Abstract
Purpose:
Cataract is the leading cause of blindness worldwide. Even in an uneventful cataract surgery, surgically induced astigmatism remains the major hurdle in attaining good unaided visual acuity post surgery. If pre-existing corneal astigmatism is not corrected at the time of surgery, it will result in more postoperative astigmatism; therefore, it is important to correct pre-existing corneal astigmatism.
Material & Methods
In this prospective study, 100 eyes of 100 age and sex matched patient’s with comparable preoperative astigmatism and visual acuity were divided in two groups according to pre operative corneal astigmatism. SIG (superior scleral incision group) included 50 eyes with steeper vertical axis and TIG (temporal corneal incision group) included 50 eyes with steeper horizontal axis. SIG and TIG were subjected to superior scleral tunnel and temporal corneal tunnel incisions respectively. Corneal astigmatism was measured preoperatively and at 1, 2 and 6 weeks postoperatively.
Results:
The mean postoperative astigmatism in SIG and TIG after 6 weeks was 0.545 ± 0.51D and 0.59 ± 0.48 D in comparison to preoperative astigmatism of 1.105 ± 0.54 D and 1.120 ± 0.49 D respectively. The difference was statistically significant in both the groups with P< 0.001 for both groups. The difference in surgically induced astigmatism between the two groups was not significant at any point of time after surgery (p>0.05).
Conclusion:
Incision site on steeper axis helps in reduction of pre-existing corneal astigmatism in cataract surgery. Both superior scleral and temporal corneal incisions help in neutralization of approx. 0.4-0.7 D of astigmatism.
Author Contributions
Academic Editor: Guo-Zhang Zhu, Department of Biological Sciences, Marshall University Huntington, WV 25705, USA
Checked for plagiarism: Yes
Review by: Single-blind
Copyright © 2015 Kavita Bhatnagar, et al.
 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Competing interests
The authors have declared that no competing interests exist.
Citation:
Introduction
Cataract is the leading cause of blindness worldwide. Even in an uneventful cataract surgery, surgically induced astigmatism remains the major hurdle in attaining good unaided visual acuity post surgery. If pre-existing corneal astigmatism is not corrected at the time of surgery, it will result in more postoperative astigmatism; therefore, it is important to correct pre-existing corneal astigmatism. Surgically induced astigmatism (SIA) depends on the type, length and position of incision and also the method of wound closure. 1
The purpose of this study was to find out if it was possible to achieve correction of preoperative astigmatism by planning incision on steeper axis during cataract surgery and to assess surgically induced astigmatism and any shift in astigmatism from ‘with the rule astigmatism’ (WTR) with steep axis in vertical meridian (axis 0-30 or 150-180 degrees) to ‘against the rule astigmatism’ (ATR) with steep axis in horizontal meridian (axis 60-120 degrees) and vice-versa.
Material & Methods
This hospital based prospective clinical study was conducted in the Department of Ophthalmology of a tertiary care teaching hospital from Nov-2010 to Nov-2012. The sample size was 100 eyes of 100 patient’s with uncomplicated senile cataracts with pre operative astigmatism between 0.25-1.5 D in two principal meridians as evident by keratometry on autorefractometer-keratometer (Potek, PRK-5000 autorefractometer- keratometer) were included in this study. Patients with no pre existing astigmatism, oblique astigmatism (axis between 30 to 60 degrees or between 120 to 150 degrees), irregular astigmatism (two principle meridian are not at 90 degrees to each other) or patients with previous ocular trauma, surgery and pathologies that could have affected corneal refraction were excluded from the study. Patients with intra and post operative complications were excluded too. 100 eyes of 100 patients were selected and were divided in two groups according to pre operative astigmatism on the basis of their keratometric findings. SIG (superior sclera incision group) included 50 eyes with steeper vertical axis that is ‘with the rule astigmatism’ (axis 180±10 degrees) and TIG (temporal corneal incision group) included 50 eyes with steeper horizontal axis that is ‘against the rule astigmatism’ (axis 90±10 degrees). SIG and TIG were subjected to self sealing superior sclera and temporal corneal incisions respectively. All the patients were operated by the same surgeon and detailed pre operative ocular examination, assessment of pre and post operative visual acuity, a A-scan biometry to calculate IOL power using SRK formula and record of pre and post operative keratometry was done by the same observer to eliminate observer’s bias.
