Abstract
Objective:
We compared preoperative data of physical examination, CT and diffusion MRI findings of temporal bone with our intraoperative observations. We investigated the diagnostic efficiency of single-shot spin echo echoplanar diffusion MRI (SS SE EPI) on primary cholesteatoma.
Methods:
33 patients with chronic otitis media who had been admitted to Otolaryngology Department of Haydarpasa Numune Training and Research Hospital between June 2010 and September 2011 were involved in this study. All patients did undergo otoscopic and audiometric examination. After imaging of temporal bone by CT and diffusion MRI, patients were operated and intraoperative observations were recorded. Patients with intraoperatively approved cholesteatoma were defined as group 1 and those without cholesteatoma were defined as group 2. Perioperative and preoperative findings of physical examination, CT and MRI of all patients were compared one by one.
Results:
Positive physical examination findings have been superior to MRI and CT, having a sensitivity of 96%, specifity of 87.5%, positive predictive value of 96% and negative predictive value of 87.5%. In terms of effectiveness of MRI in diagnosing intraoperative cholesteatoma, we had a sensitivity of 80%, specifity of 50%, positive predictive value of 83.3% and negative predictive value of 44.4%. These values are also lower than previously reported results.
Conclusion:
When we had preoperative suspection of cholesteatoma on physical examination and diffusion MRI, in addition with bone tissue erosion on CT, we found that physical examination is superior to MRI and CT in terms of capability of diagnosing the disease.
Author Contributions
Academic Editor: Cuneyt Kucur, Dumlupinar University
Checked for plagiarism: Yes
Review by: Single-blind
Copyright © 2016 Semra Kulekci, et al
 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Competing interests
The authors have declared that no competing interests exist.
Citation:
Introductıon
Cholesteatoma is a cystic lesion characterized by accumulation of desquamated epithelium and keratin layers in the mastoid air spaces and tympanic cavity. It has an erosive effect on bone tissue that caused more damage than any type of chronic otitis media. This destructive effect may lead to hearing loss, intracranial or extracranial complications 1. Being alert about cholesteatoma has a vital importance as we consider the preventive effect of early diagnosis on complications 2.
Clinical findings of cholesteatoma on otoscopic examination are intermittent, purulant otorrhea with an indigenous bad smell, aspiration of epithelium and existance of retraction pockets. Its treatment is surgical. It is not easy to identify the existance of cholesteatoma on otoscopic, otoendoscopic and otomicroscopic examination in previously operated patients. Second-look operations are usually preferred in order to observe residual or recurrent cholesteatoma within 6-18 months postoperatively. There is a developing search on preoperative imaging techniques to demonstrate recurrence of the disease for the purpose of reducing the need for revision surgery 3, 4, 5.
Today, there is a controversy on imaging techniques of cholesteatoma. Computed tomography (CT) and magnetic resonance imaging (MRI) are two preferred techniques in suspicion of cholesteatoma. CT has an advantage on anatomic localization of pathology and bone tissue destruction regarding complication occurance. On the other hand, it is insufficient for distinguishing soft tissues, cholesteatoma, mucoid secretions and granulation formation 6. Altough MRI is superior to CT on evaluating the soft tissue structures, conventional MR sequences are also not reliable for definitive differential diagnosis of cholesteatoma and granulation tissue. Imaging of temporal bone by CT or MRI for identifying postoperative residual cholesteatoma has been studied but unreliable results were reported 7, 8, 9, 10. Effect of diffusion MRI on differentiating cholesteatoma from granulation tissue has been emphasized and advocated in some studies 11, 12, 13. Different techniques of diffusion MRI were compared in terms of evaluating the diagnostic efficiency in detecting cholesteatoma but there is still a controversy. Recent studies have offered late-phase, T1-weighted, contrast-enhanced echoplanar diffusion MRI for diagnosis of cholesteatoma 14, 15, 16, 17. In this study, we compared preoperative data of physical examination, CT and diffusion MRI findings of temporal bone with our intraoperative observations. We investigated the diagnostic efficiency of single-shot spin echo echoplanar diffusion MRI (SS SE EPI) in detecting primary cholesteatoma.
