Abstract
Objective
To identify common ocular and non-ocular signs and symptoms of patients with chiasmal lesions presenting to ophthalmologists.
Methods
This is a three year case series of patients who presented to Rizal Medical Center Ophthalmology OPD clinic, diagnosed as cases of chiasmal lesion with a complete neuro-ophthalmogical exam, ancillary test and neuroimaging. Data collected include patient profile, ocular and non ocular symptoms, duration of blurring of vision (BOV), best corrected visual acuity (BCVA), Color Vision, Optic nerve (ON) description, Visual field defects (VFD) and size & location of chiasmal lesion.
Results
A total of twelve patients were included with 1:1 M:F ratio and a median age of 39 years. Blurring of Vision was the presenting symptom in 10 cases, bulging of the eyes and headaches in the remaining cases. Associated symptoms include: non specific headache in all; diplopia in 3 (1 with and 2 without motility defects); and systemic symptoms related to hormonal imbalance in 2 cases.
Best corrected vision ranged from 6/6 to no light perception (NLP). Color vision was affected in all cases. ON palor was seen in 6 (50%) and disc edema in 1 case. VFD include Junctional scotoma (58.33%), bitemporal hemianopia (33.3%) and generalised scotoma (8.3%). Neuroimaging revealed pituitary lesions in 10 cases, 1 craniopharyngioma and ON glioma with chiasmal extension.
Conclusion
Ocular and non ocular symptoms seen were comparable to other studies except that Junctional scotoma was the most common VFD identified in the included population of our case series. This highlights the importance of VF testing among patients complaining of unilateral visual loss to rule out a chiasmal lesion.
Author Contributions
Academic Editor: Samir Sutar, C L Gupta eye institute Research associate, India.
Checked for plagiarism: Yes
Review by: Single-blind
Copyright © 2020 Aishath Jeneena Amir, et al.
 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Competing interests
The authors have declared that no competing interests exist.
Citation:
Introduction
As Ophthalmologists we see majority of patients with main complaint of BOV of various etiologies. BOV can also be a symptom of a more serious problem, including a potentially sight threatening disease or neurological disorder such as an intracranial mass. According to a local study done by de Roxas, the three most common sites of brain tumor were frontal lobe (33.6%), parietal lobe (14.5%) and sellar region which accounted for 11.1% of all intracranial neoplasms.1Since mass in the sellar region is not uncommon, this is one area where ophthalmologists can help patients by reaching an early diagnosis.
The Chiasm and Manifestations of Chiasmal Lesions
The Optic chiasm is an essential structure to vision, located in the anterior inferior recess of the third ventricle. Fibers from the nasal half of the retina decussate in the chiasm and join the uncrossed temporal fibers of the retina to form the optic tract giving characteristic visual field defects that respect the vertical horizon2. The etiology of chiasmal lesions varies from congenital, traumatic, iatrogenic causes to extrinsic or intrinsic lesions. The most common intrinsic lesion is the pituitary adenoma which may promote compression of the optic chiasm causing visual disturbances.3
Ocular Symptoms of Chiasmal Lesions
In a retrospective study done by Kitthaweesin et al.4, the ocular manifestations documented among patients with suprasellar tumors were visual loss (86%), eye pain (9%), diplopia (4%), and ptosis (1%). Ocular signs including relative afferent pupillary defect was detected in 31 patients (45%) and optic disc atrophy in 26 patients (38%). The most commonly encountered VFD was bitemporal hemianopia (49%), 14% had quadrantanopia and 7% with a 3 or greater quadrant loss of visual field.
Signs of chiasmal injury include a characteristic pattern of optic atrophy called “band” optic atrophy. Optic disc atrophy occurs over weeks to months, and the absence of optic atrophy should not preclude additional evaluation of patients with visual loss5. Additional effects could arise from compression of adjacent structures such as extension of the mass to the cavernous sinus causing disorders of extra ocular motility.
Nystagmus may occur in patients with suprasellar tumors. See-saw nystagmus is an uncommon form of nystagmus with a finding of an alternating elevation and intorsion of one eye along with depression and excyclotorsion of the other eye.6
Non-Ocular Symptoms of Chiasmal Lesions
Most common non ocular manifestation of chiasmal syndrome include headache and systemic signs secondary to hormonal imbalance.
Epilepsy can occur under circumstances similar to cranial nerve lesions, and its frequency was reported by Poppen (1963)7pre-operatively with an incidence of 1-7%. If hemorrhage into a pituitary tumor occurs, that is, pituitary apoplexy, patients may present with varying combinations of sudden onset of severe headache, cranial neuropathy, visual impairment, and hypopituitarism. If very large, pituitary tumors may cause hydrocephalus and signs of increased intracranial pressure8.
