Abstract
In Rwanda, CVDs accounts around 14% of all death. Studies on knowledge, attitude, and practice (KAP) would be of great value in helping public health professionals develop targeted programs and measure the effectiveness of interventional programs. The main objective of this study was to analyze the KAP about CVDs among adult patients attending public health centers located in the City of Kigali, Rwanda. A total of 384 adult patients were enrolled in this study. A structured questionnaire was used. Data entry and analysis was done using SPSS version 21. Findings were presented as frequencies and percentages in tables. For determining the KAP-levels, the overall scores were determined for each respondent by adding up the scores through the KAP-related questions. The mean age was 36.4 years, primary school (57.3%), married (62.8%), self-employed (40.9%), and females predominated (61.5%). The knowledge mean score was 14.2 and 76% had high level of knowledge of CVD risks and prevention. The average attitude score for all respondents was 17.6 and 22.9% of the respondents showed negative attitude towards CVDs prevention. Research findings revealed that 36.5 % were not practicing physical activity and exercise. The mean practice score for all respondents was 3.9 and 70% of respondents had negative practice towards CVDs prevention. Poor CVDs prevention practices were observed among the study participants. Therefore, it is necessary to establish more effective educational interventions intended to promote positive health behaviors related CVD prevention
Author Contributions
Academic Editor: Lucio Mango, Italy
Checked for plagiarism: Yes
Review by: Single-blind
Copyright © 2022 Leonard Ntwari Nyagasare, et al.
 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Competing interests
The authors have declared that no competing interests exist.
Citation:
Introduction
In nowadays non-communicable diseases (NCDs) became a big burden Worldwide, as they are the leading causes of mortality and morbidity, and the high number is found in the developing countries as stated. For example, in 2019 18.6 million deaths were due to CVDs complications 1. Coronary heart disease and stroke, these two contributed to about 17·8 million deaths in 2017, among them greater than three quarters occurred in low income and middle-income countries. While the target of the United Nations Sustainable Development Goal especially in the indicator 3.4.1 aim is to decrease premature death caused by non-communicable diseases by a third by 2030 2. To achieve the target of Sustainable development Goal 3 which is to decrease premature deaths that result from non-communicable diseases by 30%, the strong and urgent measures should be taken to implement current cost-effective policies and interventions 3.
The Cardiovascular disease (CVD) has been the leading cause for mortality and morbidity for around 20 years since 2000 till 2019, and it has dramatically increased of the leading causes of morbidity and death among non-communicable diseases 4. Again, different findings have found that CVDs contribute to the high number of deaths, for instance of all global deaths one-third (19.9 million) was due to CVD 5.
In Africa, 38% of all non-communicable disease-mortality resulted from CVD related complications, this refers to rising threat of both CVD and Non-communicable diseases (Keates & Ntsekhe, 2017). In Sub-Sahara Africa, NCDs related deaths contributes to 35% of all deaths, which makes it the second killer after a combination of communicable, maternal, neonatal and nutritional diseases. The recent data clarifies that SSA is facing a challenge of contemporary double burden of disease due to a combination of Noncommunicable diseases and communicable, where CVD accounts 13% of all deaths, and 37% among non-communicable diseases 6.
According to the WHO, in Rwanda, NCDs account 44% of all deaths in 2015, and 14% of all deaths resulted from CVDs 7.The Rwandan target was to reduce CVD by 80% by 2020, while the rate of NCDs in 2015 was 44% of all deaths and CVD accounts 14% of all diseases, the target Rwandan strategic plan of 2014-2019 shows that the most presented CVDs included “hypertension, cardiomyopathies, stroke/TIA, rheumatic and congenital heart disease; and some of them can be prevented easily” 8.
It has also been discovered that patients with CVDs are at risk of death when infected by Covid-19 pandemic; in a study conducted by Chinese Center for Disease Control and Prevention, reported that of the Covid-19 deaths 10.5% were CVDs cases 9.
The lack of adequate knowledge is one of the main contributors of CVD deaths; for instance, in Europe, CVD related mortality has increased, more than 1.8 milion people die by CVD complications every year, which is equivalent to 36% of all deaths. For some of Europe countries, this is the first time in 50 years declared the increase in CVD related deaths. This trend is due to insufficient knowledge on CVD, limited varied investment in the prevention of CVD 10.
A study carried out in the South Arabia reported some of the most common risk factors associated with CVD in this community, including “inadequate physical exercise, obesity and stress” as mentioned by respondents. Among study participants, a small number (18.5%) have knowledge on CVD risk factors. The majority (99%) of study participants reported that they gained knowledge about CVDs from school, and other 83.7% have read education material. Among the respondents, 60% were able to recognize some of preventable factors including cessation of smoking 11.
In countries like Malaysia, the participants could identify some CVD preventive measures including “intake of vegetables and risk factors such as unhealthy diet (88%), most of respondents recognized that smoking and obesity are risk factors, and others reported that physical exercise is one of preventive measures of CVDs 12. As stated by Ashley k. et al, a gap in knowledge of CVD epidemiology has been discovered in Africa which refers to limited sources of data on CVDs on this continent 13.