Materıals and Methods
33 patients with chronic otitis media who had been admitted to Otolaryngology Department of Haydarpasa Numune Training and Research Hospital between June 2010 and September 2011 were involved in this study. The protocol was approved by Haydarpasa Numune Training and Research Hospital, Ethics Commitee. All patients had a history of continuous or recurrent otorrhea and hearing loss. On otoscopic examination, among the patients, each one of them should have at least one of signs as perforated tympanic membrane, granulation tissue in the middle ear, polipoid tissue in the external auditory canal, retraction pockets, otorrhea and cholesteatoma. These findings were classified as there is a suspicion of cholesteatoma or not. Patients were divided into 2 groups. Patients with intraoperatively detected cholesteatoma were defined as group 1 and those without cholesteatoma were defined as group 2. All patients did undergo otoscopic and audiometric examination. After imaging of temporal bone by CT and diffusion MRI, patients were operated and intraoperative observations were recorded.
Patients were lied down in supine position during MRI procedure. 1,5T Intera (Philips Medical Systems, The Netherlands) was used for imaging and patients weared head coils during the procedure.
Diffusion weighted images were obtained in axial plan by SS SE EPI. Hitachi-Pronto AR HP spiral scanner was used for tomographic imaging of temporal bone. Slices of 1mm thickness were obtained parallel to orbitomeatal line. Cases which include the destruction of ossicular chain, mastoid bone, scutum, lateral semicircular canal and facial canal, accompanied by density of soft tissue presence on CT images, were gathered in a group named ‘cholesteatoma-suspected’. No anaesthesia and contrast were used during imaging. All scans were evaluated by the same radiologist.
Otomicroscopic findings, hearing levels, CT and diffusion magnetic resonance images of temporal bone were considered preoperatively. Patients were planned to undergo tympanoplasty or mastoidectomy procedures. Written informed consent was obtained from all patients. During surgery, presence or absence of cholesteatoma and its localization were recorded. Perioperative and preoperative findings of physical examination, CT and MRI of all patients were compared one by one.
Statistical analyses were performed with the Statistical Package for the Social Sciences version 10.0, SPSS Inc, Chicago, Illinois, USA. Continuous variables are presented as means±standard deviations, whereas categorical variables are presented as percentages. Inter-group comparisons were made by Student's t-test (for normally distributed data) or the Mann–Whitney U test (for other data). Categorical varieties were compared by the chi-square or Fisher's exact test. The repeated measurements were analyzed with the Wilcoxon signed rank test. A value of P < 0.05 was accepted as statistically significant for all evaluations.
Results
14 male and 19 female patients were included in this study. Mean age was 30,33±15,4 varying between 11-62. Patients with intraoperatively detected cholesteatoma were gathered in group 1 and patients without cholesteatoma composed group 2. Demographic findings of both groups were similar.
Preoperatıve Otomıcroscopıc Fındıngs
Preoperative findings were recorded as cholesteatoma-suspected and cholesteatoma-negative. Cholesteatoma-suspected group included patients with consistant bad-smelling otorrhea, retraction pockets, polipoid tissue in the external ear canal or epithelium that could be aspirated whereas dry perforation of tympanic membrane was classified in cholesteatoma-negative group. 25 (75,7%) of 33 patients were suspected, 8 (24,3%) were not (Table 1).
Table 1. Diagnosis of cholesteatoma by physical examination, CT and MRI| Preoperative findings | Group 1 (n=25) | Group 2 (n=8) | P value |
|---|---|---|---|
| Physical examination (PE)Positive (n) Negative (n) | 24 (96%) 1 (12.5%) | 1 (4%) 7 (87.5%) | 0.000006 |
| Diffusion MRIPositive (n) Negative (n) | 20 (83.3%) 5 (55.6%) | 4 (16.7%) 4 (44.4%) | 0.09 |
| Bone erosion on CTPositive (n) Negative (n) | 18 (78.3%) 7 (70%) | 5 (21.7%) 3 (30%) | 0.61 |
24 of 25 (96%) patients demonstrated intraoperative cholesteatoma in suspected group. Only 1 of 8 12, 5 patients had intraoperative cholesteatoma in negative group (Table 2). Presence of cholesteatoma was statistically significant in suspected group (p=0,000006).