Objectives of the Study
Primary objective is to determine the common clinical symptoms and signs of patients with chiasmal lesions.
Specific Objectives Include:
1. To identify ocular and non-ocular symptoms among patients diagnosed with chiasmal lesions presenting to our OPD clinic.
2. To describe visual field defects seen among this group.
3. To compare size of lesion as documented on neuroimaging studies to the signs and symptoms of the patients.
Significance of the Study
At present, there is limited information available on chiasmal lesions presenting to ophthalmologists and this would be the first local study done. The results of this study may contribute to the diagnostic approach for patients with blurring of vision presenting to ophthalmologists.
Ethical Considerations
This study was approved by IRB ethics committee of Rizal medical center in November 2018 and followed the tenets of declaration of Helsinski. The examinations and testing done were fully explained to the patients and each provided informed written consent. Each patient was informed that all data gathered in relation with the study is confidential and will be used exclusively for purposes of the study only.
Methods
This is a case study of patients presenting to the Rizal Medical Center Eye Training and Facilities Center Outpatient clinics from May 2016 to July 2019, diagnosed to have chiasmal lesion by ophthalmologists with history, complete neuro-ophthalmologic exam, ancillary test and neuroimaging studies that gave their consent to participate in this study. Patients may either be walk-in to the eye center or as referral from departments within the hospital or from outside institutions.
Data collected include patient profile (age, sex, occupation, systemic condition), chief complaint, ocular and non-ocular symptoms, duration of blurring of vision, best corrected visual acuity, color vision using ishihara color plates, ocular motility, optic nerve description, visual field defects (by confrontation and automated perimetry) and size and location of chiasmal lesion as measured in either cranial CT scan or MRI as seen in table 1
Table 1. Checklist of signs and symptoms of chiasmal lesions.The patients were checked for the following signs and symptoms.
Results
12 patients were included from May 2016 to July 2019, with 1:1 M:F ratio and a median age of 39 years (SD 17.81), mostly as walk-in with only two (16.67%) referred already with a diagnosis of chiasmal syndrome.
Summary of Cases
A total of 12 patients diagnosed with Chiasmal lesions were included in this case series with a mean age of 39 years (10 to 62 years). We had 6 females and 6 male in this study, thus a 1:1 M:F ratio.
Table 2 summarises the patient demographics. Most of these patients were walk in to the RMC Eye Training & Facilities Center (83.33%) and 3 were referrals from the other clinical departments (Internal Medicine, General Surgery, Neurosurgery). 2 out of the 8 walk in patients were initially evaluated by other ophthalmologic subspecialty (Glaucoma, Oculoplastic, lacrimal & orbits) before being referred to the Neuro-ophthalmology service. In most of the cases, diagnosis was performed in our eye center and in only 2 cases, diagnosis were already known prior to consultation at the ophthalmology department as seen in table 3
Table 2. Patient Demographics of the 12 cases| Case No. | Age in years | Gender | Patient Type (Walk in or Referral) | Occupation |
| 1 | 51 | F | Walk in | Housewife |
| 2 | 53 | M | Walk in | Vendor |
| 3 | 31 | F | Walk in (Glaucoma) | Housewife |
| 4 | 53 | F | Referral from Internal medicine | Housewife |
| 5 | 42 | F | Walk in | Housewife |
| 6 | 62 | M | Walk in | Driver |
| 7 | 38 | F | Walk in | Housewife |
| 8 | 10 | M | Walk in | Student |
| 9 | 51 | F | Walk in | Housewife |
| 10 | 18 | M | Referral from General Surgery | Student |
| 11 | 55 | M | Walk in (Oculoplastic) | Driver |
| 12 | 13 | M | Referal from Neurosurgery | Student |
| Mean: 39 yrs; Mode: 53 yrs; Range:10-62; 1:1 M:F ratio | ||||
| Case No. | Symptoms | BCVA | Visual Fields by Confrontation | Optic nerve | Color Vision (Ishihara Plates identified) | Pupils | EOMs | ||
| Ocular | Non Ocular | ||||||||
| 1 | BOV Left> RightBinocular diplopia (all gazes) | Non specific headache | R | 6/38 | No fields identified except nasal hemifields righteye | Diffuse ON pallor, CDR 0.5 | 0 | 2-3 mm BRTL | Full |
