Abstract
Extant epidemiological and social diagnosis information shows an alarming upsurge in the prevalence of overweight and obesity over the last decade in developing countries including Ghana. Despite literature on the dangers and associated risk factors of these two health related constructs is well-written and documented, there seems to be a distinct knowledge gap on cultural influences that may trigger the onset of overweight and obesity, and related comorbidities. This review paper provides a general overview on overweight and obesity, and presents a supportive evidence of their rising prevalence as well as associated overall implications on public health in Ghana. Additionally, the paper explores how indigenous cultural perceptions, beliefs and norms impact on dietary and physical activity behaviours of the people. Based on available evidence, the complementary role of behaviour modification towards the management of overweight and obesity is suggested. The PEN-3 model as an appropriate cultural framework is proposed for future empirical investigations. This would afford programme planners to assess how to design culturally underpinned appropriate intervention programmes that would positively influence long term behavioural practices of the local people.
Author Contributions
Academic Editor: Jinbo He, University of Macau, China.
Checked for plagiarism: Yes
Review by: Single-blind
Copyright © 2018 Hagan Jnr., John Elvis, et al.
 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Competing interests
The authors have declared that no competing interests exist.
Citation:
Introduction
Recent global statistics from the World Health Organization (WHO) reveal that over 1.9 billion adults aged 18 years and older are overweight both developed and developing countries, of which 300 million of them are obese 1, 2. The WHO reiterated that by 2015, 2.3 billion adults were likely to be overweight and a subsequent 700 million adults could be obese 1. The current trends suggest that issues of overweight and obesity have become a serious public health concern in these countries, with over 115 million people affected with overweight and obesity health related problems 3, 4. According to researchers, there is a significant upsurge in the incidence of overweight and obesity in low-income countries with a double burden of the co-existence of both communicable and chronic non-communicable diseases 3, 4.
Ghana, like other sub-Saharan countries is not immune to the menace of overweight and obesity epidemic, despite the persistent problem of undernutrition in many parts of the continent 3, 5. According to Ziraba et al. 6, the prevalence of overweight and obesity increased by almost a third in sub-Saharan Africa, especially among women and people living in urban populaces. This growing epidemic is not only associated with adults but also among children and adolescents. Research evidence has recounted a rising prevalence of childhood overweight and obesity in sub-Saharan Africa countries 1, 2, 7, 8. For instance, the number of children who are overweight or obese has nearly doubled from 5.4 million in 1990 to 10.6 million in 2014. West Africa alone has a reported prevalence of overweight and obesity in urban dwellers doubled (increased by 114%) between 1995 and 2005 9. To date, the top five countries with the highest prevalence of overweight and obesity are Seychelles (73.8 %), Lesotho (70.8 %), South Africa (68.5 %), Mauritania (56.8 %), and Mauritius (53.5 %) 3. Although Ghana is not rated among countries with the highest prevalence rates in overweight and obesity conditions, these health indicators have been recognized as increasing public health problem that could exacerbate significantly on national resources 10, 11. Available scholarly information shows that in many developing countries like sub-Saharan Africa (Ghana inclusive), the risk of chronic diseases would equate the burden of acute infectious diseases in the near future due to the high prevalence of overweight and obesity 12. For example, nutritional transition characterized by the sudden change from diets of high nutritional value to those of poor quality and sedentary lifestyle may heighten the prevalence and incidence of overweight and obesity related sequels such as hypertension, diabetes, strokes, cancers, heart attacks, and other chronic non-communicable diseases 12, 13. Hence, the health and socioeconomic implications of obesity in the sub-Saharan region cannot be underestimated 14, 15. The WHO has warned and predicted that between 2025-2030, there could be an overwhelming mortality rates due to the prevalence of ischaemic heart disease in the African region and that there could be the largest increase in the prevalence of diabetes mellitus in many developing countries 1, 2, 7, 16, 17.
As at 2001, cardiovascular diseases (CVDs) were regarded as the number one cause of death worldwide with eight percent of the burden occurring in developing countries. A 2017 report by the World Health Organization (WHO) indicates that CVD remains the number one cause of death globally, with more people dying annually from CVDs than from any other cause worldwide. This WHO report reiterates that over three quarters of CVD deaths take place in low- and middle-income countries 18. In sub-Saharan Africa, the pattern of CVD-related morbidity and mortality has been rather out of the ordinary, with the magnitude and trends of CVD deaths remain unimaginable19. Considering that many developing countries are still grappling with the problems of infectious diseases and malnutrition 20, the emergence of non-communicable diseases and various types of cancer, contributes to a double burden of disease and a high incidence of morbidity and mortality on the continent 21. Consequently, twice as many deaths due to CVDs attributed to risk factors such as hypertension and obesity are normally recorded in sub-Saharan Africa where factors such as high blood pressure, high cholesterol, physical inactivity, alcohol use, and low vegetable and fruit consumption are regarded as the top risk factors for cardiovascular disease 1, 2, 7, 21.
There seems to be a dearth of social and epidemiological information on specific evidence in sub-Saharan African countries on the estimation of overweight and those who are obese. Given the high prevalence of overweight and obesity related health problems, it would be worthwhile to chart the current trends of overweight and obesity using Ghana as a case study. This information could be relevant for government and private agencies, and policy makers toward setting priorities and for designing behavioural interventions to curb the emergence of this hider-headed disease 3. Therefore, this review paper gives an overview on overweight and obesity, and presents a supportive evidence of their rising prevalence as well as associated overall implications on public health in Ghana. Additionally, the article explores how indigenous cultural perceptions, beliefs and norms impact on dietary and physical activity behaviours of the people. Based on available evidence, the complementary role of behaviour modification towards the management of overweight and obesity is suggested.