The visual acuity was noted preoperatively and at follow up visits at 1, 2 and 6 weeks post-operatively. Preoperative keratometry of all the patients was done with Keratometer. K0V being the vertical and K0H horizontal keratometry reading. SIG had K0V>K0H; with the rule astigmatism (axis 180±10 degrees) and TIG had K0H>K0V; against the rule astigmatism (axis 90±10 degrees). Post operative keratometry was done at 1, 2 and 6 weeks postoperatively.
Institutional ethical committee approval was obtained for the study. Written informed consent was taken on previous day of the surgery and patients were explained regarding complications of surgery and anaesthesia. They were informed about the nature of study and only willing subjects were included in this study.
Peribulbar block with a mixture of 2% Xylocaine with Hyaluronidase and 0.5 % Sensorcaine was used for local anesthesia in all cases. For all cases having ‘With the rule astigmatism’ (SIG)
incision (axis 180±10 degrees) was located superiorly while for all cases having ‘Against the rule astigmatism’ (axis 90±10 degrees) (TIG) incision was located temporally. In SIG group, a three- step scleral tunnel incision was made at 12 o’clock, 1.5 mm away from the limbus and for TIG group, a three step corneal incision was made temporally with a 2.8 mm crescent blade. Phacoemulsification (Zeiss Visalis 100 Phacoemulsification system )was performed by multiple chop technique. The incision was enlarged to 3.2 mm and a foldable intra ocular lens Rayner C was implanted in the capsular bag with the help of an injector in all patients. No sutures were used in any of the cases. Patients were given Prednisolone acetate steroid eye drops for a total duration of 1 month in the following regimen: 4 times a day for 1 week, 3 times a day for next 1 week, 2 times a day for next 1 week, and once a day for 1 week and then stopped. Nepalact eye drops (NSAID drops) were given 3 times a day for 2 weeks and then 2 times a day for 4 weeks and then stopped. Antibiotic drops were given 4 times a day for 1st week and then stopped. Corneal astigmatism was measured by autorefractometer-keratometer preoperatively and 1 week, 2 weeks and 6 weeks postoperatively.
Amount of astigmatism was calculated by simple subtraction method. Data was compiled and statistical analysis was done using SPSS version-16. To study whether there was significant reduction in preoperative astigmatism after phacoemulsification with incision on steeper axis, the ‘t test’ was used. Student’s t test was used to compare means from two independent groups. A p value of < 0.05 was considered significant.
Results
The mean age in superior incision group (SIG) was 60.64 ± 6.51yrs and in temporal incision group (TIG) was 61.60 ± 6.75 yrs. Thus, patients in both groups were comparable preoperatively and the difference in age group was not statistically significant (P=0.47). The patients were also comparable in terms of sex wise distribution and preoperative visual acuity. The mean preoperative astigmatism in superior incision group was found to be 1.105 ± 0.54 D on axis 180±10 degrees whereas it was 1.120 ± 0.49 D on axis 90±10 degrees for the temporal incision group. The difference in the means was not statistically significant P (0.88). (Table 1)
Table 1. Patient Particulars| Superior sclera incision group(50 eyes of 50 patients) | Temporal corneal incision group(50 eyes of 50 patients) | P value | |
| Age ( years)Sex (male: female)Preoperative astigmatism (mean diopter)Preoperative visual acuity<_6/606/36-6/246/18 | 60.64 ± 6.51yrs26:241.105 ± 0.54 31 (62%)18 (36%)1 (2%) | 61.60 ± 6.75 yrs27:231.120 ± 0.4933 (66%)16 932%)1 (2%) | 0.47-0.88 |
In both the groups, one patient had posterior capsular rent with vitreous loss and they were excluded from the study as foldable IOL could not be implanted in the bag. Rigid PMMA IOL was implanted in the sulcus after good anterior vitrectomy. Iris prolapse in one case could be managed successfully. Iris chaffing was seen in 2 cases but it did not affect end result. Fortunately we did not have any nucleus drop, persistent CME and endophthalmitis in this series.