A systemic review study conducted in Sub-Sahara Africa on both quantitative and qualitative studies documented a low level of knowledge and awareness among the study participants, since majority of studies stated that more than half of respondents had inadequate knowledge of CVDs and/ or their risk factors 14.
The study conducted by in Rwanda revealed that there is poor knowledge toward CVDs among rural community where 85.8% of the participants have no knowledge about this type of disease. The same study from this rural setting reported inadequate practices towards CVD prevention among rural community, since among study participants 79.6% habitually consume alcohol, 23.7% have smoking habit, 53.1% eat vegetables while only 5.9% eat fruits on a daily basis, and 66.5% consume cooking oil daily. Most of the respondents (99.0%) never tested for blood cholesterol, 66.2% never done blood pressure test, and 60.1% never went for medical checkup 15.
Also a study conducted in a Rwandan semi-urban setting reported that low level of education, separation with spouse are linked with inadequate knowledge of hypertension (one of cardiac disease); while among the diseased respondents 70.7% never performed their blood pressure checkup; aged people also have high risk of getting hypertension. The general prevalence of hypertension among participants was 15.3% 16.
The same study from semi-urban population also revealed that lifestyle changes, unhealthy behaviors and change of eating habits resulted from socio-economic transition and urbanization may clarify the increased risk of hypertension observed in this community. Again, the low level of knowledge on this type of CVD may result from insufficient interventions in prevention and control of this disease by public health practitioners, since for long time health programs have been focusing on contagious diseases than NCDs 16.
The factors contributing to CVDs in developing countries have been identified, these include “smoking, high alcohol and salt intake, dietary factors, diabetes, high blood pressure and psychosocial aspects like, anxiety, stress and depression. Family history and gender differences have also been classified as other factors contributing to high risks of developing CVD 17.
To achieve the Rwandan target “to reduce NCDs by 80%” and to prevent these diseases including CVDs, there is a need to first raise the knowledge toward good practice about such diseases in order to take precautions accordingly. The issue is whether the community knows these diseases, what the risk factors are and how to prevent them. Some studies have reported low level of knowledge and practices about CVDs in rural and semi-urban settings of Rwanda 15, 16, 18. However, there is very limited data about knowledge, attitude or practices among urban community of Rwanda, the reason to conduct this study in the city of Kigali.
In fact, some studies have reported the low level of knowledge, attitude and practices on CVDs in different parts of the world, but also there is inadequate data from Rwandan community especially among urban settings. In addition, the most recent Demographic and Health Data did not provide specific data regarding CVDs current status 19. Therefore, this study is intended to investigate the level of knowledge, attitude and practices about CVDs among Rwandan community, with focus on urban population. Hence, help health practitioners to develop interventions according to the provided and most updated evidences. The overall objective of this study was to assess the knowledge, attitudes and practices about cardiovascular diseases among adult patients attending public health centers in Rwanda.
Methods
Research Design
This study was a cross-sectional and quantitative study that was conducted among adult patients attending public health centers (HCs) located in Kigali City, Rwanda between October and December 2021. A structured questionnaire was used to collect data. The City of Kigali is composed by three districts (Gasabo, Kicukiro and Nyarugenge).
Target Population
The target population was the adult patients that were attending the public health centers selected to take part in the study. Participants were coming from Gahanga HC, Gatenga HC and Niboye HC of Kicukiro district; Muhima HC, Corunum HC and Kanyinya HC of Nyarugenge district and Remera HC, Kacyiru HC and Bumbogo HC of Gasabo district.
Sample Size
In this study, the sample size was calculated basing on Cochran’s formula, when the population is infinite. In 1977, Cochran developed a formula to calculate a representative sample for proportions. The sample size was derived from the table for a minimum sample size estimate for a population survey with a 95% confidence interval 20 using the following equation:
Z value = ± 1.96 at 95% confidence interval, p = 50% an expected frequency value which is recommended 50% by Fisher et al (2008). Since no estimate is available: q = 1- p =>1- 0.5=0.5 and d = 5%: level of precision. Then, the following formula was applied:
n = Z x Z (p (1-p)/ (d x d)) =1.960 x 1.960 (0.50(1 - 0.50) / (0.05 x 0.05)) =384.16 ≈ 384
The required minimum sample size of 384 adult patients was equitably allocated among the nine public HCs that were selected for the study.
Sampling Techniques
Flow chart and recruitment process using multistage sampling to choose public HCs and patients to include in the study are shown in Appendix 3. The three districts of Kigali City were considered as strata, where 3 public HCs were randomly chosen for each district to include in the study. A total of 384 adult outpatients attending the selected public HCs were selected via a systematic random sampling.