Evidence of Overweight and Obesity in Ghana
The prevalence of overweight and obesity varies greatly from country to country, and it is dependent on the criteria used for the definition of the problem. Overweight and obesity are conditions of excess body fat. The WHO defines weight status according to body mass index (BMI), the ratio of weight (in kilograms) divided by height (in metres squared). A BMI of 20 to 25.9 defines normal weight, 25 to 29.9 indicates overweight and equal to or greater than 30 defines obesity 22.
The prevalence of obesity in 46 African countries according to recent statistics from WHO Global InfoBase indicates that Ghana is ranked at the 10th and 26th positions respectively, with specific overweight prevalence figures of 35.6% and 32.5% among men and women. From obesity range of 0 to 21.3%, Ghana is rated at the 11th position, with a prevalence rate of 4.8% for men. For women’s range of 0 to 43.2%, Ghana is ranked in the 26th position, with a prevalence rate of 5.9% 3. Similarly, a transnational study involving urban women in 24 African countries between 1991 and 2014 on the prevalenceand time trends in overweight and obesity reveals that in Ghana,overweight has almost doubled (p=0.001) while obesity has tripled(p=0.001) between 1993 and 2014 23.
In a current meta-analysis on the overweight and obesity epidemic in Ghana which entailed an analysis of forty-three (43) studies involving a total population of 48,966 sampled across all the ten (10) regions, 4 in 10 of Ghanaian adults are reported either overweight or obese, with the national prevalence (overweight vs obesity) projected at 25.4% (95% CI 22.2–28.7%) and 17.1% (95% CI = 14.7–19.5%) respectively 24.Theprevalence of overweight (27.8% vs 21.8%) and obesity (21.9% vs 6.0%) are noted to be higher in women compared to men. A longitudinal evidence suggest a higher prevalence of overweight and obesity across different studies, with the most recent years (2007 to 2016) compared to past decade (1998-2006) showing a rising trend of obesity in Ghana 24. There seems to be a regional disparity in the country, with a higher prevalence recorded in the more urbanized regions of higher income compared to the less urbanized regions with lesser income levels. For example, in 2014, Greater Accra region (Ghana’s capital) recorded the highest obesity rates of 28.5%, followed by Ashanti Region (16.7%) and Eastern Region (16.5%) whereas the lowest rates of 3.7% were noted in Northern Region among women aged 15-49 years. Similar trends were noted for overweight, with Greater Accra Region recording rates of 28.8%, closely followed by Ashanti Region (28.7%), Brong Ahafo Region (28.3%) and Northern Region being the least with 8.7%. The Upper West Region figures in the same survey were 15.6% for overweight and 5.1% for obesity 25. The latest 2014 Ghana Demographic and Health survey (GDHS) report indicates that the proportion of overweight/obesity among Ghanaian women has increased considerably, from 30% in 2008 to 40% in 2014. The 2014 GDHS report further illustrates that overall, the prevalence of overweight/obesity among men is strikingly lower than the prevalence among women (16% versus 40%, Ghana Statistical Service GSS, Ghana Health Service GHS, 25). Consequently, a crude obesity prevalence of 10.9% in 2014 was estimated by WHO for Ghana, with females having a prevalence of 16.8% more than triple that of males ((4.9%, WHO, 26).
There is also strong evidence from studies that adult overweight and/ or obesity is traceable to childhood roots and that overweight/obese children are more likely than their non-overweight / obese counterparts to grow into obese adults 27, 28. Regarding children’s current statistics of this public health problem, a study involving 3089 children (9–15 years) recruited in Accra and Kumasi, two big cities in Ghana, revealed that 17% of the children were overweight or obese. Children who reported lower participation (< 3 times/week) in sports activity were 44% more likely to be overweight or obese (AOR = 1.44; 95% CI: 1.07, 1.94, 29). Another study which assessed the correlates of obesity among Junior High School Children in the Accra Metropolis indicated that the overall prevalence of obesity for the study cohort was 26.5% 30. Mohammed and Vuvor 31 examining 270 sampled basic school students, found overall prevalence of obesity to be 10.9% among the children, with a higher prevalence among girls (15.0%) than in boys (7.2%). A higher body fat composition was noted among girls aged between 10 –12 years whereas boys aged between 8 – 10 years showed higher body fat stores. Similar to these findings, a recent transnational cross sectional study conducted in 2014 to evaluate the prevalence of underweight, overweight and obesity as well as associated risk factors among school going children in seven African countries found unadjusted rates of being overweight ranged from 8.7% (Ghana) to 31.4% (Egypt). A higher overweight prevalence among females for every age group in five of the countries, except for Egypt and Malawi were reported. Taken together, being overweight was more prevalent among younger (≤12) children and decreased with age 32.
Likewise, other studies among junior high school students aged between 5 to 20 years in the Kumasi Metropolis and Northern Region of Ghana, reported prevalence figures of 12.20% , 0.80% and 17.4% for overweight and obesity respectively 33, 34. According to Lobstein et al. 35 childhood obesity is increasing in both developed and developing countries with increased risks of developing co-morbidities.
Ample evidence from findings of studies conducted in the past 5 years in Ghana reveals that the prevalence of overweight and obesity among both adults and children is soaring and is therefore regarded as an epidemic with public health implications because of the corresponding rising prevalence of diabetes, hypertension and other non-communicable diseases. Ayisi-Addo 36 contends that the rising trend for overweight and obesity and the associated diseases in Ghana was likely to worsen in the future, given the influx of high energy dense foods on the Ghanaian market, coupled with the huge change in dietary and physical activity pattern due to improved socio-economic conditions and other prevailing global factors.