Table 2. PE findings and presence of cholesteatoma| PE Findings | Group 1 (n=25) | Group 2 (n=8) | P value |
|---|---|---|---|
| Adhesion Positive (n) Negative (n) | 19 (95%) 6 (46.2%) | 1 (5%) 7 (53.8%) | 0.003 |
| Retraction Pocket Positive (n) Negative (n) | 16 (100%) 9 (52.9%) | - 8 (47.1%) | 0.002 |
| Otorrhea Positive (n) Negative (n) | 5 (100%) 20 (71.4%) | - 8 (28.6%) | 0.22 |
| Polipoid Tissue Positive (n) Negative (n) | 4 (100%) 21 (72.4%) | - 8 (27.6%) | 0.30 |
| Retraction Positive (n) Negative (n) | 2 (66.7%) 23 (76.7%) | 1 (33.3%) 7 (23.3%) | 0.70 |
| Perforation Positive (n) Negative (n) | 1 (14.3%) 24 (92.3%) | 6 (85.7%) 2 (7.7%) | 0.00005 |
Presence of membrane adhesions (p= 0,003) and retraction pockets (p=0,002) on preoperative examination were considered to be statistically significant in terms of observing intaoperative cholesteatoma. Patients with dry perforations (p=0,00005) did not demonstrate intraoperative cholesteatoma (Figure 1) (Table 1).
Figure 1.Physical examination findings and presence of cholesteatoma
Fındıngs of Preoperatıve Temporal Ct
All preoperative CT scans included soft tissue in tympanic cavity, 23 (69.7%) of them demonstrated bone tissue erosion whereas 10 (30.3%) of them did not (Figure 2) (Table 1).
18 of 23 (78.3) patients who had bone erosions on CT images were observed to have cholesteatoma intraoperatively while the remaining 5 (21.7) were not. Cholesteatoma was detected in 7 of 10 (70%) patients who did not have any sign of bone destruction on CT and remaining 3 (30%) of them were negative (Table 2). No significant result was obtained in terms of impact of tomographic view of bone erosions on indicating presence of intraoperative cholesteatoma (p=0,61)
Figure 2.Soft tissue image causing bone erosion on temporal CT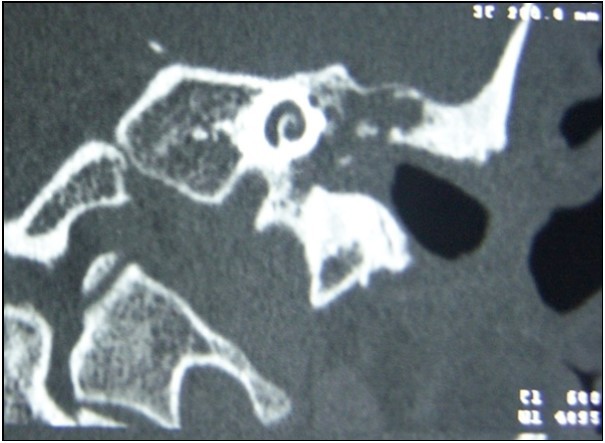
Fındıngs of Preoperatıve Dıffusıon Mrı
High intensity signals on diffusion MRI were considered to be supportive for cholesteatoma (Figure 3). 24 of patients (72.7%) were detected as cholesteatoma positive while 9 of them (27.3%) were negative on diffusion MRI (Table 1).