| L | LP | Diffuse ON pallor, CDR 0.5 | 0 | 2-3 mm BRTL | Full | ||||
| 2 | BOV right eye for 7 months | Non specific headache | R | HM with GLPj | No fields identified except nasal hemifields left eye | Slightly pale ON, CDR 0.5 | 6/15 | +2 RAPD | Full |
| L | 6/6 -1 | Unremarkable | 8/15 | 2-3 mm BRTL | Full | ||||
| 3 | BOV both eyes for 12 months | Non specific headache | R | HM with GLPj | No fields identified except superonasal quadrant of left eye | Diffuse Optic palor | 0 | 2-3 mm BRTL | Full |
| L | HM with PLPj | Diffuse Optic pallor | 0 | + 2 RAPD | Full | ||||
| 4 | BOV left > right for 3 months | Headache with dizziness | R | 6/38 | No fields identified except for nasal hemifields of right eye | Optic disc palor | 0 | 2-3 mm BRTL | Full |
| L | HM with PLPj | Optic disc palor | 0 | + 2 RAPD | Full | ||||
| 5 | Loss of vision of right eye and BOV left for 6 months | Headache | R | NLP | No fields identified except for nasal hemifields of left eye | Unremarkable | 0 | +4 RAPD | Full |
| L | 6/10 | Unremarkable | 0 | 2-3 mm BRTL | Full | ||||
| 6 | BOV both eyes for 12 months ( unable to see signboard while driving | Headache | R | 6/20 | Nasal hemifields of both eyes identified | Unremarkable , CDR 0.5 | 8/15 | 2-3 mm BRTL | Full |
| L | 6/20 | Unremarkable , CDR 0.5 | 5/15 | 2-3 mm BRTL | Full | ||||
| 7 | BOV left eye for 11 months ( gradually progressive) | Headache | R | 6/6 | No fields identified except for nasal hemifield of left eye | Unremarkable | 15/15 | 2-3 mm BRTL | Full |
| L | PLPj | Temporal disc palor | 0/15 | +4RAPD | Full | ||||
| 8 | Proptosis right eye followed by BOV of right eye for 6 months | Headache | R | 1/60 | No fields identified except for nasal hemifield and inferotemporal quadrant of left eye | Temporal disc palor | 0/15 | +4RAPD | Full |
| L | 6/6 | Unremarkable | 15/15 | 2-3 mm BRTL | Full | ||||
| 9 | BOV Right eye for 12 monthsBinocular diplopia ( all gazes) | Frontal headache | R | 6/15 | Only nasal hemifields of both eyes identified | Unremarkable | 2/15 | 2-3 mm BRTL | Full |
| L | 6/6 | Unremarkable | 6/15 | 2-3 mm BRTL | Full | ||||
| 10 | BOV right > left eye for 24 months | Non specific headache | R | LP | Only nasal hemifield of left eye was identified | Pale ON | 0/15 | + 2 RAPD | Full |
| L | 6/15 | Unremarkable | 4/15 | 2-3 mm BRTL | Full | ||||
| 11 | Bulging of both eyes ( 7 months)BOV right (5 months)Binocular diplopia | Headache | R | 6/7.5 | Only nasal hemifieds of both eyes identified | Unremarkable | 12/15 | 2-3 mm BRTL | Limitation of -2 in all gazes except -3 in downward gaze |
| L | 6/12 | Unremarkable | 13/15 | 2-3 mm BRTL | |||||
| 12 | BOV both eyes for 3 months | Frontal headache (throbbing) | R | 6/6 | Only nasal hemifieds of both eyes identified | Indistinct disc borders | 12/15 | 2-3 mm BRTL | Full |
| L | 6/6 | Indistinct disc borders | 13/15 | 2-3 mm BRTL | Full | ||||
Ocular and Non Ocular Symptoms
Majority of patients (11 of 12 cases) primarily complained of ocular problems such as BOV and bulging of the eye. BOV was the presenting symptom in 10 cases, while proptosis and headaches were the main complain in the remaining cases. Associated symptoms include: Headache in all; diplopia in 3 (1 with and 2 without motility defects); and systemic symptoms related to hormonal imbalance in 2 cases as seen in table 4
Table 4. Ocular and Non Ocular Symptoms| Symptoms | Number (n=12) | Percentage | |
| Ocular Symptoms | |||
|---|---|---|---|
| 1 | Blurring of Vision | 12 | 100% |
| 2 | Diplopia (Binocular) | 3 | 25% |
| Non-Ocular Symptoms | |||
| 1 | Headache | 12 | 100% |
| 2 | Systemic symptoms secondary to hormonal imbalance (Cushings syndrome, TED) | 2 | 16.66% |
Ocular Signs and Physical Examination
Blurring of Vision was a complaint in all patients noted in an average of 14.75 months in duration prior to consultation (range of 5-60 months). Bilateral blurring of vision was observed in 8 cases (66.67%) and was unilateral in the remaining. The BOV was asymmetrical in 9 cases (75%). All patients experienced a gradually progressive BOV but most (10/12) poorly described this symptom in terms of involved location, except in 2 cases. A driver who was able to note temporal field loss described as inability to see sign boards on the sides of the streets and sudden appearance of cars which was not in view before, while the other one was a housewife who noticed missing the temporal sides of her vision.
