Abstract
Objective
Meningiomas are most common intracranial benign tumors comprising around one third of all intracranial neoplasms, and typically have benign and indolent nature with slow-growing behaviour. Benign meningiomas are slow growing tumors typically following an indolent disease course. Nevertheless, atypical or anaplastic meningiomas may follow a more aggressive disease course with invasion of critical structures and recurrences. In the current study, we evaluate the incorporation of magnetic resonance imaging (MRI) for radiosurgery treatment planning of atypical meningiomas.
Materials and Methods
Atypical meningioma radiosurgery target volume determination with and without incorporation of MRI has been evaluated. Ground truth target volume used as the reference has been outlined by the board-certified group of radiation oncologists after comprehensive assessment, thorough collaboration and consensus.
Results
Target volume definition by use of Computed Tomography (CT)-only imaging and by CT-MR fusion based imaging has been comparatively evaluated in this study for linear accelerator (LINAC)-based radiosurgical management of atypical meningioma. Ground truth target volume defined by the board-certified radiation oncologists after detailed evaluation, collaboration, colleague peer review and consensus has been found to be identical to target determination by use of CT-MR fusion based imaging.
Conclusion
Despite significant progress in neurosurgical techniques over the years, complete surgical resection may not be feasible in the presence of meningiomas located at eloquent brain areas in close association with important neurovascular structures. RT may have a role in multidisciplinary management of meningiomas. Incorporation of MRI into treatment planning for radiosurgery of atypical meningiomas may improve target definition despite the need for further supporting evidence.
Author Contributions
Academic Editor: Amal Ibrahim Hassan Ibrahim, Department of Radioisotopes, Nuclear Research Centre, Atomic Energy Authority
Checked for plagiarism: Yes
Review by: Single-blind
Copyright © 2020 Selcuk Demiral, et al.
 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Competing interests
The authors have declared that no competing interests exist.
Citation:
Introduction
Meningiomas are most common intracranial benign tumors comprising around one third of all intracranial neoplasms, and typically have benign and indolent nature with slow-growing behaviour 1, 2, 3. These dural-based tumors have been considered to arise from the arachnoid cap or meningothelial cells present in the arachnoid layer of the meninges 4, 5.
Presentation is typically at the 6th to 8th decades of life and incidence increases with increasing age 2, 3. Meningiomas may be histologically classified as benign, atypical, or anaplastic (malignant) meningiomas according to World Health Organization (WHO) classification scheme with the most common type being WHO grade I benign meningiomas 2, 5.
Meningiomas can be located at several locations throughout the CNS, however, supratentorial region is the most frequent location followed by the skull base and posterior fossa6. Meningiomas placed at the supratentorial region are parafalcine meningiomas, parasagittal meningiomas, intraventricular meningiomas and convexity meningiomas. Meningiomas occurring at the skull base include the tuberculum sellae meningiomas, sphenoid ridge meningiomas, petroclival meningiomas, olfactory groove meningiomas, cavernous sinus meningiomas, and intraorbital meningiomas. Finally, meningiomas placed at posterior fossa region include the cerebellar convexity meningiomas, cerebellopontine angle meningiomas, jugular foramen meningiomas, foramen magnum meningiomas, and peritorcular meningiomas6.
Benign meningiomas are slow growing tumors typically following an indolent disease course. Nevertheless, atypical or anaplastic meningiomas may follow a more aggressive disease course with invasion of critical structures and recurrences 7, 8, 9.
Magnetic resonance imaging (MRI) constitutes the principal modality for imaging of meningiomas. Nevertheless, computed tomography (CT) imaging may aid in detection of tumoral calcifications, intraosseous growth of the tumor particularly for base of skull lesions, and hyperostosis of the neighboring bone10. MRI may be utilized for detection of the dural tail as post-contrast linear thickening of duramater in vicinity of the meningioma lesion in some patients and may provide improved contrast differentiation, which may assist in differentiation between intra axial and extra axial meningioma lesions. Typically, a meningioma lesion is visualized as an extra axial mass with well-defined borders. Homogeneous contrast enhancement is typical, nevertheless, areas of central necrosis or calcification may not show enhancement. Incidental detection of meningiomas is quite common, however, affected patients may also suffer from a variety of symptoms associated with location of meningioma.