Cultural Influences on Overweight and Obesity
The etiology of overweight and obesity is well documented and reviewed by many scholars 37, however, one paradigm that seems complicated, often overlooked and not entirely well appreciated, and understood is the cultural influences surrounding overweight and obesity 38. Cultural influences suggest that patterns of experiences (behaviours) originate from diverse shared norms, social behaviours, and prescribed societal values 39, 40. These diverse cultural behaviours and beliefs are often learned from childhood, deeply held, and are rarely questioned when growing up and later questioned are passed on to the next generation of offspring. The local belief systems also impact on behaviours such as food intake and physical activity, even though the attributed cultural features are not well described and precisely measured 37. According to WHO 37, culture should be seen as a stronger indicator of food preference alongside other social conventions, religious observances, social status assigned to certain foods, and household influences. From anecdotal evidence, high energy dense foods are usually preserved and served during unique family celebrations and reunions. Many people in indigenous societies like Ghana inadvertently cherish food not much for its nutritional content but rather meals that would strengthen relationships between people and build certain social class. These preferences are mostly exhibited during traditional and / or religious festivities as well as other social occasions (e.g., birthday and marriage celebrations). Consequently, culturally held perceptions, values and traditions may therefore mediate the influence of overweight and obesity 37. These influences perhaps have accounted for the high overweight and obesity prevalence recorded in some sub-Saharan nations 3, 4, 12. Therefore, health behaviours are modified through one’s routine way of life and may serve as a mirror for perceiving and interpreting body image and physique related experiences 41, 42, 43.
In Ghana, like many sub-Saharan countries, the concepts of overweight and obesity are connected with wealth (evidence of good living), beauty, good health, respect and associated with happiness comparative to the western perspective which is usually linked with the onset of illness 44, 45, 46, 47, 48, 49. Hence, derogatory remarks are sometimes made to reflect an individual’s thinness 38. Overweight and obese women are often seen as gorgeous and easily attracted by men due to their curvy body shape 37, 50. Likewise, women usually prefer men who are tall and well-built in stature. African men usually show more preference for overweight over thin women 44. For most males, the ideal body is often connected to robustness or fatness (i.e., large body structure and muscularity) but not necessarily associated with flabbiness 51, 52. Across some traditional groups in Ghana and perhaps other geographical regions (e.g., Nigeria) in the sub-Saharan region, both early and late adolescent girls are prepared for future marriages by special fattening homes, where high energy dense meals (e.g., meat, fried foods) are regularly served for these young women 53, 54, 55, 56, 57. Sequel to this, weight gain after marriage is an evidence that husbands are good providers and caring well of their wives. Alternatively, fat husbands are perceived as being well-fed by their wives who are seen as good cooks and wives, an epitome of good social status and subsequent societal approval 48, 49, 51. Therefore, losing weight is mostly received with social scorn and often associated with physical deterioration as a result of not being well managed 55. Additional to the aforementioned explanations, some foods with so much preservatives and additives (e.g., can, tin, packaged foods i.e. fish meat butter margarine cheese and diets which contain high proportions of sugar are perceived to be from the western world ‘‘whites’’ and have generally been accepted and easily patronized by the local people despite their high prizes. Ironically, the use of local vegetables, legumes and fruits noted for their high fibre content have been abandoned and rather favoured food from the ‘‘West’’ because they are perceived as poor people’s food and are mostly turned to for survival 49. This nutritional transition and other cultural norms may have also accelerated the prevalence of overweight and obesity in the sub-region and serve as a major obstacle towards successful implementation of any intervention programme 48, 49, 58. Therefore, more research is required to probe into context specific interventions that may offer deeper empirical meanings to food consumption, especially those imported from industrialized countries.
The notion of participating in regular physical activity or exercise during leisure time or for recreation is not well understood by many people in developing societies like Ghana. There are some obvious cultural and religious precursors inherent in non-participation in physical activity. For example, people living predominantly in rural and semi-urban areas are primarily more concerned about energy conservation through eaten foods than energy expenditure in order to preserve family food stock 37. Some religious practices and traditions may also have a pivotal impact on their members’ physical activity behaviours 59. Ghanaians with strong religious beliefs (e.g., prayer) may stay away from physical activity and /or exercise on the assumption that their health is controlled by a supreme being (e.g., God, Allah or deity) and their future is out of their control. Such people may not see the essence in taking preventive health measures like physical activity or exercise 60.
According to Caperchione, Kolt, and Mummery 59, sex appropriateness could be a potential barrier to physical activity behaviour, especially for women that empirical evidence has proven to be at a higher risk of overweight and obesity co-morbidities. Some women with specific religious orientation (e.g., Muslim and some Christian denominations) are discouraged from physical activity or exercise engagements to avoid exposing their curvy body in the attire they wear to men 61, 62. Similarly, a commonly held traditional norm in Ghana and perhaps many indigenous societies is that women are often expected to spend their time mostly at home, caring for the immediate family and maintaining their homes 61, 63. This historical role orientation may discourage many women from engaging in physical activity or exercise behaviour of any kind. These inhibiting culturally underpinned sedentary behaviours may have a strong influence on weight gain and the risk of CVDs later in life.
Consequences of Overweight and Obesity
According to WHO 37, the overall consequences of overweight and obesity are numerous and diverse, ranging from heightened risk of premature death to a number of non-fatal but debilitating grievances that have serious implications on one’s quality of life. Various reports from WHO on diet, nutrition and the prevention of chronic diseases have earmarked overweight and obesity as a priority on their public health programme due to the preventable risk associated with varied non communicable diseases (NCDs) 22, 37. The resultant global strategy on diet, physical activity and health has suggested that nearly 66% of deaths from NCDs happen in low-income countries like Ghana. This figure is estimated to rise in the near future if attempts are not made to curb this rising trend. The adverse health implications of overweight and obesity are to a greater or lesser extent triggered by body weight, the location of body fat, the magnitude of weight gained during adulthood as well as sedentary behaviour 64.
