Abstract
Tuberculosis involving the liver in the absence of active pulmonary tuberculosis is very rare. The inflammatory pseudotumoral form is an entity difficult to diagnose. We report a case of an inflammatory pseudotumor of the liver due to tuberculosis, who didn’t underwent hepatectomy because of the size of the tumor. The diagnosis of tuberculosis was made on biopsy and Polymerase Chain Reaction (PCR).
Author Contributions
Academic Editor: Florin Graur, Assistant Professor in General Surgery Consultant Surgeon
Checked for plagiarism: Yes
Review by: Single-blind
Copyright © 2018 Sabbah Meriam, et al
 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Competing interests
The authors have declared that no competing interests exist.
Citation:
Introduction
Tuberculosis of the liver, especially thepseudotumorform without active pulmonary tuberculosis, is very uncommon. Most of the cases reported in the literature are in the form of localized mass and are usually misdiagnosed as a primary or secondary liver tumor. Final diagnosis is made after multidisciplinary concertation regarding imaging techniques: ultrasonography (US), computed tomography, magnetic resonance imaging (MRI) associated with pathological examination of percutaneous fine-needle biopsy or resected specimen. We report a case of inflammatory hepatic pseudotumor due to tuberculosis diagnosed by polymerase chain reaction.
Case Report
A 50-year-old man, was referred to our center for abdominal pain that had persisted for 1 month with marked loss of weight. An abdominal ultrasound completed by CT scan revealed a tumor of 15 centimeters of main axis of the right liver associated in contact with the portal vein associated with bilateral pulmonary nodules (Figure 1, Figure 2). Family and personal history for tuberculosis were negative. On admission, there was no fever, the abdomen was soft and non-tender, and there was a painful hepatomegaly without palpable mass. Blood showed anicteric cholestasis. Hydatid serology as well as tuberculin skin tests were negative. Upper and lower digestive endoscopy as well as tumor markers were normal. An ultrasound-guided fine-needle biopsy showednecro-inflammatory changes of the liver parenchyma without any signs of malignancy or specificity. Concerning the pulmonary lesions, there were no proof of active tuberculosis (sputum examination and bronchoalveolar lavage showed no BK). Patient received empiric antibiotherapy (amoxicillin and clavulanic acid) with regression of the pulmonary lesions in the control X Ray.
Figure 1.Coronal CT scan showing the hypodense heterogeneous liver mass in contact with the portal vein and diaphragm
Figure 2.Coronal CT scan showing multiple bilateral pulmonary masses of both lungs associated with centrilobularmicronodules
After a multidisciplinary concertation, the hepatectomy was recused because of the size of lesion, the uncertain nature of the lesion and the small remaining liver in case of surgery. The pathological examination was performed again showing inflammatory pseudotumor of the liver (Figure 3). The Polymerase Chain Reaction (PCR) of the specimen was positive. PCR BK made on liver biopsies molecular profile compatible with a hepatic tuberculosis despite the absence of a granulomatous reaction to histology
Figure 3.Hepatic biopsy showing a marked inflammatory reaction with a polymorphic infiltrate (HEx200)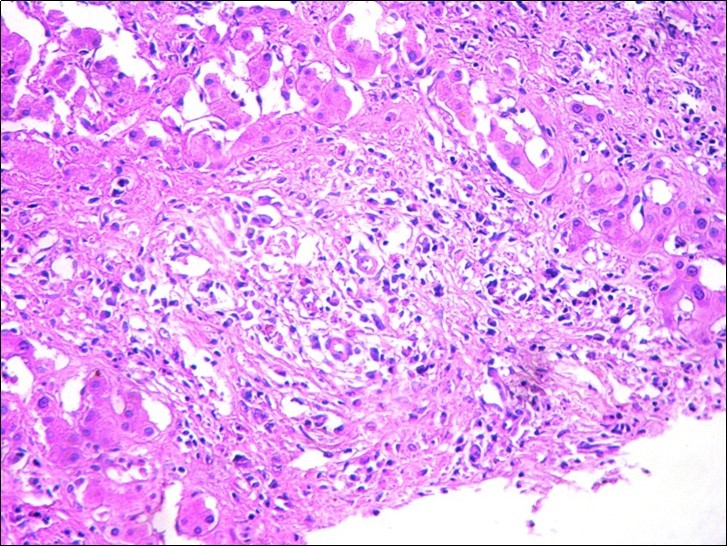
The patient was treated with tuberculostatic drugs (association of isoniazid, ethambutol and rifampicin) with good clinical tolerance. The use of pyrazinamide was recused because of cholestasis. After a 4-months follow-up period, the patient improved his general condition and laboratory tests (regression of the cholestasis). Control abdominal ultrasound showed regression of the tumor (8cm of main axis) at 3 months of treatment.
Discussion and Conclusion
Tuberculosis is a monumental health problem and it remains a healthcare challenge in the developed world owing to immigration from endemic areas, increased prevalence of immunosuppression, and emergence of multidrug- and extensively drug-resistant strains of Mycobacterium tuberculosis 1, 2.
Hepatic tuberculosis is usually disseminated associated with miliary tuberculosis in 80% of cases and primary tuberculosis of liver is uncommon3. Xing and al. 4 published the largest series of 8 cases (682 liver resections between 1988 and 2004).