Active surveillance with periodical neuroimaging can be a viable option for incidentally detected and asymptomatic meningiomas 10, 11. However, surgery has an essential role in treatment particularly in the presence of symptoms due to the mass effect from large lesions at surgically accessible locations 12. Simpson described the 5 grades of meningioma removal and reported an association between aggressiveness of surgical resection and subsequent recurrences of meningiomas 12. Although there has been significant progress in neurosurgical techniques over the years, complete surgical resection may not be feasible in the presence of tumors located at eloquent brain areas in close relationship with important neurovascular structures 13, 14, 15, 16. Despite surgical resection of some meningioma lesions, recurrences may occur 11, 12. A multimodality treatment strategy with less extensive surgical resection followed by adjuvant radiation therapy (RT) may be preferred in selected patients to avoid excessive toxicity16. Advanced RT techniques and radiosurgery in the forms of Stereotactic Radiosurgery (SRS), Stereotactic Body Radiotherapy (SBRT) and Hypofractionated Stereotactic Radiation Therapy (HFSRT) can be utilized for focused irradiation of several CNS disorders as well as tumors located throughout the human body with encouraging treatment outcomes 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37.
Accurate definition of the target volume is an integral part of successful radiosurgery applications given the smaller treatment volumes receiving higher doses per fraction. Radiosurgery treatment planning has been traditionally based on CT-simulation images of the patients acquired at treatment position. In the current study, we evaluate the incorporation of MRI for radiosurgery treatment planning of atypical meningiomas.
Materials and Methods
Atypical meningioma radiosurgery target volume determination with and without incorporation of MRI has been evaluated. Ground truth target volume used as the reference has been outlined by the board-certified group of radiation oncologists after comprehensive assessment, thorough collaboration and consensus. Informed consents have been provided before treatment, and management with radiosurgery has been decided by multidisciplinary collaboration of a team of experts from neuroradiology, neurosurgery, and radiation oncology. Comprehensive evaluation has been performed taking into account the lesion location, size, symptomatology and patient preferences. CT-simulation for radiosurgery treatment planning has been performed at the CT-simulator (GE Lightspeed RT, GE Healthcare, Chalfont St. Giles, UK) available at our department. Planning CT images have been acquired at CT-simulation and these images have been transferred to the contouring workstation (SimMD, GE, UK) for delineation of treatment volumes and critical structures. Target volume definition for radiosurgical management has been performed by use of the CT-simulation images only or fused CT and T1 gadolinium-enhanced MR images. Target definition with CT only and by incorporation of CT-MR fusion has been comparatively assessed. Definition of the ground truth target volume has been performed by board certified radiation oncologists after detailed assessment, colleague peer review, collaboration and consensus to be used for actual treatment and comparison purposes.
Results
Target volume definition by use of CT-only imaging and by CT-MR fusion based imaging has been comparatively evaluated in this study for linear accelerator (LINAC)-based radiosurgical management of atypical meningioma. Ground truth target volume defined by the board-certified radiation oncologists after detailed evaluation, collaboration, colleague peer review and consensus has been found to be identical to target determination by use of CT-MR fusion based imaging.