Inclusion and Exclusion Criteria
Were included in the study adult patients aged from 18 and above years old attending one of the public HCs selected for the study, and who were able to speak. The patients who were aged below 18 years old and not able to speak were directly excluded in the study. Participants were joined the study after signing an informed consent. Failing to give a consent, a participant was automatically conduced to an exclusion in the study. Consented participants were interviewed by trained surveyors using a set of validated KAP structured questionnaire that should be completed within 15 minutes.
Data Collection Instruments
An administered questionnaire was settled and used to collect the quantitative data. The first section consists of socio-demographic data. Section II consists of 19 items for knowledge regarding cardiovascular diseases. Section III consists of 5 items related to the attitudes towards CVDs, while the section IV is about participant’s practice towards CVDs and accounts for 8 items. Categorical responses (Yes/No) were used for knowledge (K), Likert scale (Strongly Disagree, Disagree, Neutral, Agree and Strongly Agree) for attitude (A) and multiple-choice questions for practice items (P). The total score was categorized by using SPSS Score Assessment.
Procedures of Data Collection
The researcher was first of all introduced himself to the participants, explaining the purposes of the study, and obtaining written consent from the participants who meet the inclusion criteria and willing to be part of the study. The person interview with one respondent based on a semi-structured questionnaire took around 15 minutes. It is worth mentioning that all data were collected by trained nurses from the outpatient department of the selected public health centers.
Data Analysis
In this section, data was coded and analyzed using statistical package for social science (SPSS) v.21.0. Descriptive statistics and inferential statistics were performed for cross-tabulation, data presentation and interpretation. The overall score for knowledge, attitudes and practices towards CVDs was calculated using SPSS Score Assessment and was calculated by adding up the scores for each respondent across all questions. Therefore, a scoring criterion was used to determine the level of knowledge, attitude and practice accordingly. For knowledge, a total of 19 questions were weighed up by using SPSS score assessment and the score was 1 score for a correct answer and 0 for false answer. For the attitude, overall attitude score was calculated for each respondent by adding up the scores across the 5 attitude-related questions. The answer recorded as “5 scores to strongly-agree, 4 scores to agree, 3 scores to neutral, 2 scores to disagree and score to strongly disagree answer for positive statement” and “5 scores to strongly-disagree, 4 scores to disagree, 3 scores to neutral, 2 scores to agree and 1score to strongly agree answer for positive statement”. The answers were ranged in the Likert scale format. The practice’ section contained 8 questions related to CVDs, and among them 5 questions that were relevant to every participant were marked for each respondent. If a respondent provided a correct response, he/she was given 1 score. If he/she provided a false response, he/she was marked by zero score. An overall practices score was determined for each respondent by adding up the scores across the 5 among 8 practice-related questions. For factors associated with practices on CVD prevention, chi-square test and binary logistic regression were performed. The level of significance was assessed using a p-value of (0.05) and 95% confidence interval. Furthermore, multivariate logistic regression was conducted for all variables of interest with p-value <0.05 in the bivariate model. More detailed information about the scoring assessment is found in the Appendix 2 which includes the questionnaire.
Ethical Considerations
In the first place, Research permit and introduction letter from the MKUR postgraduate program was used so as to obtain permission to carry out the research study in the selected study areas. Secondly, the permission from the study areas was requested prior to data collection. In compliance with ethical compliance, the researcher ensured confidentiality of the respondents by coding the questionnaires, and giving of informed consent to the respondents to make sure that they first agree to take part in the study out of their own free choice.
Results
Socio-Demographic Characteristics of the Respondents
The sociodemographic characteristics considered in this study were the respondents’ residence, gender, age, education, marital status, occupation, religion, health insurance ownership, social category, monthly income and family history of CVDs.
Research findings in Table 1 indicate that 83.6% of respondents were coming from urban zones, 61.5% were females, 53.6% were aged between 18 and 35 years (average age: 36.4 years, SD: 13.1, minimum age: 18 and maximum age: 86), 57.3% had primary educational level, 62.8% were married, 40.9% were self-employed, 45.8% were protestants, 90.4% owned health insurance, 48.2% were in the third social category and 69.0% had a revenue ranged between 0 and RWF 30,000. More than a half (60.4%) of respondents expressed they had not experienced CVDs in their families.