Over the past two decades, there is research evidence that has shown a rising trend in prevalence rates of chronic diseases such as hypertension, strokes and diabetes in Ghana 65. Major reasons of death have changed from merely communicable diseases to a blend of communicable and chronic non-communicable diseases. For instance, cardiovascular diseases increased from being the seventh and tenth reason for death recorded in 1953 and 1966, to becoming the number one cause of death in 1991 and 2001 respectively 66. The Ghana Demographic and Health Survey (GDHS, 25, 67, 68) show that the four notable health conditions (i.e., stroke, hypertension, diabetes and cancer) have been listed among the top ten causes of death per each regional health facility in the country. Epidemiological studies on hypertension further revealed that prevalence within the Ghana civil service and other urban workplaces surpassed rates among the urban and semi-urban poor residents 69. Addo and associates reported hypertension and stroke rates to be higher in men, although hypertension was the major cause of maternal deaths in the premier national hospital between the 1980s and 1990s 70 and is the current leading cause of maternal deaths nationally 71. These chronic diseases affect women and men differently, although women represent the higher-risk group for overweight and obesity 44, 72.
To date enough research evidence has shown that overweight and obesity increase the risk of CVDs and associated risk factors such as hypertension, stroke, diabetes, and hypercholesterolemia in some African countries 73, 74. The rising incidence of CVDs runs parallel with the upsurge of overweight and obesity in sub-Saharan Africa 3. These circumstances compromise the quality of life among nationals due to many incapacitations and deaths. Overweight and obesity conditions pose physical challenges and other experiences ranging from minor physical ailments to severe physical disabilities. Aside the complications listed above, some of the non-fatal but negative associated health problems include chronic musculoskeletal, respiratory, skin problems, and infertility 37. These physical challenges have psychological implications (i.e., coping with pain and its management as well as dealing with disrupted lives and identities) which pose enormous burden on mobility and productivity 75. Other significant negative effects on the overall well-being of overweight and obese persons include psychosocial problems like low self-esteem, anxiety, social dysfunction, depression, and moodiness 76, 77.
According to some local researchers, the growing burden of CVDs is happening at a time when infectious diseases are still high, putting enormous challenge on the already burdened and under-resourced healthcare systems in the Ghana and many sub-Saharan African societies 3, 65, 75, 78 . Given the sudden nutritional transition and sedentary lifestyle among other precursors of the growing population in Ghana and other sub-Saharan Africa 3, 65, 75, the prevalence of overweight and obesity and its associated comorbidities such as stoke, hypertension, diabetes could worsen the current public health situation further if immediate steps are not taken to address this health problem 79.
Behaviour Modification
To date, guidelines for managing overweight and obesity are well written and documented 22, 37. However, one area that has received limited attention and not well understood in the management of this public health problem is the impact of culture.
Traditional and other cultural factors influence the dietary intake based on food choices, and physical activity behaviour among most Ghanaians and other nationals from sub-Saharan Africa because local inhabitants are dispersed along a wide range of ethnic backgrounds with a vast array of cultural and geographical experiences. Consequently, dietary habits, food choices, cooking methods, and physical activity behaviour have likewise evolved from long standing histories and traditions 80. Unfortunately, nutritional related attitudes and behaviours that were once customarily preserved and were primarily influenced by natives’ cultural and psychosocial backgrounds 81, 82 have entirely shifted toward more westernized approach due to urbanization related issues 41. Consequently, several aspects of food (e.g., locally produced coarse grains like millet, sorghum, and leafy vegetables rich in dietary fibre, lean meat, smoked fish) purchased for most homes, its preparation and consumption that were culturally determined, and consciously or unconsciously used to uphold traditions and group identity 83, have suddenly changed to fast processed foods (e.g., soft drinks, cooking oils, dairy products, and flour- and fat based snacks) with high energy dense or saturated fat and sugar 78. Therefore, behavioural principles needed for the management of overweight and obesity should re-consider cultural behaviours associated to body weight (i.e., physical activity and diet behaviour) that should be relearned or modified 84. There ought to be an urgent need for dietary changes at the individual, family, and community levels to traditional diets high in locally produced coarse grains like millet, sorghum, and leafy vegetables endowed with dietary fibre, lean meat, smoked fish 78. Another cultural sensitive approach to weight loss management programme is adapting physical activity times to accommodate, for example, prayer times of religious persons (e.g., Muslims and Christians). For instance, many religious Muslim women would prefer working in an enclosed environment that would prevent men from looking at their curved vital statistics while performing physical activities due to their religious beliefs than working from an open area. Such approach portrays an application of cultural competence towards weight loss management 85.
Although physical activity and dietary modification for the prevention of chronic diseases may pose a serious challenge due to immediate compelling issues of daily living among the local population , food purchasing, preparation, nutritional related attitudes and exercise behaviours may require great efforts to change 81. To Lang & Froelicher 86, attaining sustained weight loss means that individuals should learn specific skills to foster a long-term change in eating behaviour and increased energy expenditure. According to these authors, most beneficial behavioural modification requires planning and self-monitoring. Lang & Froelicher suggested that individuals should learn how to plan their dietary intake and physical activity programmes in advance and then compile records on their physical activity and dietary behaviours. This self-monitoring approach facilitates lasting behavioural change, and affords professionals to evaluate the individuals’ progress and make useful suggestions toward their weight loss management goals.
Lang & Froelicher 86 outlined specific strategies that individuals could employed to help overcome obstacles to compliance with regular physical activity and/ or dietary modification. Below are the briefly explained under listed strategies that have been recommended for effectiveness toward a weight loss management programme:
Self-monitoring:
Using a carefully well written down dietary and physical activity behaviour diary provides general awareness of one’s personal commitment to a hitherto unrecognized behaviour to the fore for modification.
Stress Management:
Life stressors can generate dysfunctional eating behaviours. Coping skills such as meditation, mental rehearsal and relaxation techniques could be learned to help minimize stress.
Stimulus Control:
Individuals need to recognize stimuli and real life situations that may trigger incidental eating. Modification strategies include adjusting to careful purchasing of healthy foods, strategically avoiding the storage of high energy dense foods in the house, restricting the times and places of eating, and deliberately shunning situations that elicit overeating (e.g., social gatherings like funerals, parties, outdooring ceremonies).