Treatment planning for LINAC-based radiosurgery has been performed by ERGO ++ (CMS, Elekta, UK) radiosurgery planning system. Optimal target coverage and normal tissue sparing has been achieved by using a single 360-degree arc, double 360-degree arcs, or five 180-degree arcs in radiosurgery planning. Synergy (Elekta, UK) LINAC available at our department has been used in delivery of treatment. Delineation of the target volume on planning CT and MR images has been optimized by selecting the appropriate windows and levels for radiosurgery planning. Sagittal and coronal images have been used in addition to the axial planning CT images to achieve accurate contouring of target volume and critical structures. Arc Modulation Optimization Algorithm (AMOA) has been utilized for optimization of target volume coverage and critical organ sparing. Figure 1 shows coronal CT image of a patient with atypical meningioma, and Figure 2 shows the corresponding coronal MR image of the same patient with atypical meningioma.
Figure 1.Coronal CT image of a patient with atypical meningioma
Figure 2.Corresponding coronal MR image of the same patient with atypical meningioma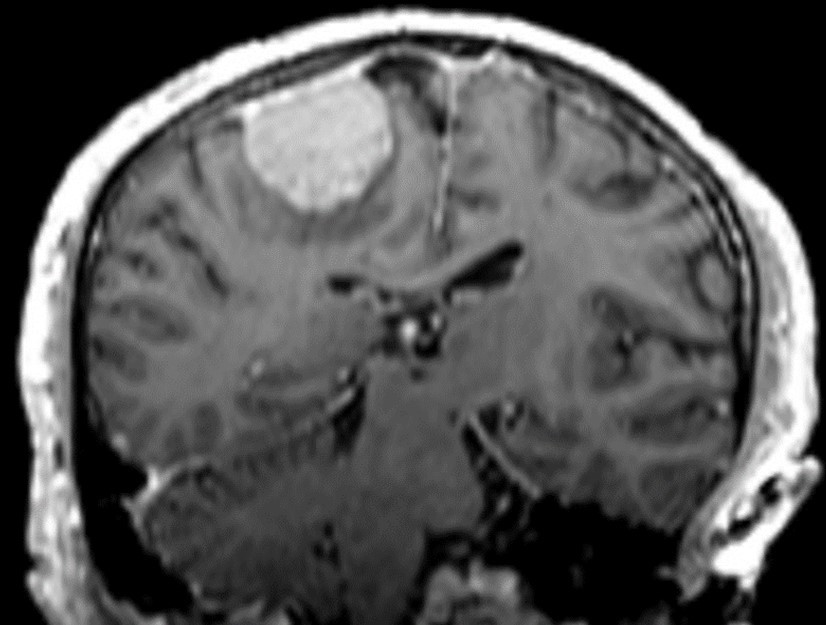
Discussion
Histological subtypes of WHO grade I meningioma are psammomatous meningioma, meningothelial (syncytial) meningioma, transitional (mixed) meningioma, fibroblastic (fibrous) meningioma, secretory meningioma, lymphoplasmacyte-rich meningioma, transitional (mixed) meningioma, microcystic meningioma, and metaplastic meningioma with respect to the WHO classification of Central Nervous System (CNS) tumors6. WHO grade II meningioma histological subtypes as per the WHO classification are atypical meningioma, clear cell meningioma, and chordoid meningioma6. Finally, WHO grade III meningioma histological subtypes are anaplastic (malignant) meningioma, rhabdoid meningioma, and papillary meningioma6.
Benign meningiomas typically follow an indolent disease course with a low risk of recurrence after complete surgical removal. However, atypical or anaplastic meningiomas may follow a more aggressive disease course with predilection for invasion of critical structures and recurrences despite surgical management 7, 8, 9. In this context, RT may serve as an integral component in multimodality management of meningiomas, particularly in the setting of incomplete resection.
There have been substantial advances in the discipline of radiation oncology recently including contemporary treatment strategies such as Image Guided Radiation Therapy (IGRT), Adaptive Radiation Therapy (ART), Intensity Modulated Radiation Therapy (IMRT), Breathing Adapted Radiation Therapy (BART), and stereotactic irradiation with SRS, HFSRT, and SBRT 38, 39, 40, 41, 42, 43, 44.