Table 1. Sociodemographic characteristics of the respondents| Variables | Categories | Frequency (n) | Percent (%) |
|---|---|---|---|
| Residence | Rural | 63 | 16.4 |
| Urban | 321 | 83.6 | |
| Gender | Male | 148 | 38.5 |
| Female | 236 | 61.5 | |
| Age category | 18-35 years | 206 | 53.6 |
| 36-50 years | 124 | 32.3 | |
| >50 years | 54 | 14.1 | |
| Level of education | Primary | 220 | 57.3 |
| Secondary | 126 | 32.8 | |
| Tertiary | 38 | 9.9 | |
| Marital status | Single | 143 | 37.2 |
| Married | 241 | 62.8 | |
| Religion | Catholic | 166 | 43.2 |
| Protestant | 176 | 45.8 | |
| Muslim | 15 | 3.9 | |
| No religion | 27 | 7.1 | |
| Occupational status | Unemployed | 153 | 39.8 |
| Self-employed | 157 | 40.9 | |
| Employed | 74 | 19.3 | |
| Health insurance | Yes | 347 | 90.4 |
| No | 37 | 9.6 | |
| Social category | Category 1 | 51 | 13.3 |
| Category 2 | 148 | 38.5 | |
| Category 3 | 185 | 48.2 | |
| Monthly income RWF | 0-30,000 | 265 | 69.0 |
| 30,001-100,000 | 88 | 22.9 | |
| > 100,000 | 31 | 8.1 | |
| Family history of CVDs | Yes | 63 | 16.4 |
| No | 232 | 60.4 | |
| Do not know | 89 | 23.2 |
Knowledge about CVDs and Risk Factors among Adult Patients
The knowledge was assessed using different parameters related to participants’ knowledge about CVDs, and findings are summarized in the following table 3 accordingly.
Findings in Table 2 show that 54.7% knew that smoking increases the risk of developing CVDs, 77.6% knew that consuming a lot of vegetables and fruits does not increase the risk of CVD, 76.3% knew that consuming too much salt is a risk to CVD, 77.3% knew that having excess body weight increases ones risk of CVD, 54.2% did not know that a family history of CVD increases ones risk of acquiring CVD, 55.5% knew that regular consumption of red meat is not healthier than white meat, 52.6% knew that cardiovascular diseases are curable upon completion of described dose, 62.0% refused that men are at higher risk of CVDs compared to women, 80.7% knew that excessive alcohol drinking is dangerous to cardiovascular health, 52.9% did not know that a person may know that he/she has CVD based on signs and symptoms alone, 78.1% refused that a person with CVD may infect a close person, 83.1% knew that high blood pressure is a risk factor of CVD, 64.3% knew that animal fat is not healthier than plant oil, 66.9% knew that old age is a risk factor for CVD, 78.6% knew that stress increases ones risk of getting CVD, 64.6% knew that exercising regularly is not harmful to cardiovascular health, 64.1% refused that high cholesterol in blood prevents one from CVD, more than a half (51.0%) of respondents did not know that CVD are not preventable, while 78.6% knew that doing health check-ups frequently is not harmful.
Table 2. Respondents’ knowledge about CVDs and risk factors| Variables | Yes n(%) | No n(%) |
|---|---|---|
| Smoking does not increase a risk of CVD. | 174(45.3) | 210(54.7) |
| Consuming a lot of vegetables and fruits increases the risk of CVD. | 86(22.4) | 298(77.6) |
| Consumption of too much salt is a risk to CVD. | 293(76.3) | 91(23.7) |
| Having excess body weight increases one’s risk of CVD. | 297(77.3) | 87(22.7) |
| A family history of CVD increases one’s risk of acquiring CVD. | 176(45.8) | 208(54.2) |
| Generally, regular consumption of red meat is healthier than white meat. | 171(44.5) | 213(55.5) |
| Cardiovascular diseases are curable upon completion of described dose. | 202(52.6) | 182(47.4) |
| Men are at higher risk of CVDs compared to women. | 146(38.0) | 238(62.0) |
| Excessive alcohol drinking is dangerous to cardiovascular health. | 310(80.7) | 74(19.3) |
| A person may know that he/she has CVD based on signs and symptoms alone. | 181(47.1) | 203(52.9) |
| A person with CVD may infect a close person. | 84(21.9) | 300(78.1) |
| High blood pressure is a risk factor of CVD. | 319(83.1) | 65(16.9) |
| Animal fat is healthier than plant oil. | 137(35.7) | 247(64.3) |
| Old age is a risk factor for CVD. | 257(66.9) | 127(33.1) |
| Stress increases one’s risk of acquiring CVD. | 302(78.6) | 82(21.4) |
| Exercising regularly is harmful to cardiovascular health. | 136(35.4) | 248(64.6) |
| High cholesterol in blood prevents one from CVD. | 138(35.4) | 246(64.1) |
| CVD is not preventable. | 188(49.0) | 196(51.0) |
| Doing health check-ups frequently is harmful. | 82(21.4) | 302(78.6) |
| Variables | n (%) | ||||
|---|---|---|---|---|---|
| SD | Disagree | Neutral | Agree | SA | |
| Everyone can get CVD. | 56(14.6) | 50(13.0) | 49(12.8) | 101(26.3) | 128(33.3) |
| If I had CVD, I would go for regular medical checkup. | 57(14.8) | 61(15.9) | 71(18.5) | 137(35.7) | 58(15.1) |
| If I had CVD, I would like to exercise more. | 58(15.1) | 56(14.6) | 77(20.1) | 101(26.3) | 92(24.0) |
| If I had CVD, I would like to change my eating habits. | 50(13.0) | 32(8.3) | 53(13.8) | 110(28.6) | 139(36.2) |
| If I had CVD, I would like to quit smoking. | 43(11.2) | 25(6.5) | 31(8.1) | 104(27.1) | 181(47.1) |
Overall Knowledge Score
This part provides the general score on residents’ knowledge about CVDs, the following figure provides the actual data.
