 292(72.3%) |
| History of Loss of consciousness | Yes | 45 | 140 | 185(45.8%) |
| No | 4 | 215 | 219(54.2%) | |
| Convulsion at presentation | Yes | 7 | 33 | 40(9.9%) |
| No | 42 | 322 | 364(90.1%) | |
| Battle sign | Yes | 16 | 13 | 29(7.2%) |
| No | 33 | 342 | 375(92.8%) | |
| Cerebrospinal fluid | CSF Otorrhea | 7 | 13 | 20(5%) |
| leakage | CSF rhinorrhea | 3 | 9 | 12(3%) |
| No CSF leakage | 39 | 333 | 372(92.1%) | |
| Increased ICP sign | Yes | 34 | 62 | 96(23.8%) |
| No | 15 | 293 | 308(76.2%) | |
| Types of increased | Decreased mentation | 22 | 49 | 71(74%) |
| ICP sign | Hypertension | 8 | 4 | 12(12.5%) |
| Vomiting | 3 | 10 | 13(13.5%) | |
| Pupillary sign | Bilateral fixed | 18 | 15 | 33(8.2%) |
| Bilaterally dilated | 9 | 7 | 16(4%) | |
| Unilaterally fixed | 3 | 15 | 18(4.5%) | |
| Midsized and reactive | 18 | 319 | 337(83.4%) | |
| Comorbidity | Yes | 20 | 53 | 73(18.1%) |
| No | 29 | 302 | 331(81.9%) | |
| Types of | Diabetes mellitus | 1 | 7 | 8(11%) |
| comorbidities | Epilepsy | 2 | 5 | 7(9.6%) |
| Anemia | 15 | 22 | 37(50.7%) | |
| Others* | 2 | 19 | 21(28.8%) | |
Management-related factor with outcome of traumatic brain injury
In this study, out of 404 patients, 133 (32.9%) had pre-hospital care. Of those patients 89(66.9%) received basic first aid after injury were happening, followed by Medication like tetanus anti -toxoid, antipain 31(23.3%). (See Table 3)
Table 3. Management related characteristics of pediatrics TBI who vested in Amhara National Regional State CSHs from January 1,2019 to December 30, 2021G.C (N=404).| Variables | Category | Outcome of TBI | Total N (%) | |
| unfavorable | Favorable | |||
| Prehospital care | Yes | 15 | 118 | 133(32.9%) |
| No | 34 | 237 | 271(67.1%) | |
| Type ofPrehospital care | Basic First aid | 4 | 85 | 89(66.9%) |
| Medication | 7 | 24 | 31(23.3%) | |
| Resuscitation | 4 | 9 | 13(9.8%) | |
| Head CT Done | Yes | 24 | 154 | 178(44.1%) |
| No | 25 | 201 | 226(55.9%) | |
| Ct-scan finding | Contusion/DAI | 5 | 9 | 14(7.8%) |
| Depressed skull #withcontusion, DAI+, ICH | 7 | 29 | 36(20%) | |
| Intracranial bleeding | 7 | 14 | 21(11.7%) | |
| Skull fracture | 6 | 47 | 53(29.4%) | |
| Normal finding | 1 | 55 | 56(31.1%) | |
| Skull X-ray done | Yes | 21 | 182 | 203(51%) |
| No | 24 | 171 | 195(49%) | |
| Skull X-rayfinding | Depressed skull # | 9 | 22 | 31(15.2%) |
| Linear skull fracture | 0 | 42 | 42(20.6%) | |
| Normal finding | 13 | 117 | 130(64.2%) | |
| Use of Inotropicmedication | Yes | 4 | 13 | 17(4.2%) |
| No | 45 | 342 | 387(95.8%) | |
| Management typein hospital | Conservative* | 26 | 316 | 342(84.7%) |
| Surgical | 8 | 25 | 33(8.2%) | |
| Both | 15 | 14 | 29(7.2%) | |
| Surgicalintervention | Burr hole | 4 | 3 | 7(11.3%) |
| Craniotomy/evacuation | 210 | 4 | 6(9.7%) | |
| Elevation of depressed skull # | 29 | 39(62.9%) | ||
| Irrigation &debridement | 6 | 4 | 10(16.1%) | |
Time-related characteristics of traumatic brain injury pediatrics
The median duration of Prehospital length of stay were 5 hours (IQ, R 2-14). most of case, 156(38.6%) seek health care service within 5-24 hours,116(28.7%) of case seek health care within 2-4 hours, 94(23.3%) case seek health care with in ≤ 1 hours and 38(9.4%) of case were come to hospital for health care service with ≥ 24 hours. The median in hospital length of stay were 3 days (IQ, R 1-7). majority of the traumatic brain injury pediatrics patients in-hospital length stay were from 2 – 7 days 245(60.6%), ≤ 1 days 121(30%) and 38(9.4%) of case stay more than 7 days. (See Table 4).