In SIG 4(8%) patients showed shift from preoperative ‘with the rule astigmatism’ on axis 180±10 degrees to ‘against the rule astigmatism’ on axis 90±10 degrees at 6 weeks postoperatively. In TIG also 4(8%) patients showed shift towards ‘with the rule astigmatism’ on axis 180±10 degrees from preoperative ‘against the rule astigmatism’ on axis 90±10 degrees postoperatively after 6 weeks. In SIG, mean postoperative astigmatism after 6 weeks was 0.545 ± 0.51D on axis 180±10 degrees in comparison to preoperative astigmatism of 1.105 ± 0.54 D on axis 180±10 degrees. The difference was statistically significant P (< 0.001). In TIG mean postoperative astigmatism was 0.59 ± 0.48 D on axis 90±10 degrees in comparison to preoperative astigmatism of 1.120 ± 0.49 D on axis 90±10 degrees. The difference was found to be statistically significant P (< 0.001). (Table 2)
Table 2. Comparison of Preoperative Astigmatism and Amount of Astigmatism 6 Weeks Postoperatively| GROUPS | Pre-Op Astigmatism (Diopter) | Post-Op Astigmatism (Diopter) | P-value |
| Superior sclera incision Group 1 | 1.105 ± 0.54 | 0.545 ± 0.51 | < 0.001 |
| Temporal corneal incision Group 2 | 1.120 ± 0.49 | 0.59 ± 0.48 | < 0.001 |
Surgically induced astigmatism, in SIG was 0.48 ± 0.14 D, 0.49 ± 0.17 D and 0.56 ± 0.20 D on axis 180±10 degrees after 1week, 2weeks and 6 weeks respectively while in TIG, it was 0.52 ± 0.17 D, 0.52 ± 0.17 D and 0.54 ± 0.15 D on axis 90±10 degrees after 1week, 2 weeks and 6 weeks respectively. The difference between SIA in both the groups was not statistically significant at 1 week (P 0.74), at 2 weeks (P 0.75) and at 6 weeks (P 0.48). (Table 3)
Table 3. Comparison of Surgically Induced Astigmatism (in dioptres) in the two Groups at 1, 2 and 6 Weeks Post Surgery| Duration post surgery (weeks) | Superior Scleral Incision Group 1Mean Astigmatism (dioptres) | Temporal Corneal Incision Group 2 Mean Astigmatism (dioptres) | P value |
| 1 | 0.48 ± 0.14 | 0.52 ± 0.17 | 0.74 |
| 2 | 0.49 ± 0.17 | 0.52 ± 0.17 | 0.75 |
| 3 | 0.56 ± 0.20 | 0.54 ± 0.15 | 0.48 |
In SIA group, 27 (54%) patients acquired 6/6-6/9, 21 (42%) acquired 6/12 – 6/18 and 2(4%) acquired 6/24 Uncorrected Visual acuity (UCVA) 6 weeks postoperatively.