The best corrected visual acuity ranged from 6/6 to hand movement with poor light projection of the better eye, and the poorer eye from 6/12 to no light perception. Relative afferent pupil defect was detected in 7 cases out of 9 cases with asymmetrical visual acuity.
Visual Field defects identified by performing confrontation testing were Junctional scotoma in 7 cases, bitemporal hemianopia in 4 cases and Generalized visual field defect in 1 case.
Diplopia was an ocular symptom observed in 3 cases (25%). In one case, there was a ocular motility defect in all gazes while in 2 cases no ocular motility defect was noted. The case of restrictive ophthalmoplegia from thyroid orbitopathy was a referral from the Oculoplastic, lacrimal and orbit service who had an incidental pituitary macroadenoma noted on imaging.
Dyschromatopsia as tested using Ishihara color plates, was identified in all 12 cases (100%). Considering 24 eyes, in only 2 eyes were all the ishihara plates identified, while in most (22 eyes) 5 plates were missed on the average (0 to 13 plates identified).
Diagnostics
Automated Visual Field perimetry in all 12 cases of chiasmal le-sions revealed similar output as confrontation testing. Junctional scotoma was seen in 7 cases, bitemporal hemianopia in 4 cases and Generalized scotoma in 1 case. There was no atypical visual field defects such as peripheral constriction or homonymous hemianopia encoun-tered in this study.
The average Mean Deviation of 22 eyes is 21.79dB (8.3 to 38.45dB). Majority of eyes had MD of more than 10 dB as seen in table 5
Table 5. Summary of AVF Perimetry Mean Deviation of 21 eyes included| Mean Deviation | Number of eyes | Average MD |
| 0 to 10 | 3 | 9.3 dB |
| >10 to 20 | 5 | 14.7 dB |
| >20 to 30 | 12 | 25.5 |
| >30 to 40 | 2 | 35.92 |
It is notable that in this case series a higher number of patients with junctional scotoma was observed compared to the bitemporal hemianopia cases in other studies 29,30
Neuroimaging
Neuroimaging(Cranial MRI or CT Scan)revealed pituitary lesions in 9 cases, two (2) cases of craniopharyngioma and Optic nerve glioma with extension to the chiasma.
The size of chiasmal lesions was measured in neuroimaging in dimensions and computed in volume using the Cavalieri’s principle. Mean volume of mass in 12 cases was 25.46cm3 (6.89 to 98.55cm3). Pituitary lesions (n = 9) have a mean size of 11.3cm3 (6.89 to 67.30cm3), Craniopharyngioma cases are larger at 38-98.55cm3 and the Optic nerve glioma with extension to the chiasma at 11.30cm3 as seen in table 6
Table 6. Neuroimaging studies, Lesion size in dimensions and computed volume of 12 included cases| Case No. | Radiologic etiology of chiasmal lesion | Neuroimaging modality | Lesion Size | |
| In dimension(in cm) | Volume(in cm3) | |||
| 1 | Pituitary Adenoma | CT Scan | 3.1 x 2.4 x 2.9 | 11.30 |
| 2 | Pituitary Adenoma | MRI | 3.0 x 2.0 x 2.5 | 7.85 |
| 3 | Pituitary Adenoma | MRI | 4.0 x 3.0 x 2.5 | 15.71 |
| 4 | Pituitary Adenoma | MRI | 3.2 x 2.0 x 2.8 | 9.38 |
| 5 | Pituitary Adenoma | CT Scan | 4.3 x 6.1 x 4.9 | 67.30 |
| 6 | Pituitary Adenoma | MRI | 2.8 x 2.6 x 2.2 | 8.39 |
| 7 | Pituitary Adenoma | MRI | 2.3 x 2.6 x 2.2 | 6.89 |
| 8 | ON glioma with chiasmal extension | MRI | 3.1 x 2.4 x 2.9 | 11.30 |
| 9 | Pituitary Adenoma | MRI | 3.0 x 3.3 x 4.0 | 20.73 |
| 10 | Craniopharyngioma | MRI | 5.5 x 5.9 x 5.8 | 98.55 |
| 11 | Pituitary Adenoma | MRI | 3.1 x 2.5 x 2.5 | 10.14 |
| 12 | Craniopharyngioma | CT | 5.4 x 3.2 x 4.2 | 38.00 |
Discussion
Patient Profile
A retrospective study done by Astorga-Carballo et al9 with a larger population than ours (n = 104) observed a slight female predominance (1:1.47) and a median age of 52 years (4-86 years) among patients with diagnosis of chiasmal syndrome attending their ophthalmological institution. In our case series, the mean age is 39 years, with a 1:1 M:F ratio.