Table 4. Time-related variables for outcomes of TBI pediatrics who vested in Amhara national regional state CSH from January 1,2019 to December 30, 2021G.C(N=404).| Variables | Category | Outcome of TBI in children | Total N (%) | |
| Unfavorable | Favorable | |||
| Prehospital lengthof stay | ≤1hours | 7 | 87 | 94(23.3%) |
| 2-4hours | 15 | 101 | 116(28.7%) | |
| 5-24hours | 21 | 135 | 156(38.6%) | |
| ≥24hours | 6 | 32 | 38(9.4%) | |
| In hospital lengthof stay | ≤ 1 days | 3 | 118 | 121(30%) |
| 2-7 days | 32 | 213 | 245(60.6%) | |
| >7 days | 14 | 24 | 38(9.4%) | |
Outcomes of traumatic brain injury at time of discharge from hospital
The overall prevalence of unfavorable outcomes of traumatic brain injury among pediatrics patient treated in Amahera National Regional State Compressive Specialized Hospitals were found that 12.13% (95% CI: 9.1% - 15.7 %) as indicated in figure five. Based on the Glasgow Outcome Score, nearly three-four of pediatric patients with traumatic brain injuries had good recovery at the time of discharge 292 (72.3%), followed by moderate disability 63 (19.6%), severe disability 19 (4.7%), persistent vegetative state 6 (1.5%), and death 24(5.9 %) of cases (Figure 4).
Figure 4. Outcome of TBI among pediatrics patients treated in Compressive Specialized Hospitals of Amhara National Regional State from January 1,2019 to December 30,2021G.C.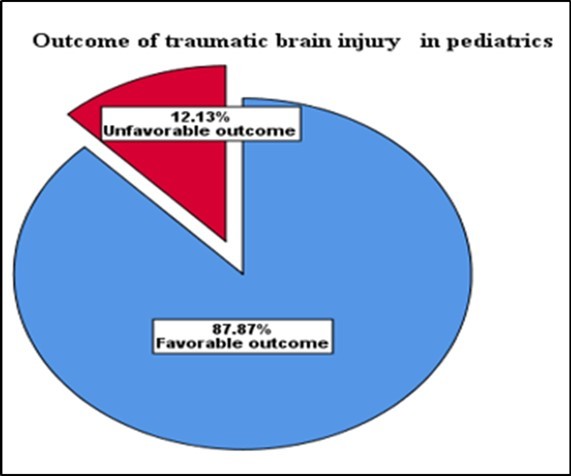
Factors associated with outcomes of traumatic brain injury in pediatrics
In binary logistic regression analysis, the sex of respondent, Residency, severity of traumatic brain injury, Blood glucose Level, Body temperatures, O2 saturation, Sign of increased ICP, medical Comorbidity and Prehospital length of stay were significantly associated with unfavorable outcome of traumatic brain injury. However, in multivariable logistic regression analysis only Severity TBI, blood glucose level, Sign of increased ICP and medical Comorbidity were significantly associated with outcome of traumatic brain injury patient.
This study shows having sever TBI (GCS 3-8) [AOR: 5.11(CI :1.8-14.48) and moderate TBI (GCS9-12) (AOR:2.44(CI:1.07-5.58) were significantly associated with unfavorable outcome. The severity of traumatic brain injury among sever traumatic brain injury were 5.11 times and among moderate TBI 2.44 times higher odds of developing unfavorable outcome as compared to those who had mild traumatic brain injury.