Problem Solving:
Individuals employ in self-correction of problem areas related to their eating (e.g., avoid eating late and immediately going to bed at night) and physical activity (e.g., making training clothes easily accessible, i.e., putting them next to one’s sleeping pillow). The routine could be to identify the problem, choose solution, plan, implement, and evaluate the outcome.
Contingency Management:
Individuals taking rewards for behaviour modification. Verbal as well as tangible rewards can be useful, coming from self and significant others (e.g., family, health care professionals).
Cognitive Restructuring:
Individuals modifying or altering negative thoughts, mentally avoiding unrealistic goals, and changing inaccurate beliefs and perceptions about weight loss and making plans in advance for relapses or setbacks.
Social Support:
Individuals aligning with family members, friends, colleagues, or health care professionals to maintain their motivation and offer positive reinforcement during their weight loss management schedule.
Relapse Prevention Training (RPT):
Different specific techniques to overcome setbacks and to cope with problems are learnt through the assistance of health care professionals.
Practical Implications for Interventions using the PEN-3 Model:
Given that the individual, extended family, neighborhood or community are mutually and culturally connected to each other in Ghana and other sub-Saharan African societies, designing specific health intervention programmes should be holistic, multi-cultural and faceted. For example, women could be targeted because traditionally they are usually perceived to be concerned with their family’s health, are mostly responsible for food preparation, setting standards for healthful or unhealthful eating practices, and providing access to other family members 87. Likewise, men are perceived to be responsible for activities that elicit more physical exertion, hence they could be targeted to initiate and sustain family’s engagement in physical activity or exercise. Since Africans are extremely religious and its practices are very pervasive and play a central role in the Ghanaian society, leaders of religious entities (e.g., Christians, Muslims) could help implement health education and promotion programmes on physical activity, dietary modification and other healthy lifestyle behaviours.
Policy interventions developed should explore strategies including laws and regulations that would be stringent on misleading advertisements on foods, drinks and beverages provided by multi-national food industries by blocking distribution channels in the country before getting to the consumer. Individuals need to learn how to differentiate between reliable and unreliable nutritional information (e.g., food labels) and understand how the media could influence their decision making on food preferences and the implication on their overall health 80. Taxation and pricing standards that could promote or limit consumption of certain foods should be established by stakeholders. Neighborhood environment could be modified by programme and/ or intervention planners to also encourage physical activity or exercise (e.g., building bicycle and pedestrian walkways and recreational parks).
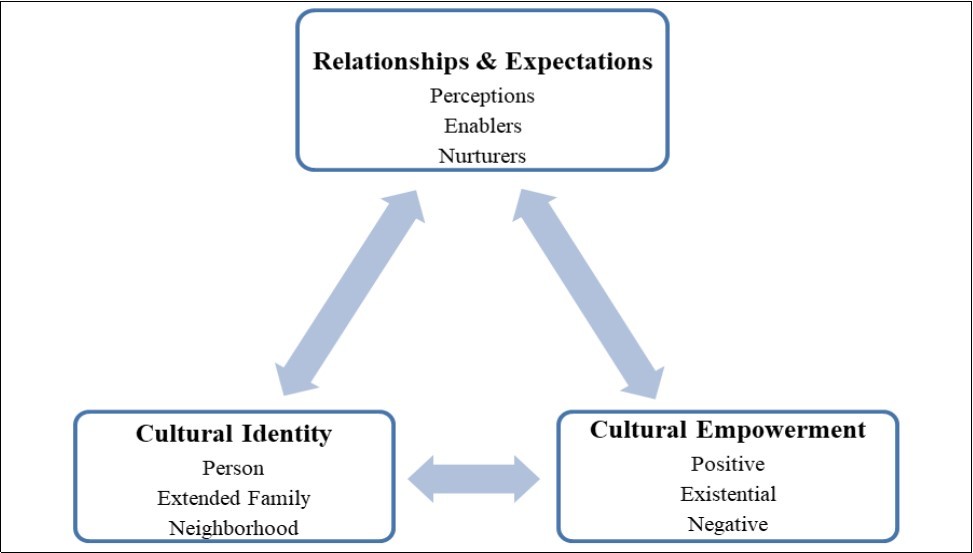
One cultural intervention model that could be drawn upon to help efforts toward implementing sensitive strategies for eating and physical activity behaviour across local communities from a cultural perspective is the PEN-3 model 41, 80. This model as a tool kit allows researchers and health related professionals to evaluate diverse factors that determine the health challenges confronting local people through multiple entry points. Using this model, programme planners are empowered to develop comprehensive health education and promotion programmes through prevention and intervention efforts to mitigate their health challenges within local communities. The model evaluates health beliefs, decisions and behaviours within specific socio-cultural context through distinct attributes so that effective locally underpinned interventions can be designed, applied and appraised 41, 80, 88, 89. According to BeLue et al. 41, the model emphasizes the significance of integrating the local people, community and their culture in finding sustainable interventions that would elicit positive long-term behaviour changes. The PEN-3 model consists of three intertwined and interdependent components; relationships and expectations, cultural empowerment, and cultural identity. Each component comprises three sub-constructs. The relationships and expectations, and cultural empowerment components function as the assessment module for targeted intervention whereas the domain, cultural identity, defines the entry point for potential interventions (Figure 1).
Specifically, the relationships and expectations domain explores the perceptions (i.e., knowledge, attitudes, values, and beliefs that may motivate or hinder behavioural change) of health information and the factors that enable (i.e., cultural, societal, and structural influences that hinder or facilitate behaviour change) and nurture health behaviours of potential target groups. The cultural identity component then determines persons, extended family and neighborhoods (i.e., community structures like the health care, school and religious systems) that ought to be targeted. Such individuals and / or groups or entities should be educated and empowered to make informed health decisions appropriate to their roles and responsibilities in the family and community. This focuses on appropriate health education and health promotion networks to meet the needs of the intended target group (s). The last constituent, cultural empowerment/ appropriateness of health behaviours determine the positive (i.e., individuals’ knowledge, positive beliefs and practices regardless of how small they might be, ought to be recognized, encouraged, and adhered to), existential (i.e., cultural beliefs and behaviours that are endemic to a particular individual, group or community and have no detrimental health implications), and negative (i.e., beliefs and practices that are known to be dangerous to health within the individual, group or community’s cultural, historical, and political contexts) health behaviours of targeted individuals or groups 41, 80.