Radiosurgery has been utilized for management of atypical meningiomas with encouraging outcomes 45, 46, 47, 48, 49, 50, 51. Radiosurgery may be utilized for improved precision in RT delivery by use of stereotactic localization and optimized normal tissue sparing with steeper dose gradients around the target volume. Delineation of target volume for radiosurgery is a critical aspect of management. Excessive toxicity may result from determination of larger target volumes and geopraphical misses may occur when smaller than actual target volumes are determined. Multimodality imaging may add to the accuracy and precision in target contouring. Combined use of fused CT and MR images may supplement each other for accuracy in contouring of target volume for radiosurgery. Utility of multimodality imaging for radiosurgery treatment planning for atypical meningiomas has been poorly addressed in the literature. In this context, our study adds to the literature by reporting improved target definition by incorporation of MRI in radiosurgery treatment planning for atypical meningiomas. Indeed, several other studies have addressed the utility of multimodality imaging for radiosurgery target volume definition 52, 53, 54, 55, 56, 57, 58, 59, 60, 61, 62, 63.
In conclusion, incorporation of MRI into treatment planning for radiosurgery of atypical meningiomas may improve target definition despite the need for further supporting evidence.
References
- 1.Ostrom Q T, Cioffi G, Gittleman H, Patil N, Waite K. (2019) . CBTRUS Statistical Report: Primary Brain and Other Central Nervous System Tumors Diagnosed in the United States in 2012-2016. Neuro Oncol 1-21.
- 2.Claus E B, Bondy M L, Schildkraut J M, Wiemels J L, Wrensch M. (2005) Epidemiology of intracranial meningioma. , Neurosurgery 57, 1088-95.
- 3.Bondy M, Ligon B L. (1996) Epidemiology and etiology of intracranial meningiomas: A review. , J Neurooncol 29, 197-205.
- 4.Pieper D R, Al-Mefty O, Hanada Y, Buechner D. (1999) Hyperostosis associated with meningioma of the cranial base: Secondary changes or tumor invasion. , Neurosurgery 44, 742-6.
- 5.Louis D N, Ohgaki H, Wiestler O D, Cavenee W K, Burger P C. (2007) WHO classification of tumours of the central nervous system.Acta Neuropathol. 114(2), 97-109.
- 6.Bhat A R, Wani M A, Kirmani A R, Ramzan A U. (2014) Histological-subtypes and anatomical location correlated in meningeal brain tumors (meningiomas). , J Neurosci Rural Pract 5, 244-9.
- 7.Shakir S I, Souhami L, Petrecca K, Mansure J J, Singh K. (2018) Prognostic factors for progression in atypical meningioma. , J Neurosurg 19, 1-9.
- 8.Buerki R A, Horbinski C M, Kruser T, Horowitz P M, James C D. (2018) An overview of meningiomas. , Future Oncol 14, 2161-77.
- 9.Rogers L, Barani I, Chamberlain M, Kaley T J, McDermott M. (2015) Meningiomas: Knowledge base, treatment outcomes, and uncertainties. A RANO review. , J Neurosurg 122, 4-23.
- 10.Goldbrunner R, Minniti G, Preusser M, Jenkinson M D, Sallabanda K. (2016) EANO guidelines for the diagnosis and treatment of meningiomas. , Lancet Oncol 17, 383-391.
- 11.Sughrue M E, Kane A J, Shangari G, Rutkowski M J, McDermott M W. (2010) The relevance of simpson grade I and II resection in modern neurosurgical treatment of world health organization grade I meningiomas. , J Neurosurg 113, 1029-35.
- 12.SIMPSON D. (1957) The recurrence of intracranial meningiomas after surgical treatment. J Neurol Neurosurg Psychiatry. 20(1), 22-39.
- 13.DeMonte F, Smith H K, al-Mefty O. (1994) Outcome of aggressive removal of cavernous sinus meningiomas. , J Neurosurg 81, 245-51.