Figure 3.Diffusion MRI image of cholesteatoma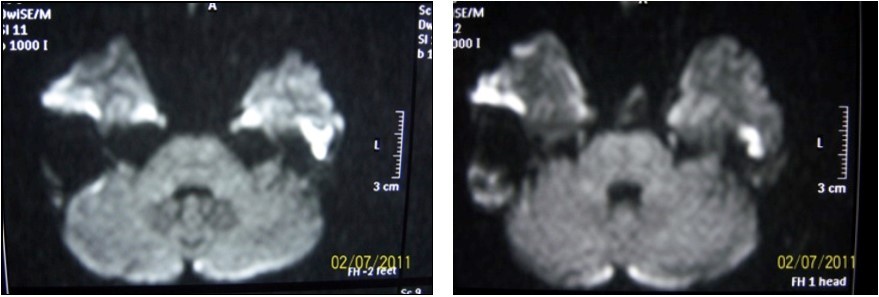
20 of 24 (83.3%) patients who had signs of cholesteatoma on preoperative diffusion MRI were positive intraoperatively while the remaining 4 (16.7%) were negative. 5 of 9 (55.4%) patients who had no evidence of cholesteatoma on MRI were positive intraoperatively while 4 (44.4%) were not (Table 1). There was no significant result obtained in terms of impact of diffusion MRI on detecting intraoperative cholesteatoma (p=0.09). In terms of indicatory strength of positive physical examination findings over presence of intraoperative cholesteatoma, sensitivity was found to be 96% whereas specifity was 87.5%, positive predictive value was 96% and negative predictive value was 87.5%. The area below the curve on ROC curve analysis was calculated as 98% (Table 3) (Figure 4).
Table 3. ROC analysis over diagnostic effect of PE, CT and MRI on cholesteatoma| Area Under Curve | P Value | 95% Confidence İnterval | ||
| Lower Limit | Upper limit | |||
| Diffusion MRI | 0.8 | 0.04 | 0.57 | 1.025 |
| Physical Examination | 0.98 | 0 | 0.93 | 1.028 |
| CT | 0.66 | 0.27 | 0.39 | 0.93 |
Figure 4.ROC curves of PE, CT and diffusion MRI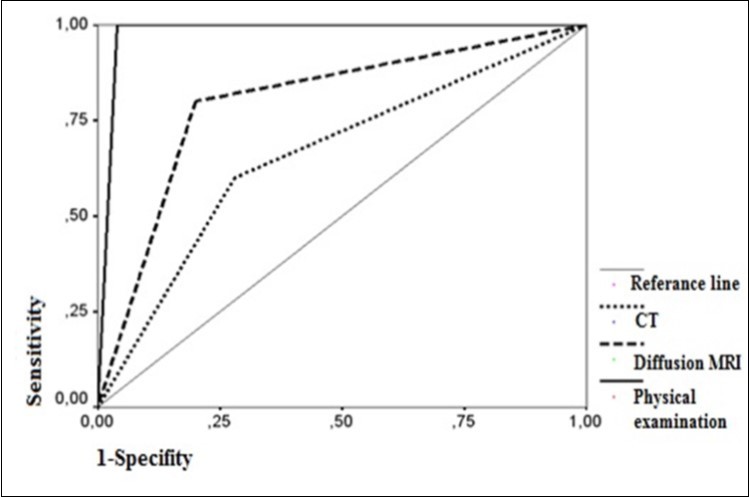
When the impact of positive MRI findings on detecting cholesteatoma was concerned, sensitivity was found to be 80% whereas specifity was 50%, positive predictive value was 83.3% and negative predictive value was 44.4%. The area below the curve on ROC curve analysis was calculated as 80% (Table 3) (Figure 4). When the impact of tomographic view of bone erosion on detecting cholestatoma was investigated, sensitivity was found to be 72% whereas specifity was 37%, positive predictive value was 78% and negative predictive value was 30%. The area below the curve on ROC curve analysis was calculated as 66% (Table 3) (Figure 4).
Type of Surgery Performed
5 of 33 patients did undergo modified radical mastoidectomy, 12 cases were radical mastoidectomy, 9 were tympanomastoidectomy, 3 were revision mastoidectomy and 4 were tympanoplasty.
Localızatıon of Cholesteatoma
When we look through the localization of cholesteatoma, 3 cases were located in antrum, 8 in tympanic cavity and 14 covering both tympanic cavity and antrum. When we compare cholesteatoma positive and negative groups, no significance was obtained in terms of localization of the disease (p=0.27) (Table 4).