The clinical presentation is not specific and a high degree of clinical suspicion is required to diagnose the entity. There is often abdominal pain with fever associated with a biological inflammatory syndrome 5. Weight loss, jaundice and hepatic failure are very rare. Imaging can play an important role in the detection, characterization, and management of liver tuberculosis 6. Knowledge of the wide spectrum of CT appearances of abdominal tuberculosis should alert the radiologist to consider its diagnosis, especially among high-risk groups of patients, however, the diagnosis remains histological showing a large epithelioid tumour composed of a giant cells with central caseating necrosis. However,the confirmation of mycobacterium in the tissue samples is rare and the sensitivity of the Ziehl stain coloration onthe tissue remains low (20%) 7 as well as culture of tissuesample for mycobacterium tuberculosis (one third of cases). Therefore, the discovery of liver granulomas, even in the absence of caseous necrosis, is accepted as evidence of tuberculosis) 8. During the last two decades, the use of polymerase chain reaction to directly detect the presence of Mycobacterium tuberculosis is increasing and may improve sensitivity rates. (sensitivity 53-92% andspecificity 70%) 9, 10. This technique was usefull to perform diagnosis in our case report. In most cases, the diagnosis is madeon the resected specimen obtained by laparotomy. Thisreflects the difficulty in establishing a correct diagnosisin the absence of extrahepatic involvement.
For most authors the diagnosis can be reached based either on the presence of hepatic granulomas associated with documented tuberculosis in another organ, particularly the lungs, or when the clinical symptoms and radiological examination evidence regress after starting up antituberculous treatment 11.
The main stay of treatment is antitubercular drug therapy. Chemotherapy with standard anti-tuberculosis drugs remains the cornerstone of treatment. In general, a 6- to 9-months regimen 2 months of isoniazid, rifampin, pyrazinamide, and ethambutol followed by 4-7 months of isoniazid and rifampin) is the recommended treatment forextrapulmonary tuberculosis 12. However in the literature, hepatectomy has been done in some cases13, 14 as a part of effective treatment along with antitubercular therapy or when mistakenly diagnosed as malignancy or for complicated tuberculoma. Surgery is often the only way to obtain a sufficiently largespecimen for pathological study. Laparoscopic examination can also be considered before abrupt surgery. Due to the uncertain pre-operative nature of the lesion, a formal hepatic resection should be performed 15. In our patient, surgery couldn’t be performed because of the size of the tumor and the low remaining hepatic parenchyma in case of surgery.
Cumulative mortality for hepatic tuberculosis ranges between 15% and 42% 16. The factors associated with adverse prognosis are: age < 20 years, miliary tuberculosis, concurrent steroid therapy, AIDS, cachexia, associated cirrhosis and liver failure, and drug induced hepatotoxicity 1. In conclusion, hepatic tuberculosis is uncommon andthe diagnosis of a tubercular lesion of the liver pre-operativelyremains a big challenge that can be helped such as in our case report, by PCR.
References
- 1.Kharrasse G, Soufi M, Berekhli H, Intissar H, Bouziane M et al.(Nov2014) Primary tuberculoma of the liver: a case report and literature review. , Pan Afr Med J; 26, 19-321.
- 2.Walls T, Shingadia D. (2007) The epidemiology of tuberculosis in Europe.ArchDisChild. 92(8), 726-729.
- 3.Tan T C, Cheung A Y, Wan W Y, Chen T C.Tuberculoma of the liver presenting as a hyperechoic mass on ultrasound. , Br J Radiol1997;70: 1293-5.
- 4.Xing X, Li H, W G Liu. (2005) Hepatic segmentectomy for the treatment of hepatic tuberculous psuedo-tumour. Hepatobiliary Pancreat DisInt;. 4, 565-568.
- 5.Cotte E CherkiS, Boibieux A, Baulieux J, Adham M. (2006) Hepatic tuberculosis : a case report of pseudo-tumoral form. , GastroenterolClinBiol; 30, 1317-1320.
- 6.Karaosmanoglu A D, Onur M R, Sahani D V, Tabari A, Karcaaltincaba M.(Jun2016,24) Hepatobiliary Tuberculosis: Imaging Findings. [Epub ahead of print]. , AJR Am J Roentgenol: 1-11.
- 7.Selvakumar N, al. (2002) Efficiency of 0.3% carbolfuchsin in Ziehl- Neelsen staining for detecting acid-fast bacilli. , J ClinMicrobiol 40(8), 3041-3043.
- 8.Kayar Y, Ekinci I, Turkdogan F T, Atay M, Soytas R B et al.(Nov2015) A rare case of isolated macronodular hepatic tuberculosis (Tuberculous) in an immunocompetent patient. , J Pak Med 65(11), 1235-6.
- 9.Soumitesh C, K S Manas, S T Jaya. (2005) Diagnosis of extra -pulmonary tuberculosis by smear, culture and PCR using universal sample processing technology. , J ClinMicrobiol 43(9), 4357-4362.
- 10.Brookes M J, Field M, Dawkins D M, Gearty J, Wilson P. (2006) Massive primary hepatic tuberculoma mimicking hepatocellular carcinoma in an immunocompetent host. , MedGenMed 8(3), 11.
- 11.Wu Z, Wang W L, Zhu Y, Cheng J W, Dong J et al.(Sep2013,25) Diagnosis and treatment of hepatic tuberculosis: report of five cases and review of literature.Int. , J ClinExp 6(9), 845-50.
- 12.Soufi M, Benamer S, Chad B.(Mar2011) Pseudotumoral gallbladder tuberculosis. , Rev Med Interne; 32(3), 32-3.
- 13.Sagara K, Fujiyama S, Umeda T, Sato T, Tashiro S et al.Hepatic granuloma: Report of a case successfully treated by hepatectomy and antituberculous therapy. GastroenterolJpn1984;19: 556-62.
- 14.Sheen-Chen S M, Chen M C, Hu T H, Eng H L, Chen W J et al.Computed tomography and angiography in hepatic tuberculosis mimicking liver tumour. , Int J Tuberc Lung Dis2001;5: 876-8.