- 14.Larson J J, van Loveren HR, Balko G, Tew JM Jr. (1995) Evidence of meningioma infiltration into cranial nerves: Clinical implications for cavernous sinus meningiomas. , J Neurosurg 83, 596-9.
- 15.Sen C, Hague K. (1997) Meningiomas involving the cavernous sinus: Histological factors affecting the degree of resection. , J Neurosurg 87, 535-43.
- 16.Dufour H, Muracciole X, Métellus P, Régis J, Chinot O. (2001) Long-term tumor control and functional outcome in patients with cavernous sinus meningiomas treated by radiotherapy with or without previous surgery: Is there an alternative to aggressive tumor removal?. , Neurosurgery 48, 285-96.
- 17.Demiral S, Dincoglan F, Sager O, Uysal B, Gamsiz H. (2018) . , Contemporary Management of Meningiomas with Radiosurgery. Int J Radiol Imaging Technol 80(2), 187-90.
- 18.Dincoglan F, Sager O, Demiral S, Gamsiz H, Uysal B. (2019) Fractionated stereotactic radiosurgery for locally recurrent brain metastases after failed stereotactic radiosurgery. , Indian J Cancer 56(2), 151-6.
- 19.Dincoglan F, Sager O, Uysal B, Demiral S, Gamsiz H. (2019) Evaluation of hypofractionated stereotactic radiotherapy (HFSRT) to the resection cavity after surgical resection of brain metastases: A single center experience. , Indian J Cancer 56(3), 202-6.
- 20.Dincoglan F, Sager O, Demiral S, Uysal B, Gamsiz H. (2017) Radiosurgery for recurrent glioblastoma: A review article. , Neurol Disord Therap 1, 1-5.
- 21.Demiral S, Dincoglan F, Sager O, Gamsiz H, Uysal B. (2016) Hypofractionated stereotactic radiotherapy (HFSRT) for who grade I anterior clinoid meningiomas (ACM). , Jpn J Radiol 34(11), 730-737.
- 22.Dincoglan F, Beyzadeoglu M, Sager O, Demiral S, Gamsiz H. (2015) Management of patients with recurrent glioblastoma using hypofractionated stereotactic radiotherapy. , Tumori 101(2), 179-184.
- 23.Gamsiz H, Beyzadeoglu M, Sager O, Demiral S, Dincoglan F. (2015) Evaluation of stereotactic body radiation therapy in the management of adrenal metastases from non-small cell lung cancer. , Tumori 101(1), 98-103.
- 24.Demiral S, Beyzadeoglu M, Sager O, Dincoglan F, Gamsiz H. (2014) Evaluation of linear accelerator (linac)-based stereotactic radiosurgery (srs) for the treatment of craniopharyngiomas. , UHOD - Uluslararasi Hematoloji-Onkoloji Dergisi 24, 123-129.
- 25.Dincoglan F, Sager O, Gamsiz H, Uysal B, Demiral S. (2014) Management of patients with ≥ 4 brain metastases using stereotactic radiosurgery boost after whole brain irradiation. , Tumori 100(3), 302-306.
- 26.Gamsiz H, Beyzadeoglu M, Sager O, Dincoglan F, Demiral S. (2014) Management of pulmonary oligometastases by stereotactic body radiotherapy. , Tumori 100(2), 179-183.
- 27.Sager O, Dincoglan F, Beyzadeoglu M. (2015) Stereotactic radiosurgery of glomus jugulare tumors: Current concepts, recent advances and future perspectives. , CNS Oncol 4(2), 105-114.
- 28.Sager O, Beyzadeoglu M, Dincoglan F, Gamsiz H, Demiral S. (2014) Evaluation of linear accelerator-based stereotactic radiosurgery in the management of glomus jugulare tumors. , Tumori 100(2), 184-188.