Nineteen (19) questions related to the knowledge towards CVDs were appraised by using SPSS score assessment and the score was one score for a correct answer and zero for false answer. An overall knowledge score was calculated by adding up the scores for each respondent across all 19 questions. Findings in Figure 1 specify that 76% of respondents had a high level of knowledge towards CVDs whereas 24% had shown a low level of knowledge towards CVDs. The mean knowledge score for all participants was found to be 14.2 (SD = 1.6). The minimum score was 9.9 scores and the maximum score was 19 scores.
Attitudes about CVDs and Risk Factors among Respondents
In this study, attitude was assessed using different parameters, it includes five questions related to participants’ attitudes about CVDs, and the key findings on this aspect are summarized in the following table accordingly.
In this table, SD stands for Strongly Disagree, SA stands form Strongly Agree
Study results as presented in Table 4 reveal that 33.3% of respondents strongly agreed that everyone can get CVD, 35.7% agreed that if he/she had CVD, he/she would go for regular medical checkup, 26.3% agreed that if he/she had CVD, he/she would like to exercise more, 36.2% strongly agreed that if he/she had CVD, he/she would like to change their eating habits and 47.1% strongly agreed that if he/she had CVD, he/she would like to quit smoking.
Table 4. Respondent’s practices towards CVDs| Variables | Items | Frequency (n) | Percent (%) |
|---|---|---|---|
| Currently smoking | Yes | 92 | 24.0 |
| No | 292 | 76.0 | |
| Tried to stop smoking (n=92) | Yes | 51 | 55.4 |
| No | 42 | 44.6 | |
| Currently consuming alcohol | Yes | 145 | 37.8 |
| No | 239 | 62.2 | |
| Type of oil or fat mostly used | Vegetable oil | 304 | 79.2 |
| Butter or ghee | 23 | 6.0 | |
| Margarine | 57 | 14.8 | |
| Physical activity and exercise practice | Yes | 244 | 63.5 |
| No | 104 | 36.5 | |
| Frequency of physical activity and exercise practice (n=244) | Every day | 35 | 14.4 |
| Occasionally | 121 | 49.6 | |
| Every weekend | 63 | 25.8 | |
| Never | 25 | 10.2 | |
| CVDs checkup | Yes | 124 | 32.3 |
| No | 242 | 63.0 | |
| Do not remember | 18 | 4.7 | |
| Type of CVD checkup done (n=124) | Hypertension | 61 | 49.2 |
| Diabetes | 13 | 10.5 | |
| Stroke | 4 | 3.2 | |
| Cardiomyopathies | 43 | 34.7 | |
| Rheumatic | 2 | 1.6 | |
| Congenital heart disease | 1 | 0.8 |
Overall Attitude Score
This part provides the general score on residents’ knowledge about CVDs, the following figure provides the actual data.
The overall attitude score was calculated for each respondent by adding up the scores across the five (5) attitude-related questions. The true answer recorded 5 scores and the false answer got zero. The answers were ranged in the Likert scale format. From the findings presented in Figure 2, the researcher established that 296 (77.1%) of all respondents (384) had positive attitude towards CVDs while 88 (22.9%) showed negative attitudes towards CVDs. The mean attitude score for all respondents was 17.6 (SD = 5.7, minimum score = 5 and maximum score = 25).
Figure 2.Distribution of respondents’ attitudes towards CVDs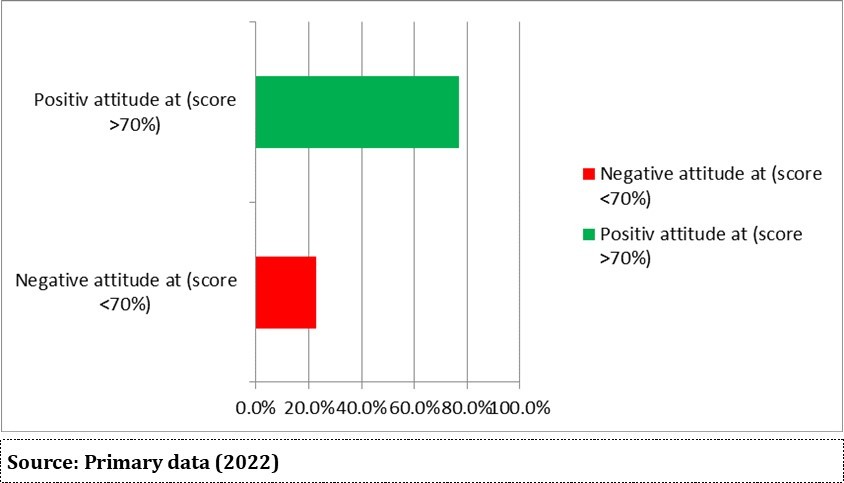
Practices towards Cardiovascular Diseases
This section contains different parameters, including five main questions and 3 sub-questions related to CVDs and were marked for each respondent accordingly.