In TIA group, 26 (52%) patients had UCVA 6/6-6/9, 23 (46%) had UCVA 6/12 – 6/18 and 1(2%) had UCVA 6/24. Best corrected visual acuity (BCVA) was found to be 6/6 in all the patients in both the groups. [Bar diagram 1]
Bar diagram 1.Uncorrected visual acuity (UCVA) and BCVA after 6 weeks Postoperative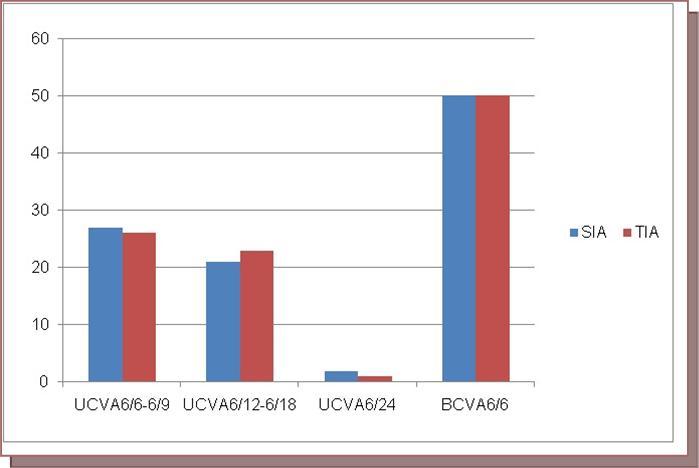
Discussion
Cataract surgery has gone through a ladder of technological advancements, raising the bar for surgical outcomes and patients expectations and level of satisfaction post surgery. Patients now expect good unaided visual acuity and less dependence on spectacles after surgery. To attain this goal, one important consideration is reduction of astigmatism. Modern cataract surgery using small incisions and foldable IOLs has led to achieving emmetropia in a great number of patients.. Modifications of surgical techniques and incisions may further improve refractive outcomes by reduction of astigmatism. Different methods have been used to correct pre-existing astigmatism during cataract surgery. These are choosing incision on steeper axis, astigmatic keratotomy, and corneal relaxing incisions for pre-existing corneal astigmatism less than 1.5 D. 2, 3
Astigmatic keratotomy may give rise to glare sensation, diplopia and fluctuation of refractive error due to proximity of the incisions to the centre cornea. 4 Corneal relaxing incisions are technically easy, producing less symptoms, early wound stabilization but requires diamond knife and preoperative pachymetry in addition to controversies in application of the nomogram. 5, 6 Choosing incision on steep corneal axis is the simplest method for lower degree of astigmatism.
In this prospective study on 100 eyes of 100 age and sex matched patients, we tried to evaluate effectiveness of on steep axis incisions in reducing pre-existing corneal astigmatism keeping all the other parameters same in both the groups except site and type of incision. Even pre-existing astigmatism and visual acuities were comparable in the two groups. We used superior scleral incision for pre-existing with the rule astigmatism and temporal corneal incision for pre-existing against the rule astigmatism.
Studies suggest that for patients with less than 1 D of pre-existing corneal astigmatism, placing the phacoemulsification incision on the steep meridian of corneal astigmatism is the ideal approach. 7 Nielsen PJ 8 found that the refractive effect of the clear corneal incisions did not change significantly from day one to week six. Preoperative against-the-rule astigmatism was reduced significantly by temporally placed clear corneal incisions and preoperative with-the-rule astigmatism, by superiorly placed clear corneal incisions. Our results correspond with these findings. The only difference is that we used superior sclera incision and temporal corneal incision. In this study, the difference in mean preoperative and postoperative astigmatism 6 weeks after surgery was statistically significant in both superior sclera and temporal corneal incision groups (P < 0.001). This proves that there was a significant reduction in pre-existing astigmatism. There are reports that sclera incisions are less effective in reducing astigmatism than corneal incisions while our study did not find any such difference. Both superior sclera and temporal corneal incisions were effective in reducing pre-existing astigmatism and could neutralize approx. 0.4 D to 0.7 D astigmatism so our first objective was achieved.