- 29.Sager O, Beyzadeoglu M, Dincoglan F, Uysal B, Gamsiz H. (2014) Evaluation of linear accelerator (LINAC)-based stereotactic radiosurgery (SRS) for cerebral cavernous malformations: A 15-year single-center experience. , Ann Saudi Med 34(1), 54-58.
- 30.Demiral S, Beyzadeoglu M, Uysal B, Oysul K, Kahya Y E. (2013) Evaluation of stereotactic body radiotherapy (SBRT) boost in the management of endometrial cancer. , Neoplasma 60(3), 322-327.
- 31.Dincoglan F, Beyzadeoglu M, Sager O, Uysal B, Demiral S. (2013) Evaluation of linear accelerator-based stereotactic radiosurgery in the management of meningiomas: A single center experience. , J BUON 18(3), 717-722.
- 32.Sager O, Beyzadeoglu M, Dincoglan F, Demiral S, Uysal B. (2013) Management of vestibular schwannomas with linear accelerator-based stereotactic radiosurgery: A single center experience. , Tumori 99(5), 617-622.
- 33.Dincoglan F, Sager O, Gamsiz H, Uysal B, Demiral S. (2012) Stereotactic radiosurgery for intracranial tumors: A single center experience. , Gulhane Med J 54(3), 190-198.
- 34.Dincoglan F, Sager O, Gamsiz H, Demiral S, Uysal B. (2012) Management of arteriovenous malformations by stereotactic radiosurgery: A single center experience. UHOD-Uluslararasi Hematoloji-Onkoloji Dergisi. 22, 107-112.
- 35.Dincoglan F, Beyzadeoglu M, Sager O, Oysul K, Sirin S. (2012) Image-guided positioning in intracranial non-invasive stereotactic radiosurgery for the treatment of brain metastasis. , Tumori 98(5), 630-635.
- 36.Surenkok S, Sager O, Dincoglan F, Gamsiz H, Demiral S. (2012) Stereotactic radiosurgery in pituitary adenomas: A single center experience. UHOD-Uluslararasi Hematoloji-Onkoloji Dergisi. 22, 255-260.
- 37.Sirin S, Oysul K, Surenkok S, Sager O, Dincoglan F. (2011) Linear accelerator-based stereotactic radiosurgery in recurrent glioblastoma: A single center experience. , Vojnosanit Pregl 68(11), 961-966.
- 38.Sager O, Beyzadeoglu M, Dincoglan F, Oysul K, Kahya Y E. (2012) Evaluation of active breathing control-moderate deep inspiration breath-hold in definitive non-small cell lung cancer radiotherapy. , Neoplasma 59(3), 333-340.
- 39.Uysal B, Beyzadeoğlu M, Sager O, Dinçoğlan F, Demiral S. (2013) Dosimetric evaluation of intensity modulated radiotherapy and 4-field 3-d conformal radiotherapy in prostate cancer treatment. , Balkan Med J 30(1), 54-57.
- 40.Dincoglan F, Beyzadeoglu M, Sager O, Oysul K, Kahya Y E. (2013) Dosimetric evaluation of critical organs at risk in mastectomized left-sided breast cancer radiotherapy using breath-hold technique. , Tumori 99(1), 76-82.
- 41.Sager O, Beyzadeoglu M, Dincoglan F, Demiral S, Uysal B. (2015) Adaptive splenic radiotherapy for symptomatic splenomegaly management in myeloproliferative disorders. , Tumori 101(1), 84-90.
- 42.Sager O, Dincoglan F, Uysal B, Demiral S, Gamsiz H. (2017) Splenic Irradiation: A Concise Review of the Literature. , J App Hem Bl Tran 1(1), 101.
- 43.Sager O, Dincoglan F, Uysal B, Demiral S, Gamsiz H. (2018) Evaluation of adaptive radiotherapy (ART) by use of replanning the tumor bed boost with repeated computed tomography (CT) simulation after whole breast irradiation (WBI) for breast cancer patients having clinically evident seroma. , Jpn J Radiol 36(6), 401-406.
