Abstract
Central retinal artery occlusion (CRAO) is a retinal ischemic disorder associated with sudden loss of vision and has a poor prognosis. We report a case of CRAO that occurred during frontal sinus surgery involving craniotomy in a patient with a frontal sinus cyst. The prognosis for treatment after the acute phase is generally unfavorable; however, aggressive treatment is recommended for patients with visual acuity of “hand motion” or better within 1 day after onset. This case highlights the need for informed consent prior to nasal or paranasal sinus surgery, including mention of the possibility of CRAO as a complication.
Author Contributions
Academic Editor: Ioannis Chatzistefanou, Aristotele University of Thessaloniki (A.U.Th)
Checked for plagiarism: Yes
Review by: Single-blind
Copyright © 2016 Yasushi Ota, et al
 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Competing interests
The authors have declared that no competing interests exist.
Citation:
Introduction
Central retinal artery occlusion (CRAO) is a retinal ischemic disorder associated with sudden loss of vision and has a poor prognosis. Loss of vision is caused by vessel occlusion leading to ischemic injury affecting nerve cells (ganglion, amacrine, and bipolar cells) that line the retina. CRAO is often associated with vascular thrombotic events. It usually occurs in elderly patients with hypertension or diabetes, but may also develop due to retrobulbar anesthesia, as a complication of optic neuritis, or during surgery.1, 2, 3 Here, we report a case of CRAO that occurred during frontal sinus surgery with craniotomy in a patient with a frontal sinus cyst.
Case History
A 57-year-old man had presented 12 years earlier with left upper eyelid swelling, was diagnosed with frontal sinusitis, and underwent surgery at another hospital. Craniotomy was performed with removal of the left frontal bone and placement of a ceramic implant. The subsequent clinical course was uneventful. However, on February 3, 2007, he again experienced left upper eyelid swelling and pain that was evaluated at a local clinic. Antibiotics were prescribed.
Recurrent frontal sinusitis was suspected, and the patient was referred to our department for evaluation on February 14, 2007. On initial evaluation, the left upper eyelid swelling was resolved; however, paranasal sinus computed tomography (CT) showed two left frontal sinus cysts (Figure 1). The patient had a history of hypertension that was well-controlled on oral medications. No other major disorders were present, including diabetes or heart disease.
Figure 1.CT of the paranasal sinuses showed two left frontal sinus cysts. Black arrows: ceramic implant. Black stars: two left frontal sinus cysts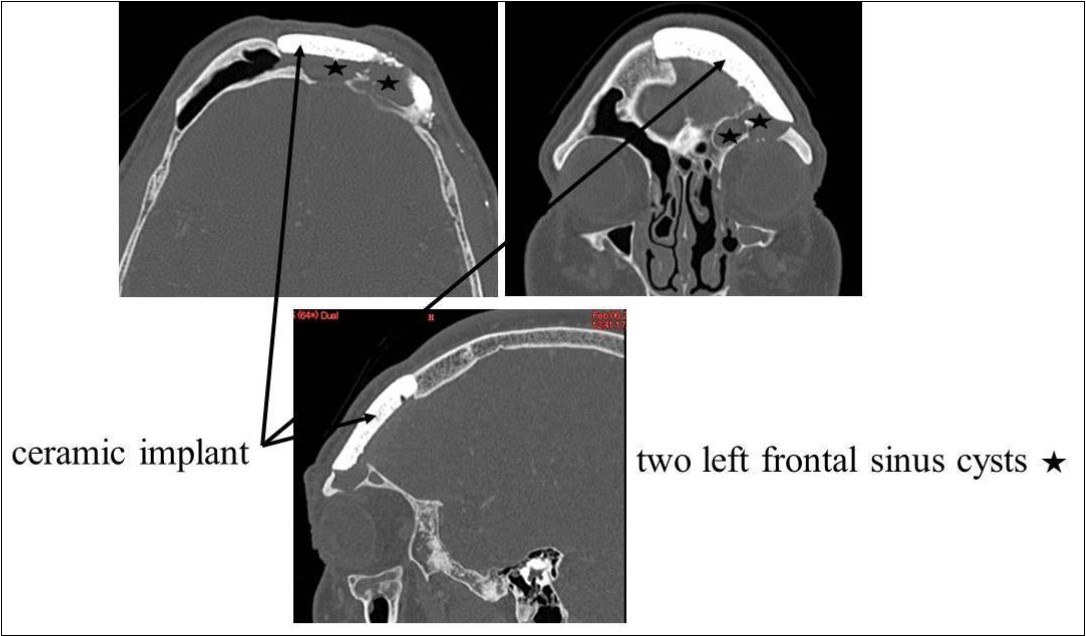
On April 28, 2007, craniotomy was performed under general anesthesia, with removal of the ceramic implant and median drainage of the frontal sinus (Figure 2). Two cysts in the left lateral frontal sinus were opened. One cyst was inflamed with thickened mucosa. The left and right frontal sinuses were opened widely, the anterosuperior nasal septum was excised, and a large drain was placed (Figure 3). A new ceramic implant was not placed because of infection and contamination. The operative time was 4 h 25 min (surgery completed at 18:30). Blood loss was 400 mL, without the need for any transfusions. During endotracheal intubation and extubation, no significant changes in blood pressure were observed, nor were any arrhythmias identified. During surgery, epinephrine gauze (1:5000) was used several times, and a total of 15 mL of epinephrine (1:20,0000) was injected intranasally. Specifically, no intraoperative manipulation or compression of the left eye was performed. Just before completion of surgery, gauze with Achromycin ointment was packed into the nasal cavity, the absence of bleeding was confirmed, and surgery was completed.