Research findings presented in Table 4 revealed that 76.0% were not smoking but 55.4% of those who were smoking had tried to stop smoking, 62.2% of respondents were not consuming alcohol, 79.2% were using vegetable oil in cooking, 63.5% were practicing physical activity and exercise, where among those practicing physical activity and exercise 49.6% were doing it occasionally, and only 32.3% of respondents accepted they are doing regular CVDs’ checkup and 49.2% of them have been checked up hypertension followed by cardiomyopathies at 34.7%.
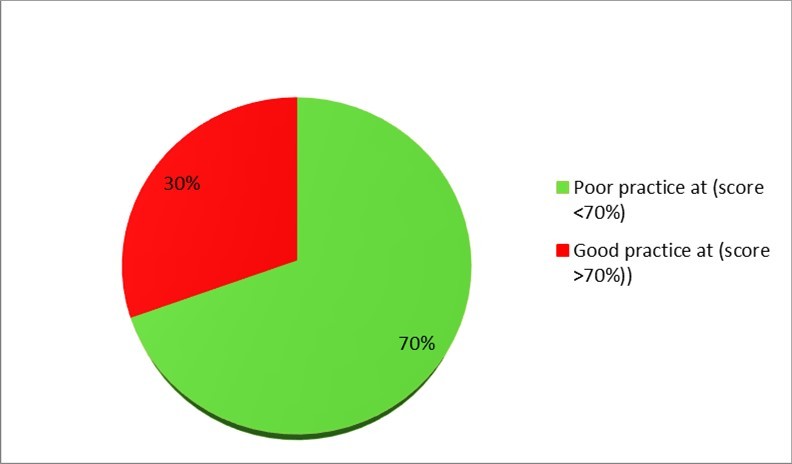
Overall Practice Score
The practice’ section contained five questions related to CVDs and were marked for each respondent. If a respondent provided a correct response, he/she was given a score of 1 score. If he/she provided a false response, he/she was marked by zero.
An overall practices score was determined for each respondent by adding up the scores across the 5 main practice-related questions. The total score was 5 scores.
Research findings presented in Figure 3 revealed that 30% of all respondents had good practice while 70% presented poor practice towards CVDs. The mean practice score for all respondents was 3.9 (SD = 0.7). The minimum score was 2.5 scores and the maximum score was 5 scores.
Discussion
The NCD epidemic continues to accelerate amongst the ongoing infectious diseases battle, health-care systems in the world are increasingly regarding CVDs in particular and NCDs in general as a top public health priority 21. To curb this distressing trend, health literacy has a prominent significance in prevention of CVD both at the primary and secondary levels 22, 23.
Defined health literacy as the “individual’s knowledge, motivation, and competences to access, understand, appraise, and apply health information in order to make judgments and take decisions in everyday life concerning health care, disease prevention, and health promotion to maintain or improve quality of life during the life course” 24.
With a total 75.5% of participants having an overall adequate knowledge regarding to CVD risk factors, this present study demonstrated a highest level of health literacy in an urban setting of Rwanda. Our rates of CVD literacy echoes on the same level with findings of previous studies from South Africa 25, Iran 26 and Malaysia 27 which produced knowledge rates of 75.3, 78.7 and 81% respectively.
Contrary to these findings, regional studies from Nigeria with 44% 28 and 47.5% in Cameroon 29 revealed considerably low rates of CVD knowledge. This perceived variability in knowledge rates between cited studies could be explained by the education-level differences among study participants and diversity of tools used for knowledge assessment.
With regards to knowledge of specific risk behaviors, more than half of participants in this study acknowledged smoking (54.7%), having excess body weight (77.3%), excessive alcohol drinking (80.7%), consuming too much salt (76.3%), stress (78.6%) as CVDs risk factors, while having a family history of CVD was acknowledged by 45.8%. In other studies, a wide variation of knowledge rates regarding individual risk factors is observed in the literature. For instance, smoking has been recognized as a CVD risk by 36.2–93.2% of participants 25, 27, 28, excess alcohol intake by 40.7% and 65% unhealthy diet by 2.8–88% 12 and excess body weight by 1.6–100% 30.
In contrast to our findings, a study conducted in Kuwait 31 recognized family history as an attributable risk of CVD. However, in a couple of other studies conducted in Cameroon 29, Turkey 32 majority (> 50%) of participants were unaware of the increased risk of acquiring CVD in the presence of a positive family history.