Being Hyperglycemic was 5.84 times more likely to develop unfavorable outcome of TBI than those blood glucoses levels were with in normal range (AOR: 3.01 (CI:1.1-8.04). And The odds of unfavorable outcome among those who had sign of increased ICP were 7.4 times higher than those had no sign of increased ICP (AOR:7.4(CI:3.5-15.26).
The finding of these study shows that the odds of having unfavorable outcome from traumatic brain injury were 2.65 times higher in those having medical comorbidity at presentation than those not having medical comorbidity (AOR: 2.65(CI:1.19-5.91). (See Table 5)
Table 5. Bivariable and multivariable logistic regression analysis of factors associated with outcome of TBI pediatrics patients who visited in Amhara national regional state CSHs from January 1, 2019 to December 30, 2021G.C.| Variable | Category | Outcome of TBI | COR (95% CI) | AOR (95%CI) | P-value | |
| Unfavorable | Favorable | |||||
| Sex | Male | 28 | 236 | 0.67 (0.36-1.2) | 0.81(0.38-1.70) | 0.58 |
| Female | 21 | 119 | 1 | 1 | ||
| Residency | Rural | 35 | 216 | 1.6(0.84-3.09) | 1.24(0.57-2.72) | 0.589 |
| Urban | 14 | 139 | 1 | 1 | ||
| GCS category | 3-8 | 15 | 21 | 12.4(5.1-30.04) | 5.11(1.8-14.48) | 0.002* |
| 9-12 | 22 | 125 | 3.0(1.46-6.40) | 2.44(1.07-5.58) | 0.033* | |
| 13-15 | 12 | 209 | 1 | 1 | ||
| Blood glucose Level | <70mg/dl | 10 | 50 | 1.4(0.63-3.43) | 1.94(0.71-5.30) | 0.193 |
| >200mg/dl | 15 | 47 | 2.34(1.08-5.07) | 3.01(1.12-8.04) | 0.028* | |
| Not.Ix | 7 | 133 | 0.38(0.15-0.96) | 0.58(0.21- 1.5) | 0.289 | |
| 70-200mg/dl | 17 | 125 | 1 | 1 | ||
| Body temperatures | Hyperthermic | 13 | 69 | 1.64(0.98-4.71) | 1.44(0.57-3.64) | 0.43 |
| Hypothermic | 15 | 103 | 1.26(0.62-2.56) | 1.89(0.81-4.38) | 0.13 | |
| Normothermic | 21 | 183 | 1 | 1 | ||
| O2 saturation | Hypoxia | 24 | 88 | 2.91(1.58-5.35) | 0.99(0.44-2.26) | 0.99 |
| Normal | 25 | 267 | 1 | 1 | ||
| Sign of ICP | Yes | 34 | 62 | 10.7(5.5-20.8) | 7.4(3.5-15.26) | 0.000* |
| No | 15 | 293 | 1 | 1 | ||
| Medical Comorbidity | Yes | 20 | 53 | 3.13(0.1.8-5.2) | 2.65(1.19-5.91) | 0.017* |
| No | 29 | 302 | 1 | 1 | ||
| Prehospital length of stay | ≤1 Hours | 7 | 87 | 1 | 1 | |
| 2-4 Hours | 15 | 101 | 1.84(.72-4.73) | 0.96(0.23-3.96) | 0.96 | |
| 5-24 Hours | 21 | 135 | 1.93(0.78-4.74) | 1.03(0.29-3.6) | 0.96 | |
| >24 Hours | 6 | 32 | 2.3(0.72-7.45) | 1.60(0.47-5.41) | 0.44 | |
Discussion
The aim of this study was to evaluate the outcome of traumatic brain injury and associated factors in pediatric patients seen at Amhara National Regional State Comprehensive Specialized Hospitals in Ethiopia. The overall prevalence of unfavorable outcome of traumatic brain injury among pediatrics patients was found that 12.13 % (95 % CI: 9.1 % - 15.7 % ).This study finding was consistent with study conducted in India 10.7 % (15) and study conducted in Saudi Arabia 14.8% (19) . In contrast, it was higher than study conducted in Netherlands 5% (12) . This difference could be due to variability in socio demographic states, study design and availability of advance equipment like CT-scan and MRI. On the other hand , the current study result was lower than study conducted in Mulago National Referral Hospital in Uganda 21.25% (20). The possible discrepancy may be due to difference in study setting, study design and study period it was conducted in community based and long term follow up study.