Most walk in patients to our Eye center had blurring of vision in the average of around 16 months prior to consultation (6 to 60 months), while those referred from other services noted BOV earlier at around 10 months prior to referral (3-24 months) as seen in table 7
Table 7. Patient type (walk in or referral) and relation to blurring of vision duration in months| Case No. | Patient Type (Walk in or Referral) | Duration of BOV (in months) |
| Referrals from Clinical departments other than Ophthalmology | ||
| 12 | Neurosurgery | 5 |
| 10 | General Surgery | 24 |
| 4 | Internal medicine | 3 |
| Average | 10.67 | |
| Walk In to Eye Center/ Subspecialty Service | ||
| 1 | Neuro-Ophthalmology | 60 |
| 2 | Neuro-Ophthalmology | 7 |
| 5 | Neuro-Ophthalmology | 6 |
| 6 | Neuro-Ophthalmology | 12 |
| 8 | Neuro-Ophthalmology | 6 |
| 9 | Neuro-Ophthalmology | 12 |
| 7 | Neuro-Ophthalmology | 11 |
| 3 | Glaucoma | 24 |
| 11 | Oculoplastic, Lacrimal & Orbit | 7 |
| Average | 16.11 | |
Ocular Signs and Symptoms
Irrespective of etiology of mass, blurring of vision was the main complaint in 10 of our 12 cases, involving one or both eyes. This main complaint was associated with headache in all cases, diplopia in 3 (25%)and symptoms secondary to hormonal imbalance in 2 (16.66%).
Chiasmal syndrome can have a variety of clinical manifestations with low vision as the initial presentation in most cases1,3. In our case series, most complained of asymmetrical, gradually progressive blurring of vision in both eyes, often poorly described in the aspect of involved location except in 2 cases.
The duration of BOV prior to consultation among this set of patients was 14.75 months on the average, which is delayed compared to other studies at 12 months (4 days to 5 years)4, which is probably the reason for advanced disease at presentation. Considering that among these cases, patient may consult late in onset when macular fibres become affected, since an early peripheral field defect usually goes unnoticed by patients.10Also, having a good vision in one eye may have precluded consulting earlier.
The best corrected visual acuity (BCVA) of 24 eyes ranged from 6/6 to NLP. Bilateral blurring of vision was observed in 8 cases (66.67%) and was asymmetrical in 9 cases (75%) with corresponding relative afferent pupillary defect, in accordance to a study done by Jonathan et al.11
Visual Field defects were intially identified by performing confrontation testing which corresponded well with AVF perimetry results. According to Lenworth et al12, sensitivities for confrontation testing for posterior visual field defects, were high for detecting homonymous hemianopsias at 76% (19 of 25) and junctional scotomas at 75%, but low for bitemporal hemianopsias at 50% (6 of 12). This low sensitivity might have occurred because these visual field defects were often relative rather than near absolute scotomas.
Dyschromatopsia as tested using Ishihara color plates was seen in all cases (100%), involving 22 eyes. This is higher compared to a study by Astorga9, affecting only 62.5% of their cases, which probably is due to the fact that most of the patients presented in the late course of the disease.
Diplopia was an ocular symptom observed in 3 cases (25%). 1 case was restrictive ophthalmoplegia and 2 cases were not associated with any ocular motility defect. These 2 nonparetic diplopia cases have related VFD of bitemporal hemianopia and junctional scotoma, which resulted to retinal hemifield slide.13,14
There were no complaints of eye pain or problem in depth perception.
Optic nerve was described as unremarkable in 12 eyes (50%), pale (diffuse or temporal pallor) in 10 eyes (41.67%), and was swollen in 2 eyes (8.33%). This finding was slightly different with others, that Optic nerve palor was observed frequently (63% to 64.4%) among patients with perichiasmal tumors10,12. This may be due to the more asymmetrical involvement in our cases. The 2 eyes with swollen optic nerves was found in a patient with a large chiasmal mass associated with supratentorial hydrocephalus with moderate transependymal edema, which can be considered as an unusual manifestation of a chiasmal mass15.