Table 4. Localization of cholesteatoma| Localization | Diffusion MRI pozitive (n=20 ) | Diffusion MRI negative(n=5 ) | P value |
|---|---|---|---|
| Antrum (n)Tympanic Cavity (n)Antrum + Tympanic Cavity (n) | 3 (100%) 5 (62.5%) 12 (85.7%) | - 3 (37.5%) 2 (14.3%) | 0.27 |
Discussion
Cholesteatoma occurs as a result of accumulation of desquamated epithelium and keratin layers in cytic lesions of mastoid spaces along temporal
bone and tympanic cavity. It is a unique type of chronic otitis media with progressive destruction. Cholesteatoma is clinically defined on otomicroscopic examination. Its treatment is surgical. A second-look operation is often performed in a period of 6-18 months after primary surgery in order to observe any possible residual or recurrent cholesteatoma 3, 4. Therefore intensive search on preoperative imaging techniques proceeds as it may be an alternative method for open or endoscopic surgical interventions.
Cholesteatoma-suspected group include patients with recurrent bad-smelling otorrhea, presence of
polipoid tissue in the external ear canal, existance of retraction pockets and easily aspirated epithelial tissue. Cholestaetoma-absent group include patients who have dry perforations of tympanic membranes on examination. These findings were compared with intraoperative results. Sensitivity of concordance between positive preoperative findings and intraoperative observations was 96%, whereas its specifity was 87.5%, positive predictive value was 96% and negative predictive value was 87.5% . These results signify the importance of preoperative detailed otomicroscopic examiantion of cholesteatoma-suspected cases.
There is still a controversy on imaging techniques of cholesteatoma. Computed tomography is effective on determinig the localization of pathology and bone tissue destruction but it is still inefficient to distinguish cholesteatoma from mucoid secretions and granulation 6. Nevertheless, soft tissue involvement with adjacent bone tissue destruction is interpreted as a sign of cholesteatoma 18, 19. High-resolution CT provides a useful image for clinicians. It has high sensitivity on defining soft tissue rather than aerated and bony tissues. Postoperative conventional CT images are insufficient to differentiate cholesteatoma from any soft tissue formation. Therefore this technique has a low specifity due to high amount of false-positive results. A high resolution-CT has a negative predictive value of 100% on air cavity images 20.
In our study, 69.7% of cases demonstrated bone tissue destruction on CT whereas in 75.7% of cases we observed intraoperative cholesteatoma. Plouin-Gaudon et al. published an article about pediatric recurrent cholesteatoma and stated that the sensivitiy of CT on demonstrating cholesteatoma had been found 69% whereas its specifity, its negative predictive value and positive predictive value have been found 68%, 55% and 75% respectively 21. When compared with our study, our findings were 72% for sensitivity, 37% for specifity, 78% for positive predictive value and 30% for negative predictive value . These variations results from insufficiency of CT in distinguishing cholesteatoma from soft tissue. In our study, patients with cholesteatoma were more likely to demonstrated bone tissue erosion on CT therefore this finding could be considered as a supportive sign of cholesteatoma existance.
Standard MRI technique is known to be inefficient in detecting cholesteatoma preoperatively 9, 10, 22. However, diffusion MRI has been recently recommended for differentiating cholesteatoma from granulation tissue 11, 12, 13. Low diffusion of cholesteatoma leads to high intensity of signal when compared to granulation, fibrous tissue or mucoid secretions.
In many studies, different techniques of diffusion MRI have been used in order to investigate its effectiveness on differential daignosis of cholesteatoma. All these techniques could be useful and the user could prefer any of them depending on its hardware and software properties. Any possible superiority of one of these methods to another was not discussed in matherial-methods section of our study.
Rapidly obtained images and insensibility to artifacts are main advantages of echoplanar diffusion MRI however, need for high-performance hardware, thick slices, low resolution and magnetic-sensible artifacts seem to be the deficits of this technique. We used SS SE EPI in our study.
Previous studies about echoplanar MRI reported that the sensitivity of this technique had been 77-100%, specifity 66-100%, positive predictive value 84-100% and negative predictive value 75-100% (53-55%). All these studies consisted of revision cases and different MRI techniques had been used. Our study included only 3 previously operated cholesteatoma case out of 33. Two of these 3 patients were preoperatively visualized by diffusion MRI while all of them were diagnosed as cholesteatoma intraoperatively. Echoplanar MRI had been considered as insufficient for detecting cholesteatoma cases which were under 5mm of diameter owing to previously mentioned disadvantages 14, 25, 26, 27, 28, 29. We didn’t measure the size of cholesteatoma intraoperatively and that seems to be a weakness of our study.