By evaluating the extent of public health problem (e.g., obesity prevalence) within a socio-cultural context, two components are cross-tabulated in a 3 × 3 matrix (see Table 1 with dietary intake strategies as examples). The proposed intervention should be in congruence with the local practices of the people that identifies them, an attempt to facilitate its effectiveness. The idea is for the intervention to holistically target not only individual people but rather on the context and broader community within which the individual operates 41, 80.
Table 1. A Matrix of Relationships/Expectations and Cultural Empowerment components that influence food choices.| Positive | Existential (not harmful) | Negative | |
| Perceptions | Family gathering through food intake and communal bonding | Eating and sharing for togetherness | Adding salt and additives for tasty food; cooking methods that deplete nutrients |
| Enablers | Money to buy food; Accessibility to healthy foods | Food preparation together | Low income to access healthy foods; patronizing fast foods, already packaged foods in urban areas |
| Nurturers | Family members promote the eating of healthy foods to reduce the risk factors of CVDs | Preparing a list of food items together; developing a menu or planning food intake together | Family members supporting the eating of foods that may increase the risk of CVDs |
Conclusion
Some of the weird longstanding beliefs and perceptions about body weight held by many indigenes have negative health implications and ought to be changed. More positive attitudes that would promote healthy behaviours such as healthy dietary intake and regular physical activity are encouraged. Devoting attention to cultural perceptions and norms surrounding diet and weight and efforts to design appropriate interventions would help reduce associated comorbidities and fatalities connected with overweight and obesity. The understanding is that that perceptions dietary intake and of physical activity vary across cultures, therefore, it would be prudent that more empirical research is required to investigate culture-related educational components of health promotion programmes, with specific focus on the exchange of information related cultural norms, beliefs and perceptions that would improve on the overall health of the people. The PEN-3 model provides a useful cultural framework by which health behaviours (e.g., promoting and compromising) could be critically assessed and managed by researchers, health related professionals and programme planners to create long lasting lifestyle change strategies. Numerous epidemiological studies have consistently proven that overweight and obesity are associated with increased risks of morbidity, disability and mortality. For instance, overweight and obesity are well-connected risk factors for type 2 diabetes mellitus, hypertension and stroke. Therefore, further increases in these two health compromising indicators in the country would have serious impact on the already overburdened healthcare resources in Ghana. Therefore, complimentary preventive measure like behaviour modification is greatly required to control and prevent the rising incidence of overweight and obesity in the country, especially in urban Ghana.
Authors' Contributions
JEH, CB, TH, DP, and TS contributed equally to the writing of this manuscript. All authors have read and approved the final version of the manuscript.
References
- 1. (2010) World Health Organization. Global strategy on diet, physical activity and health: obesity and overweight. http://www.who.int/mediacentre/factsheets/fs311/ en/index.html
- 2.WHO. (2015) Obesity and overweight. WHO. Fact sheet N°311. http://www.who.int/mediacentre/factsheets/fs311/en/
- 3.Agyemang C, Boatemaa S. (2016) Agyemang Frempong G, de-Graft Aikins A. Obesity in sub-Saharan Africa. Metabolic Syndrome: A Comprehensive Textbook. 41-53.
- 4.Adeboye B, Bermano G, Rolland C. (2012) Obesity and its health impact in Africa: a systematic review. Cardiovascular journal of Africa. 23(9), 512-21.
- 5.Lopez A D, Mathers C D, Ezzati M, Jamison D T, Murray C J. (2006) Measuring the global burden of disease and risk factors,1990–2001.Global burden of disease and risk factors. 1, 1-4.
- 6.Ziraba A K, Fotso J C, Ochako R. (2009) Overweight and obesity in urban Africa: A problem of the rich or the poor? BMC public health. 1, 465.
- 7. (2010) World Health Organization. Physical inactivity: A global public health problem. http://www.who.int/dietphysicalactivity/factsheet_inctivity/en
- 8. (2016) World Health Organization (WHO). Obesity and overweight. Geneva: World Health Organization.
- 9.Mbanya J C, Ramiaya K. (2006) Disease and mortality in sub-Saharan Africa. In DT. Jamison, RG. Feachem, MW. Makgoba.2nd edition ed.Washington. DC: WorldBank
- 12.Martorell R, Khan L K, Hughes M L, Grummer-Strawn L M. (2000) Obesity in women from developing countries. , Eur J Clin Nutr 54(3), 247-52.
- 14.Abubakari A R, Lauder W, Agyemang C. (2008) Prevalence and time trends in obesity among adult West African populations A meta-analysis. Obesity Reviews. 9, 297-311.
- 15.Awuah R B, Anarfi J, Agyemang C. (2014) Prevalence,awareness, treatment and control of hypertension in urban poor communities. , J Hypertens 32, 1203-1210.
- 16. (2010) International Diabetes Foundation (IDF). Diabetes Atlas. http://www.diabetesatlas.org/map
- 19.Mensah G A, Sampson U K, Roth G A, Forouzanfar M H, Naghavi M et al. (2015) Mortality from cardiovascular diseases in sub-Saharan Africa, 1990-2013: A systematic analysis of data from the Global Burden of Disease Study 2013: cardiovascular topic. Cardiovascular journal of Africa. 26(1), 6-10.
- 20.Lawoyin T O, Asuzu M C, Kaufman J, Rotimi C, Owoaje E et al. (2002) Prevalence of Cardiovascular Risk Factors in an African, Urban Inner City Community. West Africa Journal Medicine. 21(3), 208-211.
- 21. (2006) World Health Organization (WHO): Obesity and Overweight. Global Strategy on Diet, Physical Activity and Health.