In all 12 cases, Junctional scotoma was the most common (58.33%) visual field defect reported using the Automated Visual Field Perimeter, followed by bitemporal hemianopia (33.3%) and Generalized scotoma in 1 case. This is different with other studies citing bitemporal hemianopia as the most frequent VFD observed1,13,14,16. 7cases (77.78%) presenting with asymmetrical BOV had a VFD of Junctional scotoma and 2 with bitemporal hemianopic defect in Automated Visual Field Perimetry. There was no atypical visual field defects such as peripheral constriction or homonymous hemianopia encountered in this study.
Considering only the Pituitary adenoma cases (n=9), Junctional scotoma was the mostly observed VFD (5 cases), bitemporal hemi-anopsia in 3 cases and one case with generalized depression. This is different with other studies citing bitemporal hemianopia as the most frequent VFD observed among those observed with pituitary adenoma cases 14, 16.
Non-Ocular Manifestations
Headache is the most common non-ocular manifestation seen in all 12 of our cases. It was described as non-specific in character that is mild to severe in intensity in most cases. Headache among patients with brain tumors was described by Kirby et al17, as intermittent, moderate to severe in intensity with variable character described as dull, aching, throbbing or shooting and usually more severe in the morning. Headache is a common manifestation of brain tumor according to a local study1, occurring in 39.1% of patients. Among patients with chiasmal syndrome, headache was the presenting symptom of 10 patients among 104 studied (9.61%). In our case series, headache was the main complaint in only 1 case, but was an associated symptom in all the remaining cases. This was expected since they are presenting to ophthalmologists.
In a 15 year retrospective study done in Jamaica by Cawich et al18, nonspecific headaches accounted the most (72.3%) common clinical manifestation of pituitary adenoma, with cranial nerve palsies (16%) and pituitary apoplexy (5%). These, however, were not observed in any of the 12 cases in this case series.
Etiology
Pituitary adenoma was the most considered etiology of chiasmal lesion on this case series (75%) based on neuroimaging, which is similar to those found in the literature regarding chiasmal lesions3,16,19. Pituitary adenoma accounts for 12-15% of all intracranial neoplasms and it is estimated that 25% of the population have pituitary adenoma, most of which are incidentally found.20
Table 8 summarises the common causes of Lesions affecting the chiasm including extrinsic and intrinsic causes.
Table 8. Common causes chiasmal syndromeEight (8) patients included in this study, radiologically considered with pituitary adenoma had an average age of 44.5 years (range of 31-61 years old) that is similar with findings of other studies (mean age of 43-51 years14,21) and a female preponderance of 1:3.5 M:F ratio, no different to other studies (1:2, 1:3.8)14,21
Apart of pituitary adenomas the rest of our cases (25%) were in paediatric age group (range of 10-18 years). Craniopharyngioma was the etiology in 2 cases (16.67%) and Optic nerve glioma with chiasmal extension in one. These etiologies other than pituitary adenoma were also among the common etiologies reported in other studies affecting the chiasm 3,12,16,19,22
Craniopharyngiomas constitute to 5-10% of tumours of childhood23. Craniopharyngioma accounts for 56% of sellar and suprasellar tumors in children24.Our 2 cases of Craniopharyngioma have an average age of 15.5 years (13-18), similar to the results of a retrospective study of 45 patients by Kennedy et al25, wherein more than half presented in the first two decades of life. The US-Central Brain Tumor Registry of the United States (CBTRUS), observed a bimodal age of distribution: one in childhood (0-1924, 5-1426years) and in adulthood (45-8424, 50-7526years), higher peak for ages 65-7428.
The chiasm was secondarily involved in the case of a 10 year old boy diagnosed with neurofibromatosis type 1 (NF1) with an optic nerve glioma. He presented later than what was reported in the literature at 627 to 8.828 years. This case was similar to those described in a chart review study by Segal27, wherein nearly a third (36%) of NF1 patients with Optic nerve glioma (13% of the 331 NF1 patients) presented past the age of 6 years and 18% are symptomatic (decreased vision or precocious puberty) demonstrating chiasmal or retrochiasmal tumor in addition to nerve involvement.