We detected the sensitivity level as 80% in terms of capability of diffusion MRI to detect intraoperative cholesteatoma whereas its specifity was 50%, positive predictive value was 83.3% and negative predictive value was 44.4% . In comparison to previous studies, our values were lower. Most of previous articles included lower numbers of patients than our study therefore further studies of larger series are needed in order to investigate the effectiveness of SS SE EPI on detecting cholesteatoma. There was a restrictive condition for us which is to have had limited number of patients in the study.
When we compared our patients with respect to localization of cholesteatoma, there were no difference between diffusion MRI positive and negative groups . Diffusion MRI was found to be ineffective not only for detection of cholesteatoma but also for its localization.
When we concern about preoperative suspection of cholesteatoma on physical examination and diffusion MRI, in addition with bone tissue erosion on CT, we found that physical examination had been superior to MRI or CT in terms of capability of diagnosing the disease.
Conclusıon
►When we compare the findings of physical examination, temporal bone CT and single shot spin echo echoplanar MRI with intraoperative findings of cholesteatoma-suspected patients, we concluded that positive physical examination findings had been superior to MRI and CT, having a sensitivity of 96%, specifity of 87.5%, positive predictive value of 96% and negative predictive value of 87.5%.
►When we evaluate the effect of tomographic finding of bone tissue destruction on diagnosing intraoperative cholesteatoma, we had had a sensitivity of 72%, specifity of 37%, positive predictive value of 78% and negative predictive value 30%. These values were found to be lower than previously reported results.
►In terms of effectiveness of MRI on diagnosing intraoperative cholesteatoma, we had a sensitivity of 80%, specifity of 50%, positive predictive value of 83.3% and negative predictive value of 44.4%. These values are also lower than previously reported results.
►When we concern about preoperative suspection of cholesteatoma on physical examination and diffusion MRI, in addition with bone tissue erosion on CT, we found that physical examination had been superior to MRI or CT in terms of capability of diagnosing the disease.
References
- 1.Akyıldız N. (1998) Kulak Hastalıkları ve Mikrocerrahisi Cilt 1. Ankara: Bilimsel Tıp Yayınevi. 247-472.
- 2.Albers F W. (1999) Complications of otitis media: the importance of early recognition. , AmJ Otol 20, 9-12.
- 4.Gyo K, Sasaki Y, Hinohira Y. (1996) Residue of middle ear cholesteatoma afterintact canal wall tympanoplasty: surgical findings at one year. Ann Otol RhinolLaryngol;105:. 615-19.
- 5.Migirov L, Tal S, Eyal A. (2009) MRI, not CT, to rule out recurrent cholesteatoma and avoid unnecessary second-look mastoidectomy. Isr Med Assoc J;11:. 144-46.
- 6.Chee N W, Tan T Y. (2001) The value of pre-operative high resolution CT scans incholesteatoma surgery. , Singapore Med J; 42, 155-59.
- 7.Tierney P A, Pracy P, SPA Blaney, Bowdler D A. (1999) An assesment of the value of the preoperative computed tomography scans prior to otoendoscopic “second look” in intact canal wall mastoid surgery. , Clin Otolaryngol; 24, 274-276.
- 8.1Wake M, Robinson J M, Witcombe J B, Bazerbachi S, Stansbie J M et al. (1992) Detection of recurrent cholesteatoma by computerized tomography after ‘closed cavity’ mastoid surgery. , J Laryngol Otol 106, 393-395.
- 9.Denoyelle F, Silberman B, Garabedian E N. (1994) Value of magnetic resonance imaging associated with x-ray computed tomography in the screening of residual cholesteatoma after primary surgery [in French].Ann Otolaryngol Chir Cervicofac;. 111, 85-88.
- 10.Vanden Abeele D, Coen E, Parizel P M, Heyning P Van de. (1999) Can MRI replace a second look operation in cholesteatoma surgery ?. , Acta Otolaryngol; 119, 555-561.