The findings of this study indicated that pediatrics with severe TBI 5.11 times and moderate TBI 2.44 higher risk of unfavorable outcomes than those who had mild traumatic brain injury. This finding were consistent with in study conducted in Germany, Singapore and Togo.11, 12, 21 The similarities may be due to increased risk for secondary brain injury in severe and moderate TBI cases , like hypoxia, and elevated intracranial pressures. 29, 34, 35
This study also revealed that Hyperglycemia in traumatic brain injury pediatrics patients were 3.01 times more likely to develop unfavorable outcome than those with normal range of blood glaucous level , This study finding in line with study conducted in Singapore , Ankara Turkey and Hawassa Ethiopia. 10, 39, 40 Possibility explanation could be impaired cerebral mitochondrial dysfunction following TBI and acute stress response causes hyperglycemia, which worsens impairments of microcirculatory blood flow, increases blood-brain barrier permeability, promotes inflammation, triggers osmotic diuresis, hypovolemia, and immunosuppression .27, 40, 58
The odds of unfavorable outcome among those TBI pediatrics patients who had sign of increased intracranial pressures 7.4 times higher than those who had not increased intracranial pressures signs , This finding is supported by a study done united states of America, Singapore and Hawassa Ethiopia (10,11,38). This may due to the fact that brain tissue itself is swelling from injury that the fluid under pressure tends to deform the brain and pushes tissue results Diffuse cerebral ischemia of the brain (60,61).
This study finding showed that the odds of having unfavorable outcome from TBI pediatrics patients were 2.65 times higher in those having medical comorbidity than those had no medical comorbidity. This finding in line with study conducted in Togo and Singapore. 11, 21 The possible explanation of similarity may be due to having comorbid medical illness like anemia, epilepsy and heart failures compromise adequate oxygenated blood supply to the brain .62, 63
Limitation of study
One of the study's limitations was dealing with insufficient data from the patients' charts. However, data collators received training, and incomplete chart was treated as a non-response and lack of local data for comparison and conclusion.
Conclusion and recommendation
According to this study, about twelve present of traumatic brain injury of pediatrics patient results unfavorable outcome and the most common predictive factors associated with unfavorable outcome of traumatic brain injury were severity of traumatic brain injury, signs of increased ICP, hyperglycemia and medical comorbidity. This study indicates that need for precaution and appropriate management for moderate and sever form of traumatic brain injury, sign of increased intracranial pressures, hyperglycemia and medical comorbidity. To address possible risk factors including children's educational backgrounds, families, and other variables that are not properly captured from patient charts, it is preferable to conduct prospective studies.
List of Abbreviation/Acronym
AOR - Adjusted Odds Ratio
CI - Confidence Interval
COD - Crud Odds Ratio
CSH - Comprehensive Specialized Hospital
CSF - Cerebrospinal Fluid
DAI -Diffuse Axonal Injury
GCS - Glasgow Coma Scale
GOS -Glasgow Outcome Scale
ICH -Intracranial hemorrhage
ICP - Intracranial pressure
ICU - Intensive Care Unit
RTA - Road Traffic Accident
TBI -Traumatic brain injury
WHO - World Health Organization
Declarations
Confidentiality
To reassure confidentiality, the data on the chart was collected without the names of the patients, and the information which is collected from this research project were keep confidential. In addition, it was not be revealed to anyone except the investigator.
Consent for publication
Not applicable
Availability of data and material
The datasets used and/or analyzed during the current study is available upon request from the corresponding author and Co- authors.
Funding
There is no source of funding for this research. All costs were covered by the authors.
Author’s contribution
Aytenew Getabalew conceived, designed the study, analyzed the data and prepared the manuscript. Abebaw Alemayehu, Kennean Mekonnen, Bikis Liyew and Belete Melesegn assisted with the design conception, advising and reviewing the manuscript.
Acknowledgements
The authors are grateful for university of Gondar, hospitals administration staff for their cooperation and helpful information, data collectors' and supervisor’s cooperation throughout the data collection.