In this study, merely 35.7% had agreed that if they experienced a CVD, they would go for regular medical checkup. This was translated in the fact that only 32.3% of respondents accepted they are doing regular CVDs’ checkup. The study results show that the study participants had good attitude to CVDs (77.1%) even if simply 36.2% of participants had strongly agreed that if they had CVD, they would like to change their eating habits. This is in consistent with a study conducted Eastern Nepal, which reported that some of respondents revealed that if they had cardiovascular disease, they would: make regular checkups (92.7%), do more physical exercise (90.4%), change diet (93.9%), or stop smoking (90.6%) 33; and to another study conducted in Malaysia which reported that participants would make regular checkups (81%), eager to exercise more (94.9%), easily change their diet (70.1%) and quit smoking or become passive smoker (79.2%) if they were sick from CVD 34.
In contrast, a study conducted among migrant Chinese in Beijing found that negative attitudes on stop smoking were still high (56.1%) 34. Similarly, in a study done among French pregnant smokers also noted that 59.8% of them did not respond to the offer of cessation services 35.
The percentage of good practice in the present study was around 30.5% which indicates that the behaviour to reduce the CVD risk was non-promising and not optimal. It was consistent with the result found in a study conducted in low level of practice on keeping the normal weight between 28%-52% and nearly 59% in patients with CVD and the overall practice regarding CVD risk reduction behaviour were (50%) 36.
In the present study, some of practice items were reported as positive practice including not smoking (76.0%), trying to stop smoking (55.4%), not consuming alcohol (62.2%), using vegetable oil in cooking (79.2%), practicing physical activity and exercise (63.5%). These findings were consistent with what found North-East coast Malaysia 34, but inconsistent with another study conducted by Robinson and noted that the practice regarding maintaining the desired weight among CVD patients was lower between 27.6% and 52% as compared to our result 37. The comparison here may be biased since the interpretation of normal weight might differ as reported in other studies among British Bangladeshi women, 20% of them perceived that their weight were normal although in the actual fact, it was abnormal 38.
Conclusion
This study revealed the current level of public knowledge, attitude, and practice regarding CVD, risk factors and prevention. Although more than half of the current study participants had high knowledge and attitude about CVD, their behavior is not satisfied. Consequently, it is necessary to establish more effective educational interventions intended to promoting positive health behaviors and explaining to the public that knowledge and action regarding the reduction of risk factors are linked to reduced CVD and mortality.
References
- 1.American Heart Association. (2021) . Heart Disease & Stroke Statistical Update Fact Sheet.Global Burden of Disease .
- 2.Kaptoge S, Pennells L, Bacquer D, Cooney M, Kavousi M et al. (2019) World Health Organization cardiovascular disease risk charts: revised models to estimate risk in 21 global regions .Lancet Glob Health.
- 3.Gregory A, A M George, Catherine O, Giovanni A, Enrico A et al. (2020) The Global Burden of Cardiovascular Diseases and Risks: A Compass for. , Global Action.Journal of the American College of Cardiology 76(25), 2982-3021.
- 4.World Health Organization. (2020) 09).Medical life sciences. Retrieved from WHO highlight leading cause of mortality and morbidity worldwide from. to 2019: http://www.WHO-highlights-leading-causes-of-mortality-and-morbidity-worldwide-from-2000-to-2019.pdf
- 5.A R Gregory, Catherine J, Amanue A, Foad A-A, Gebre A et al. (2017) Global, regional and national burden of cardiovascular diseases for 10 causes from1990to2015.Journalof the American College of Cardiology. 70(1), 26-28.
- 6.Yuyun. (2020) Cardiovascular Diseases in Sub-Saharan Africa Compared to High-Income Countries: An Epidemiological Perspective.Global Heart. 15(1), 15.
- 7. (2018) World Health Organization.Noncommunicable Diseases (NCD): Country Profiles. Retrieved from https://www.who.int/nmh/countries/rwa_en.pdf.
- 8. (2019) . Ministry of Health [Rwanda].Rwanda Noncommunicable Diseases National Strategic Plan July2014 – June2019).Kigali: .
- 9.Vetta F, G V. (2020) Coronavirus Disease 2019 (COVID-19) and cardiovascular disease.Cardiol Cardiovasc Res. 1(1), 1-12.
- 10. (2020) European Society for Cardiology. Fighting cardiovascular disease.A blueprint for EU action.
- 11.Alghamdi A S, M A. (2021) A Community-Based, Cross-Sectional Study Assessing the Level of Awareness and Insight Related to Cardiovascular Diseases.Cureus.13(6).
- 12.Mohammad N, Muhamed B, Rahman N, Ramarhan A, Haque M et al. (2018) Knowledge, attitude, and practice regarding the risk of cardiovascular diseases in patients attending outpatient clinic in Kuantan. , Malaysia.J Pharm Bioall Sci 10, 7-14.
- 13.Ashley k Keates, O A. (2017) Cardiovacular disease in Africa: epidemiological profile and challenges.Macmillan.
- 14.Boateng D, F-B-G W. (2017) Knowledge and awareness of and perception towards cardiovascular disease risk in sub-Saharan Africa: A systematic review.Journal pro. 12-12.