- 11.Martin N, Sterkers O, Nahum H. (1990) Chronic inflammatory disease of the middle ear cavities: Gd-DTPA-enhanced MR imaging. , Radiology; 176, 399-405.
- 12.Ayache D, Williams M T, Lejeune D. (2005) Usefulness of delayed postcontrast magnetic resonance imaging in the detection of residual cholesteatoma after canal wall-up tympanoplasty. , Laryngoscope; 155, 607-10.
- 13.Williams M T, Ayache D, Alberti C. (2003) Detection of postoperative residual cholesteatoma with delayed contrast-enhanced MR imaging: initial findings. , Eur Radiol; 13, 169-74.
- 14.Aikele P, Kittner T, Offergeld C, Kaftan H, Huttenbrink K B et al. (2003) Diffusion-weighted MR imaging of cholesteatoma in pediatric and adult patients who have undergone middle ear surgery. , AJR Am J Roentgenol 181, 261-265.
- 15.Fitzek C, Mewes T, Fitzek S, Mentzel H J, Hunsche S et al. (2002) Diffusion-weighted MRI of cholesteatomas of the petrous bone. , J Magn Reson Imaging 15, 636-641.
- 16.Maheshwari S, Mukherji K. (2002) Diffusion-weighted imaging for differentiating recurrent cholesteatoma from granulation tissue after mastoidectomy: case report. AJNR. 23, 847-849.
- 17.Ishii K, Takahashi S, Kobayashi T, Matsumoto K, Ishibashi T. (1991) MR imaging of middle ear cholesteatomas. , J Comput Assist Tomogr 15, 934-936.
- 18.R K Jackler, W P Dillon, R A Schindler. (1984) Computed tomography in supurative ear disease: a correlation of surgical and radiographic findings. Laryngoscope. June;94: 746-52.
- 19.G M O’Donoghue, G J Bates, Anslow P, M P Rothera. (1987) The predictive value of high resolution computed tomography in chronic suppurative otitis ear disease. , Clin Otolaryngol; 12, 89-96.
- 20.Thomassin J M, Braccini F. (1999) Role of imaging and endoscopy in the follow up and management of cholesteatomas operated by closed technique (in French). Rev Laryngol Otol Rhinol (Bord). 120: 75 – 81
- 21.Bossard D Plouin-Gaudon, Fuchsmann C, Ayari-Khalfallah S, Froehlich P. (2010) Diffusion-weighted MR imaging for evaluation of pediatric recurrent cholesteatomas. , Int J Pediatr Otorhinolaryngol. Epub 2009 Nov 3 2010Jan; 74(1), 22-6.
- 22.Kimitsuki T, Suda Y, Kawano H, Tono T, Komune S. (2001) Correlation between MRI findings and secondlook operation in cholesteatoma surgery. , ORL J Otorhinolaryngol Relat Spec 63, 291-293.
- 23.Fitzek C M, Fitzek S, Meves T, Mann W, Stoeter P.Ultrafast MRI examination of cholesteatomas of the petrous bone EurRadiol2000;10(suppl):. 295.
- 24.Toyama C, Leite Cda C, Barauna Filho IS, Brito Neto RV, Bento R F et al.The role of magnetic resonance imaging in the postoperative management of cholesteatomas.BrazJOtorhinolaryngol.2008Sep-Oct;74(5):. 693-6.
- 25.Stasolla A, Magliulo G, Parrotto D, Luppi G, Marini M. (2004) Detection of postoperative relapsing/residual cholesteatomas with diffusion-weighted echo-planar magnetic resonance imaging. , Otol Neurotol; 25(6), 879-84.
- 26.Venail F, Bonafe A, Poirrier V. (2008) Comparison of echo-planar diffusion weighted imaging and delayed postcontrast T1 weighted MR imaging for detection of residual cholesteatoma. , AJNR Am J Neuroradiol; 29, 1363-68.
- 27.B De Foer, Vercruysee J-P, Pouillon M. (2007) Value of high-resolution computed tomography and magnetic resonance imaging in the detection of residual cholesteatomas in primary bony obliterated mastoids. , Am J Otolaryngol; 28, 230-34.