- 44.Sager O, Dincoglan F, Demiral S, Uysal B, Gamsiz H. (2019) Breathing adapted radiation therapy for leukemia relapse in the breast: A case report. , World J Clin Oncol 10(11), 369-374.
- 45.Acker G, Meinert F, Conti A, Kufeld M, Jelgersma C. (2019) Image-Guided Robotic Radiosurgery for Treatment of Recurrent Grade II and III Meningiomas. A Single-Center Study. World Neurosurg. 131, 96-107.
- 46.Lagman C, Bhatt N S, Lee S J, Bui T T, Chung L K. (2017) Adjuvant radiosurgery versus serial surveillance following subtotal resection of atypical meningioma: A systematic analysis. , World Neurosurg 98, 339-46.
- 47.Zhang M, Ho A L, D’Astous M, Pendharkar A V, Choi C Y. (2016) Cyberknife stereotactic radiosurgery for atypical and malignant meningiomas. , World Neurosurg 91, 574-81.
- 48.Wang W H, Lee C C, Yang H C, Liu K D, Wu H M. (2016) Gamma knife radiosurgery for atypical and anaplastic meningiomas. , World Neurosurg 87, 557-64.
- 49.Aboukais R, Zairi F, Lejeune J P, E Le Rhun, Vermandel M. (2015) Grade 2 meningioma and radiosurgery. , J Neurosurg 122, 1157-62.
- 50.Ding D, Starke R M, Hantzmon J, Yen C P, Williams B J. (2013) The role of radiosurgery in the management of WHO Grade II and III intracranial meningiomas. , Neurosurg Focus 35, 16.
- 51.Choi C Y, Soltys S G, Gibbs I C, Harsh G R, Jackson P S. (2010) Cyberknife stereotactic radiosurgery for treatment of atypical (WHO grade II) cranial meningiomas. , Neurosurgery 67, 1180-8.
- 52.Beyzadeoglu M, Dincoglan F, Sager O, Demiral S. (2020) Evaluation of Target Volume Definition with Multimodality Imaging for Radiosurgery of Intracranial Germ Cell Tumors (GCTs): An Original Article. , Asian Journal of Pharmacy, Nursing and Medical Sciences 08(02), 1-4.
- 53.Dincoglan F, Demiral S, Sager O, Beyzadeoglu M. (2020) Utility of Multimodality Imaging Based Target Volume Definition for Radiosurgery of Trigeminal Neuralgia: An Original Article. , Biomed J Sci & Tech Res 26(2), 19728-32.
- 54.Sager O, Demiral S, Dincoglan F, Beyzadeoglu M. (2020) Target Volume Definition for Stereotactic Radiosurgery (SRS) Of Cerebral Cavernous Malformations (CCMs). , Canc Therapy & Oncol Int J 15(4), 555917.
- 55.Demiral S, Sager O, Dincoglan F, Uysal B, Gamsiz H. (2018) Evaluation of Target Volume Determination for Single Session Stereotactic Radiosurgery (SRS) of Brain Metastases. , Canc Therapy & Oncol Int J 12(5), 555848.
- 56.Sager O, Dincoglan F, Demiral S, Gamsiz H, Uysal B. (2019) Evaluation of the Impact of Magnetic Resonance Imaging (MRI) on Gross Tumor Volume (GTV) Definition for Radiation Treatment Planning (RTP) of Inoperable High Grade Gliomas (HGGs). Concepts in Magnetic Resonance Part A. Article ID. 4282754.
- 57.Sager O, Dincoglan F, Demiral S, Gamsiz H, Uysal B. (2019) Utility of Magnetic Resonance Imaging (Imaging) in Target Volume Definition for Radiosurgery of Acoustic Neuromas. , Int J Cancer Clin Res 6, 119.