- 15.Nyirahabimana M Vestine. (2017) Knowledge and preventive practice regarding cardiovascular diseases risk factors among rural population at a selected District in Rwanda.University of Rwanda.
- 17.Farah R, B M Irfan. (2016) . Risk Factors of Cardiovascular Disease in Developing Countries.International Current Pharmaceutical Journa 5(8), 69-72.
- 18.Saiari A. (2015) Guidelines for Providing Prevention and Control of NonCommunicable Diseases in Primary Health Care System, IraPEN protocol, Non-physician (midwife) pamphlet.Minist Health Med Educ.
- 19. (2020) Rwanda Demographic and Health Survey. Rwanda Demographic and Health Survey 2019-2020.Key Indicators Report.RwandaDHS.
- 20.Lwanga S, Lemeshow S. (1991) size determination in health studies: A practical manual, 1991.Geneva: World Health Organization.
- 21.Juma P, Adbou A, Mohamed S, Faradje Y, Matanje B et al. (2018) Non-communicable disease prevention policy process in five African countries authors.BMCPublic. , Health 18, 961.
- 22.Joshi C, Jayasinghe U, Jaysinghe W, Parker S, Joysua K et al. (2014) Does health literacy affect patients’ receipt of preventative primary care? A multilevel analysis.BMC Fam Pract.
- 23.Lim S, Beauchamp A, Dodson S, Beausejour M, Brandon H et al. (2017) Health literacy and fruit and vegetable intake in rural Australia.Public Health. , Nutr 20, 2680-4.
- 24.Sørensen K, Broucke S Van den, Fullam J, Friedrich K, Burg L Van der et al. (2012) Health literacy and public health: a systematic review and integration of definitions and models.BMC. , Public Health 12, 80.
- 25.Burger A, M C Fourie. (2016) The relationship between cardiovascular risk factors and knowledge of cardiovascular disease. in African men in the north-West Province.Health SA Gesondheid 21(1), 364-71.
- 26.Toupchian O, Abdollahi S, Samadi M, Touchan P, Abdallah K et al. (2016) Knowledge and attitude on cardiovascular disease risk factors and their relationship with obesity and biochemical parameters.Journal Of Nutrition And Food Security. , (JNFS) 1(1), 63-72.
- 27.Mohammed J. (2012) Knowledge of, and Attitude to Cardiovascular Disease Risk Factors Among Members Of The Nigerian Armed Forces.World. , J Public Heal Sci 11(2), 23-7.
- 28.Oladapo O, Oedraogo O, Salako L, Sadiq L, Nuanko H et al. (2013) Knowledge of hypertension and other risk factors for heart disease among Yoruba rural southwestern Nigerian population.JAMMR. 3, 993-1003.
- 29.Aminde L, Amad N, Takah N, Ngwasiri C, Ngweso G et al. (2017) Population awareness of cardiovascular disease and its risk factors in Buea. , Cameroon.BMC Public Health 17, 545.
- 30.Shafiq. (2017) Public knowledge of cardiovascular diseases and its risk factors in. , Srinagar.International Journal of Medical and Health Research 3(12), 69-76.
- 31.Awad A, Al-Nafisi H. (2014) Public knowledge of cardiovascular disease and its risk factors in Kuwait: a cross-sectional survey.BMC. , Public Health 14, 1131.
- 32.Güneş F, Jurgen E, Bekiroglu N, Imeryuz N, Carnoghrou H et al. (2019) Awareness of cardiovascular risk factors among university students. in Turkey.Primary Health Care Research & Development, 20(e127): 1-10.
- 33.Manisha S, Prajjwal P, Kamlesh P, Sweta S, Soumya P et al. (2020) Knowledge, Attitude and Practices regarding Cardiovascular Diseases among people of Pakhribas municipality of. , Eastern Nepal.Nepalese Heart Journal 17(1), 33.
- 34.Rosediani M, Ranimah Y, Harmy M, Mamdhan Y, Hamza K et al. (2017) . Knowledge, Attitude and Practice on Cardiovascular Disease among Women in North-East coast Malaysia.International Journal of Collaborative Research on Internal Medicine & Public Health 4(1), 85-98.
- 35.Baha M, A-L Le Faou. (2019) Attitude towards cessation among French pregnant smokers: Explaining the poor uptake of specialised support.European. , Journal of Obstetrics & Gynecology and Reproductive Biology 147(1), 46-51.
- 36.Kim C, Beckles G. (2014) Cardiovascular disease risk reduction in the Behavioral Risk Factor Surveillance System.American. , Journal of Preventive Medicine 27(1), 1-7.
Cited by (1)
- 1.Taghian Gabriella, Fisher Samantha, Chiles Thomas C., Binagwaho Agnes, Landrigan Philip J., 2024, The Burden of Cardiovascular Disease from Air Pollution in Rwanda, Annals of Global Health, 90(1), 10.5334/aogh.4322