- 22. (2003) World Health Organization (WHO): Report of a Joint WHO/FAO Expert Consultation Report on. Diet, Nutrition and the Prevention of Chronic Disease. Diet, Nutrition and the Prevention of Chronic Disease.Geneva .
- 23.Amugsi D A, Dimbuene Z T, Mberu B, Muthuri S, Ezeh A C. (2017) Prevalence and time trends in overweight and obesity among urban women: An analysis of demographic and health surveys data from 24 African countries,1991–2014. BMJ open. 7(10), 017344.
- 24.Ofori-Asenso R, Agyeman A A, Laar A, Boateng D. (2016) Overweight and obesity epidemic in Ghana: A systematic review and meta-analysis. BMC Public Health. 16(1), 1239.
- 25. (2015) . Ghana Statistical Service (GSS), Ghana Health Service (GHS), and ICF International. Ghana Demographic and Health Survey2014 , Rockville, Maryland, USA:GSS,GHS,ICF.International .
- 26. (2014) . WHO. Cancer Country Profiles for Ghana.http://www.who.int/cancer/countryprofiles/gha_en.pdf?ua=1(Accessed:July21,2017) 4–5 .
- 27.Goran M I.(1Feb).Metabolic precursors and effects of obesity in children: a decade of progress,1990–1999. The American journal of clinical nutrition. 73(2), 158-71.
- 28.Whitaker R C, Pepe M S, Wright J A, Seidel K D, Dietz W H. (1998) Early adiposity rebound and the risk of adult obesity. Pediatrics. 101(3), 5.
- 29.Aryeetey R, Lartey A, Marquis G S, Nti H, Colecraft E et al. (2017) Prevalence and predictors of overweight and obesity among school-aged children in urban Ghana. , BMC Obesity 4(1), 38.
- 30.Annan-Asare J, Asante M, Amoah A G. (2017) Obesity and its Correlates among Junior High School Children in the Accra Metropolis. , J Nutr Health Sci 4(2), 206.
- 31.Mohammed H, Vuvor F. (2012) Prevalence of childhood overweight/obesity in basic school in Accra. , Ghana Medical Journal 46(3), 124.
- 32.Manyanga T, El-Sayed H, Doku D T, Randall J R. (2014) The prevalence of underweight, overweight, obesity and associated risk factors among school-going adolescents in seven African countries. , BMC Public Health 14(1), 887.
- 33.Kumah D B, Akuffo K O, Abaka-Cann J E, Affram D E, Osae E A. (2015) Prevalence of overweight and obesity among students in the Kumasi metropolis. , Journal of Nutrition and Metabolism
- 34.Mogre V, Gaa P K, Abukari R N. (2013) Overweight, obesity and thinness and associated factors among school-aged children (5-14 years) in Tamale, Northern Ghana. , European Scientific Journal,ESJ 9(20).
- 35.Lobstein T, Baur L, Uauy R. (2014) Obesity in children and young people: A crisis in public health. Obesity Reviews. 5(1), 4-85.
- 37. (2004) World Health Organization. Obesity: Preventing and managing the global epidemic report. World Health Organization.
- 38.Scott A, Ejikeme C S, Clottey E N, Thomas J G. (2012) Obesity in sub-Saharan Africa: Development of an ecological theoretical framework. Health Promotion International. 28(1), 4-16.
- 39.Basabe N, Paez D, Valencia J, Rimé B, Pennebaker J et al. (2000) Sociocultural factors predicting subjective experience of emotion: A collective level analysis. Psicothema. 12-1.
- 40.Culture and Emotion: Models of Agency as Sources of Cultural Variation in Emotion. InFeelings and Emotions:The Amsterdam Symposium,Amsterdam,Netherlands2004.CambridgeUniversityPress.
- 41.BeLue R, Okoror T A, Iwelunmor J, Taylor K D, Degboe A N et al. (2009) An overview of cardiovascular risk factor burden in sub-Saharan African countries: A socio-cultural perspective. , Global Health 5, 10-19772644.
- 42.Dutta–Bergman M J. (2004) The unheard voices of Santalis: Communicating about health from the margins of India. Comm Theory. 14, 237-263.
- 43.Niang C I. (1994) The Dimba of Senegal: A support group for women. Reprod Health Matters. 2, 39-45.
- 44.AGB Amoah. (2003) Sociodemographic variations in obesity among Ghanaian adults. , Public Health Nutr.; 6, 751-757.
- 46.Holdsworth M, Gartner A, Landais E, Maire B, Delpeuch F. (2004) Perceptions of healthy and desirable body size in urban Senegalese women. , Int J Obes 28, 1561-1568.
- 47.Siervo M P, Grey P, Nyan O A. (2006) Urbanization and obesity in The Gambia: A country in the early stages of the demographic transition. Eur J Clin Nutr. 60, 455-463.
- 48.A Fat Renzaho. (2004) rich and beautiful: Changing sociocultural paradigms associated with obesity risk, nutritional status and refugee children from sub-Saharan Africa. Health and Place. 10, 105-113.
- 49.Puoane T, Bradley H, Hughes G. (2005) Obesity among black South African women. Human Ecology Special. 13, 91-95.
- 50.Bourne L. (1996) Dietary intake in an urban African population in South Africa with special reference to the nutrition transition. Thesis for Doctor of Philosophy. , University of Cape Town, South Africa
- 53.Markey C N, Tinsley B J, Ericksen A J, Ozer D J, Markey P M. (2002) Preadolescents' perceptions of females' body size and shape: Evolutionary and social learning perspectives. , Journal of Youth and Adolescence 31(2), 137-46.
- 54.Nasser M. (1988) Eating disorders: The cultural dimension. Social psychiatry and psychiatric epidemiology. 23(3), 184-7.
- 55.Massara E B. (1989) Que gordita!: A study of weight among women in a Puerto Rican community.AmsPressInc.