- 58.Demiral S, Sager O, Dincoglan F, Beyzadeoglu M. (2019) Assessment of target definition based on Multimodality imaging for radiosurgical Management of glomus jugulare tumors (GJTs). , Cancer Ther Oncol Int J 15(2), 83-86.
- 59.Dincoglan F, Sager O, Demiral S, Beyzadeoglu M. (2019) Multimodality Imaging for Radiosurgical Management of Arteriovenous Malformations. , Asian Journal of Pharmacy, Nursing and Medical 7(1), 7-12.
- 60.Sager O, Dincoglan F, Demiral S, Beyzadeoglu M. (2019) Evaluation of Radiosurgery Target Volume Determination for Meningiomas Based on Computed Tomography (CT) And Magnetic Resonance Imaging (MRI). , Cancer Sci Res Open Access 5(2), 1-4.
- 61.Beyzadeoglu M, Sager O, Dincoglan F, Demiral S. (2019) Evaluation of Target Definition for Stereotactic Reirradiation of Recurrent Glioblastoma. , Arch Can Res 7(1), 3.
Cited by (8)
- 1.Murat Beyzadeoglu, Omer Sager, Ferrat Dincoglan, Selcuk Demiral, Bora Uysal, et al, 2020, Single Fraction Stereotactic Radiosurgery (SRS) versus Fractionated Stereotactic Radiotherapy (FSRT) for Vestibular Schwannoma (VS), Journal of Surgery and Surgical Research, 6(1), 062, 10.17352/2455-2968.000099
- 2.Omer Sager, Ferrat Dincoglan, Selcuk Demiral, Murat Beyzadeoglu, 2021, Radiation Therapy (RT) target determination for irradiation of bone metastases with soft tissue component: Impact of multimodality imaging, Journal of Surgery and Surgical Research, (), 042, 10.17352/2455-2968.000134
- 3.Omer Sager, Murat Beyzadeoglu, Ferrat Dincoglan, Selcuk Demiral, Bora Uysal, et al, 2020, A concise review of irradiation sequelae on the cardiovascular system in pulmonary malignancies, Journal of Surgery and Surgical Research, 6(1), 079, 10.17352/2455-2968.000102
- 4.Omer Sager, Ferrat Dincoglan, Selcuk Demiral, Murat Beyzadeoglu, 2021, Evaluation of changes in tumor volume following upfront chemotherapy for locally advanced Non Small Cell Lung Cancer (NSCLC), Global Journal of Cancer Therapy, (), 031, 10.17352/2581-5407.000039
- 5.Omer Sager, Murat Beyzadeoglu, Ferrat Dincoglan, Selcuk Demiral, Bora Uysal, et al, 2020, Evaluation of critical organ dosimetry with focus on heart exposure in supine versus prone patient positioning for breast irradiation, Journal of Surgery and Surgical Research, 6(1), 087, 10.17352/2455-2968.000104
- 6.Omer Sager, Selcuk Demiral, Ferrat Dincoglan, Murat Beyzadeoglu, 2021, Assessment of posterior fossa target definition by multimodality imaging for patients with medulloblastoma, Journal of Surgery and Surgical Research, (), 037, 10.17352/2455-2968.000133
- 7.Ferrat Dincoglan, Omer Sager, Selcuk Demiral, Murat Beyzadeoglu, 2022, Multimodality imaging based treatment volume definition for recurrent Rhabdomyosarcomas of the head and neck region: An original article, Journal of Surgery and Surgical Research, 8(2), 013, 10.17352/2455-2968.000148
- 8.Selcuk Demira, Ferrat Dincoglan, Omer Sager, Murat Beyzadeoglu, 2021, Treatment volume definition for irradiation of primary lymphoma of the orbit: Utility of multimodality imaging, Journal of Surgery and Surgical Research, (), 057, 10.17352/2455-2968.000138