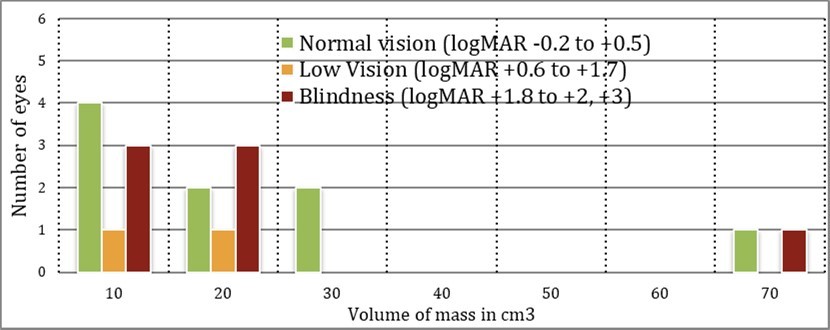
Size of Lesion, BCVA and Visual Field Defect
The largest mass measuring 98.55cm3and the smallest mass measuring 6.89cm3both had a BCVA of the poorer eye (>2 logMAR units). Also, the largest mass had one eye with normal vision showing the asymmetrical visual involvement. (see table 9).
Table 9. BCVA (in logMAR) of 24 eyes classified to Normal, Low Vision and Blindness in relation to size of lesion in cm3Mean deviation (MD) from Automated Visual Field Perimetry performed were gathered only from 22 eyes. The Average mean deviation of 22 eyes is 21.79 dB, with majority having a MD above >10 and <40dB (19 eyes). There are only 3 eyes with mean deviation less than 10 dB (see Table 10).
Considering AVF perimetry Mean Deviation and size of the lesion (in cm3), an eye of the patient with a large lesion (67.30cm3) had a MD of <10 dB, while an eye with MD of more than 30 dB had a small lesion (6.89cm3).
Table 10. AVF Perimetry Mean Deviation (in dB) of 22 eyes in relation to volume of lesion in cm3Table 11 summarizes MD of 22 eyes with size of lesions. Our results does not support studies regarding severity of VFD and visual loss in relation to tumor size. This maybe explained by the higher number of patients with junctional scotoma in this series compared to the bitemporal hemianopia cases in previous studies29,30.
To further compare size of lesion with BCVA in LogMAR and AVF Perimetry, non pituitary lesions were excluded as seen in table 12 and table 13. Majority of the cases (16 eyes) have pituitary lesions with volume measuring less than 20 cm3. The largest pituitary lesion volume measured at 67.3 cm3, had one eye with vision classified to be in the normal range, whereas the other eye was blind. This asymmetry was also seen in the group with pituitary lesions measuring less 20 cm3 (16 eyes), with equal number of eyes with normal vision and blindness (7 eyes each).
Table 11. AVF Perimetry Mean Deviation of 22 eyes in relation to Volume of lesion (in cm3)| Mean Deviation | Number of eyes | Average MD | Lesion Size (in cm3) | ||
| Average Volume | smallest | largest | |||
| 0 to 10 | 3 | 9.3 dB | 36.25 | 20.73 | 67.30 |
| >10 to 20 | 5 | 14.7 dB | 20.93 | 8.39 | 38.0 |
| >20 to 30 | 12 | 25.5 dB | 29.74 | 6.89 | 98.55 |
| >30 to 40 | 2 | 35.92 dB | 9.10 | 6.89 | 11.30 |
| Pituitary Lesion Volume (cm3) | Number of eyes | Average MD(in dB) | AVF Perimetry Mean Deviation | |
| lowest | highest | |||
| 0 to 10 | 8 | 24.60 | 17.10 | 33.40 |
| >10 to 20 | 6 | 23.59 | 11.70 | 38.45 |
| >20 to 30 | 2 | 9.10 | 8.30 | 9.90 |
| >30 | 2 | 18.45 | 9.80 | 27.1 |
The average AVF Perimetry MD of the 18 eyes with pituitary lesion is 21.86 dB, with the majority of eyes (14 eyes) having an average MD higher than 20 dB, as shown in table 13. The eyes with lesion measuring more than 30cm had the lowest average AVF Perimetry MD as compared to lesions measuring smaller than 20 cm3, not supporting the findings in other studies.29, 30
Conclusion
Ocular and non ocular symptoms seen were comparable to other studies except that Junctional scotoma was the most common VFD identified in the included population of our case series. This highlights the importance of VF testing among patients complaining of unilateral visual loss to rule out a chiasmal lesion.
Study Limitation
Except for one case, most of the cases collected as chiasmal mass would not have histopathological confirmation and classification of the type of mass. There are no statistical test done to correlate tumor vol-ume with logMAR BCVA or AVF Perimetry MD. Also, stereo acuity was not determined in this study.