- 56.Rguibi M, Belahsen R. (2006) Fattening practices among Moroccan Saharawi women. PMID: 17333802. East Med Health J.12: 619.
- 57.Smith A D. (2009) Girls being force-fed for marriage as fattening farms revived.http://www.guardian.co.uk/world/2009/mar/01/mauritania-force-feeding-marriage.
- 58.Kumanyika S. (1993) Special issues regarding obesity in minority populations. , Annals of Internal Medicine 19, 650-654.
- 59.Caperchione C M, Kolt G S, Mummery W K. (2009) Physical activity in culturally and linguistically diverse migrant groups to Western Society. Sports Medicine. 39(3), 167-77.
- 60.Evenson K R, Sarmiento O L, Ayala G X. (2004) Acculturation and physical activity among North Carolina Latina immigrants. , Social Science and Medicine 59(12), 2509-22.
- 61.Guerin P B, Elmi F H, Corrigan C. (2007) Body composition and cardiorespiratory fitness among refugee Somali women living in New Zealand. , Journal of Immigrant and Minority Health 9(3), 191-6.
- 62.Lawton J, Ahmad N, Hanna L, Douglas M, Hallowell N. (2005) I can't do any serious exercise’: Barriers to physical activity amongst people of Pakistani and Indian origin with Type 2 diabetes. Health Education Research. 21(1), 43-54.
- 63.Walseth K, Fasting K. (2003) Islam’s view on physical activity and sport: Egyptian women interpreting Islam. International Review for the Sociology of Sport. 38(1), 45-60.
- 64.Bray G A. (1996) Coherent, preventive and management strategies for obesity. InCiba Foundation. Symposium201-The Origins and Consequences of Obesity.John Wiley & Sons,Ltd 228-254.
- 65.Aikins A D. (2007) Ghana's neglected chronic disease epidemic: A developmental challenge. , Ghana Medical Journal 41(4), 154.
- 66.Agyei-Mensah S.Accra (Ghana) in Transition: Epidemiological change at the turn of the 21st century.2004.Paper presented at the Seminar on Health in African Cities, Harvard Centre for Population Studies. , Harvard University, Cambridge(31stMarch2004)
- 67. (2004) . Ghana Statistical Service (GSS), Noguchi Memorial Institute for Medical Research (NMIMR), and ORC Macro. Ghana Demographic and Health Survey2003. Calverton, Maryland:GSS,NMIMR,and ORC Macro .
- 68.Ghana Statistical Service.. Ghana Health Service & ORC Macro. Ghana Demographic and Health Survey2008.Accra, Ghana and Calverton, MD:GSS,GHS and ORC Macro2009 .
- 69.Prevalence. (2008) detection, management, and control of hypertension in Ghanaian civil servants. Ethnicity & Disease. 18(4), 505-11.
- 70.Lassey A T, Wilson J B. (1998) . Trends in maternal mortality in Korle Bu Hospital, 1984–1994. Ghana Medical Journal. 32a: 910-916.
- 71.Kumi-Aboagye P.Status of MDG 5: Evidence from the field. Paper presented at the National Consultative Meeting on the Reduction of Maternal Mortality. in Ghana.Accra.8thJuly2008
- 72.Amoah A G, Owusu S K, Adjei S. (2002) Diabetes in Ghana: A community-based prevalence study in Greater Accra. Diabetes research and clinical practice. 56(3), 197-205.
- 73.Agyemang C. (2006) Rural and urban differences in blood pressure and hypertension in Ghana, West Africa. Public Health. 120-525.
- 74.Medeiros F, Casanova M D, Fraulob J C, Trindade M. (2012) How can diet influence the risk of stroke? International Journal of Hypertension.
- 75.Aikins de-Graft, A. (2003) Living with diabetes in rural and urban Ghana: a critical social psychological examination of illness action and scope for intervention. , Journal of Health Psychology 8(5), 557-72.
- 76.Mcinnis K J, Franklin B A, Rippe J M. (2003) Counseling for physical activity in overweight and obese patients. American Family Physician. 67(6), 1249-56.
- 77.Dietz W H. (1998) Health consequences of obesity in youth: childhood predictors of adult disease. Pediatrics. 101, 518-525.
- 78.Agyei-Mensah S, de-Graft Aikins A.Epidemiological transition and the double burden of disease in Accra. , Ghana. Journal of Urban Health 87(5), 879-97.
- 79.Sanuade O A, Anarfi J K, Aikins A D, Koram K A. (2014) Patterns of cardiovascular disease mortality in Ghana: a 5-year review of autopsy cases at Korle-Bu Teaching Hospital. Ethnicity & Disease. 24(1), 55-9.
- 80.James D. (2004) Factors influencing food choices, dietary intake, and nutrition-related attitudes among African Americans: application of a culturally sensitive model. Ethnicity and Health. 9(4), 349-67.
- 81.Hochbaum G M. (1981) Strategies and their rationale for changing people's eating habits. , Journal of Nutrition Education 13-1.
- 82.Crockett S J, Sims L S. (1995) Environmental influences on children's eating. , Journal of Nutrition Education 27(5), 235-49.
- 85.Guerin P B, Diiriye R O, Corrigan C. (2003) Physical activity programmes for refugee Somali women: Working out in a new country. Women Health. 38(1), 83-99.
- 86.Lang A, Froelicher E S.Management of overweight and obesity in adults: behavioral intervention for long-term weight loss and maintenance. , European Journal of Cardiovascular Nursing 5(2), 102-14.
- 87.James D C, Rienzo B A, Frazee C. (1996) Using focus groups to assess barriers and motivators to healthy eating among adolescents. Health Educator. 39-44.
Cited by (1)
- 1.Aberman Noora-Lisa, Nisbett Nick, Amoafo Adjoa, Areetey Richmond, 2022, Assessing the readiness of small cities in Ghana to tackle overweight and obesity, Food Security, 14(2), 381, 10.1007/s12571-021-01234-z