Figure 2.Craniotomy and median drainage. Left: Removal of the ceramic implant from the frontal bone. Right: Median drainage of the frontal sinus.
Figure 3.Frontal sinus median drainage by nasal endoscopy. Drill head from the cranial side. The left and right frontal sinuses were opened.
After arousal from surgery (at about 19:30), the patient complained of difficulty seeing with his left eye, particularly in the central field of vision. At 21:00, a paranasal sinus CT showed no evidence of orbital injury during surgery. An emergency ophthalmology consult was requested, and CRAO was diagnosed. Urokinase and Palux infusion were started, and the eye was massaged.
The following day (April 19, 2007), the corrected visual acuity of the left eye was 1.2; funduscopy showed a cherry red spot, characteristic of CRAO (Figure 4). Vision in the left eye subsequently improved gradually. At hospital discharge, although not perfect, vision had improved to the point where no impairment to daily activities was present.
Figure 4.Cherry red spot. Funduscopy showed a cherry red spot.
On April 16, 2008, reoperation was performed to place a ceramic implant, but some pus was found in the left lateral sinus. The lesion was debrided, the dead space was filled with muscle, and surgery was completed without ceramic implantation. On October 17, 2008, another surgery confirmed that the frontal sinus was clean, and a ceramic implant was placed. The postoperative course has been good, and as of May 2009, the frontal sinus extending laterally is filled with air (Figure 5, Figure 6).
Figure 5.Paranasal sinus CT after the last surgery. White star: The frontal sinus extending laterally is filled with air.
Figure 6.Endoscopic findings after surgery. Right and left frontal sinuses. The entrance of the left frontal cyst area is clearly opened (black arrow). The left frontal sinus extending laterally is filled with air.
Discussion
Intraorbital and intracranial complications are the most serious complications of nasal and paranasal sinus surgery. A major adverse complication in paranasal sinus surgery is loss of vision.4 In our patient, CRAO developed despite a lack of direct orbital manipulation. This intraoperative event certainly represents a serious complication of paranasal sinus surgery.
Increased surgery in elderly patients has been accompanied by an increased incidence of perioperative vascular thrombotic events such as stroke. Such events have also been reported in ear nose and throat surgery. After nasal surgery under local anesthesia, CRAO related to local anesthesia has also been reported5, 6, 7.
CRAO typically presents as sudden unilateral loss of vision and is more common in men in their 50s and 60s. With stenosis or occlusion in the internal carotid arteries due to atherosclerosis, emboli may break off from a plaque and cause a retinal artery embolus. CRAO may also occur during surgery under general anesthesia or during cardiac catheterization. Underlying risk factors include hypertension, arteriosclerosis, heart disease, blood dyscrasia, and diabetes.
During the acute phase, within a few hours after onset, the retina appears normal, with characteristic findings developing within 24 h. The posterior pole of the retina is edematous and opaque, the retina thins at the fovea, and red coloration of the choroid is visible as a “cherry red spot” on funduscopy (Figure 4)8.
If CRAO is diagnosed within 2 h after onset, ocular massage, rapid reduction in intraocular pressure by anterior chamber paracentesis, intravenous acetazolamide, and amyl nitrite inhalation for vasodilation are recommended. In addition, treatment for arterial thrombosis may be started with warfarin, heparin, or urokinase. If treatment is administered after the acute phase, the prognosis is generally unfavorable, but aggressive treatment is recommended for patients with visual acuity of “hand motion” or better within 1 day after onset.8
The development of CRAO was probably incidental in this case. However, since the event occurred during surgery, a causal relationship to surgery cannot be completely excluded. This case highlights the need for informed consent prior to nasal or paranasal sinus surgery, including mention of the possibility of CRAO as a complication; careful ocular evaluation upon arousal from anesthesia; and prompt treatment if any symptoms are encountered.
Conclusion
We have reported the case of a patient with frontal sinus cysts who developed CRAO during surgery under general anesthesia. Treatment was started promptly after diagnosis. The patient’s vision gradually improved, and although not perfect at hospital discharge, recovered sufficiently to perform daily activities. Upon arousal from anesthesia, careful ocular evaluation is mandatory, with prompt treatment if any symptoms are identified.
References
- 1.Ueda Y, Kanazawa S, Ohira A. (2002) Retinal vascular obstruction and asymptomatic cerebral infarction. , Jpn J Ophtalmol 46, 209-214.
- 2.Shah H G, Brown G C, Goldberg R E. (1985) Digital subtraction carotid angiography and retinal arterial obstruction. Ophthalmology. 92, 68-72.
- 3.Douglas D J, Schuler J J, Buchbinder D. (1988) The association of central retinal artery occlusion and extracranial carotid artery disease. , Ann Surg; 208, 85-90.
- 4.May M, Levine H L, Mester S J. (1994) Complications of endoscopic sinus surgery. Analysis of 2108 patients. Incidence and prevention. , Laryngoscope; 104, 1080-1083.
- 5.Savino P J, Burde R M, Mills R P. (1990) Visual loss following intranasal anesthetic injection. , J Clin Neuroophthalmol 10, 140-144.
- 6.Maaranen T H, Mantyjarvi M I. (2000) Central retinal artery occlusion after a local anesthetic with adrenaline on nasal mucosa. , J Neuroophthalmol 20, 234-235.