References
- 1.R De, Pedro K, Rivera J, Batara J M. (2017) Current treatment status of adult brain tumors in the Philippine general hospital. , J Neurol Neurorehabil Res 2(1), 7-13.
- 2.Levin L.Clinical Neuro ophthalmology, Topical diagnosis of chiasmal and retrochiasmal lesions. , Chapter 12.
- 3.Wadud S A, Ahmed S, Choudhury N, Chowdhury D.Evaluation of ophthalmic manifestations in patients with intracranial tumours.
- 4.Kitthaweesin K, Ployprasith C. (2008) Ocular Manifestations of Suprasellar Tumors. , J Med Assoc Thai.91-5
- 5.Kirkham T H.The Ocular Symptomatology of Pituitary Tumours. (The National Hospital. , Queen Square, London WCJ
- 6.Unsold R, Ostertag C. (2002) Nystagmus in suprasellar tumors: recent advances in diagnosis and therapy. , Strabismus 10, 173-177.
- 8.Hollenhorst R W, Younge B R. (1973) Ocular manifestations produced by adenomas of the pituitary gland: analysis of 1000 cases. In:KohlerPO,RossGT,editors.Diagnosis and treatment of pituitary tumors. , Amsterdam: Excepta Medica 53-63.
- 9.Astorga-Carballo A, Serna-Ojeda J C, Camargo-Suarez M. (2017) Chiasmal syndrome: Clinical characteristics in patients attending an ophthalmological center by Saudi. , Journal of Ophthalmology 31, 229-233.
- 11.Jonathan D, Trobe J D, Tao A H, Schuster J J. (1984) Perichiasmal Tumors: Diagnostic and Prognostic Features. , Neurosurgery 15(3), 391-399.
- 12.Johnson L, Baloh F.The accuracy of confrontation visual field test in comparison with automated perimetry.University of Missouri-Columbia Mason Eye Institute. , Columbia, MO65212.Hershey,Pennsylvania
- 13.Peragallo J H, Bialer O Y, Pineles S L, Newman N J.Hemifield Slide Phenomenon as a Result of Heteronymous Hemianopia. , Neuro-Ophthalmol 38, 82.
- 14.S G Elkington. (1968) Pituitary adenoma. Preoperative symptomatology in a series of 260 patients. , Br. J. Ophthalmol 52, 322-328.
- 15.Dhar M, Pehere N.. , Unusual Visual Manifestations of Pituitary Tumours.Kerala Journal of Ophthalmology.Vol.XIX 2.
- 16.Schiefer U, Isbert M, Mikolaschek E, Mildenberger I, Krapp E et al. (2004) Distribution of scotoma pattern related to chiasmal lesions with special reference to anterior junction syndrome. Graefes Arch Clin Exp Ophthalmol. 242(6), 468-77.
- 18.Crandon I Cawich, Harding H, McLennon H.Clinical presentation of patients with pituitary adenoma at a university hospital. in Jamaica.Jan1989-June2005
- 19.Tagoe N N, Essuman V A, Fordjuor G, Akpalu J, Bankah P et al. (2015) Neuro-Ophthalmic and Clinical Characteristics of Brain Tumors in a Tertiary Hospital in Ghana. , Ghana Med J.Sep 49(3), 181-6.
- 20.Vasenwala S M, Ansari H, Basari R, V K Srivastava. (2014) Pituitary adenoma: A case report with special emphasis on 2 approach to diagnosis. , Clin Cancer Investig J 3, 264-7.
- 21.Kasputytė R, Slatkevičienė G, Liutkevičienė R, Glebauskienė B, Bernotas G et al.Changes of Visual Functions in Patients With Pituitary Adenoma.
- 22.Mejico L, Miller N, Dong L M. (2004) Clinical Features Associated with Lesions other than Pituitary adenoma in patients with an Optic Chiasmal Syndrome. , American Journal of Ophthalmology.May 137(5), 908-913.
- 26.Bunin G R, Surawicz T S, Witman P A, Preston-Martin S, Davis F et al. (1998) descriptive epidemiology of craniopharyngioma. , J Neurosurg 89(4), 547.
- 27.Segal L.Darvish-Zargar M,Dilenge ME,Ortenberg J, Polomeno RC.Optic pathway gliomas in patients with neurofibromatosis type 1: follow-up of 44 patients. , J AAPOS. 2010 Apr;14(2): 155-8.
- 28.Alvord E C, Lofton S. (1988) Gliomas of the optic nerve or chiasm. Outcome by patients' age, tumor site, and treatment". , J Neurosurg 68(1), 85-98.