Our second objective was to compare surgically induced astigmatism between the two groups. The difference between SIA in both the groups was not significant at any point of time postoperatively (p>0.05). These findings corroborate with other similar studies. 9, 10
Our third objective was to assess any shift from preoperative ‘with the rule astigmatism’ (astigmatism on axis 180±10 degrees) to ‘against the rule astigmatism’( astigmatism on axis 90±10 degrees) and vice-versa. In SIG 4(8%) patients showed shift from preoperative ‘with the rule astigmatism’ to ‘against the rule astigmatism’ at 6 weeks postoperatively. In TIG also 4(8%) patients showed shift towards ‘with the rule astigmatism’ from preoperative ‘against the rule astigmatism’ postoperatively after 6 weeks. As any incision on the cornea flattens the same axis and steepens cornea 90 degree away from the site of incision, superior incision leads to shift in astigmatism towards against the rule and temporal incision leads to shift towards with the rule type of astigmatism. These findings corroborate with findings of Tejedor J, Murube J 11 who found that superior incision led to shifting of astigmatism from preoperative with the rule to against the rule postoperatively and shift to with the rule from preoperative against the rule for temporal incision group.
There was marked improvement from preoperative visual acuity which is expected after phacoemusification with IOL implantation. Both groups had comparable UCVA and BCVA postoperatively. Thus, choosing a proper site of incision preoperatively can lead to significant improvement in both UCVA and BCVA after cataract surgery by phacoemulsification with foldable IOL.
Strengths of this study are that patients in both groups were comparable preoperatively with reference to their age, sex, preoperative visual acuity and pre-existing corneal astigmatism in both the groups. A single surgeon operated all the cases. A single ophthalmology resident carried out entire preoperative and postoperative evaluation on all the visits. A major limitation of this study is shorter follow-up period therefore a long term follow up is required to corroborate our findings.
Conclusion:
Selection of the site of incision on steeper axis on the basis of preoperative keratometric status of the patient helps in reduction of astigmatism. Both superior sclera and temporal corneal incisions help in neutralization of approx.0.4-0.7 D of astigmatism. There is a shift towards ATR astigmatism on axis 90±10 degrees in superior approach and towards WTR astigmatism on axis 180±10 degrees in temporal approach. There is marked improvement in visual acuity after phacoemusification with incision on steeper axis, early stabilization of astigmatism and early patient rehabilitation leading to greater patient satisfaction.
References
- 1.Haldipurkar S S, Hasanain T Shikari, Gokhale Vishwanath. (2009) Wound construction in manual small incision cataract surgery.IndianJOphthalmol.2009Jan–Feb; 57(1):. 9-13.
- 2.Tetsuro Oshika.Sugita Gentaro Tanabe Tatsuro, Tomidokoro Atsuo, Amano Shiro. (2000)Regular an keratomileusisd irregular astigmatism after superior versus temporal scleral incision cataract surgery. , Ophthalmology.November2000; 107(11), 2049-2053.
- 3.Kaufmann C, Peter J, Ooi K, Phipps S, Cooper P et al. (2005) Limbal relaxing incisions versus on-axis incisions to reduce corneal astigmatism at the time of cataract surgery. , J Cataract Refract Surg.2005Dec; 31(12), 2261-5.
- 4.Lindstrom R L, Lindquist T D. (1988) Surgical correction of postoperative astigmatism. , Cornea1988; 7, 138-48.
- 5.Muller-Jensen K, Fisher P, Siepe U. (1999) Limbal relaxing incisions to correct astigmatism in clear corneal cataract surgery. J Refract Surg. 15, 586-89.
- 7.Lesiewska-Junk H, Kaluzny J, Malukiewicz-Wisniewska G. (2002) Astigmatism after cataract surgery. Klin Oczna2002;104(5-6):. 341-43.
- 8.Joshi1 M R, Shakya S. (2009) Change in refractive status of the patients undergoing phacoemulsification surgery. , Nepal Med Coll 11(1), 19-22.
- 9.Nielsen P J. (1995) Prospective evaluation of surgically induced astigmatism and astigmatic keratotomy effects of various self-sealing small incisions. , J Cataract Refract Surg.1995Jan; 21(1), 43-8.
