Abstract
Background and Context:
Autologous bone grafts require a second surgical exposure to harvest the graft with a significant risk of post-operative complications and donor site morbidity. Employment of allografts potentially eliminates donor site morbidity but carries the potential of causing foreign body immune reactions with a high rate of rejection and failures. Hence, Alloplasts have emerged as novel materials to overcome the drawbacks of autogenous and allogenous bone grafts. Today’s advanced dentistry is enterprising a putty form of calcium phosphosilicate (CPS) into several aspects of reconstructive domain of dentistry including the sinus augmentation procedures, osseous regeneration of periodontal bone defects, cystic cavity defects and alveolar socket preservation. This eccentric multifaceted study was planned as an honest effort on the path of proving the efficiency of CPS as an alloplastic bioactive graft material and aimed at quantitative evaluation of regenerated bone radiographically using Cone Beam Computed Tomography (CBCT) scans following sinus augmentation procedures.
Materials and Methods:
A total of 20 sinus augmentations were carried-out in 17 patients satisfying the criteria (inclusion and exclusion) requiring placement of implants in atrophic maxilla and in other situations of anatomic constraints. The graft material used was calcium phosphosilicate (CPS) putty (Nova bone dental putty, Novabone products, Alachua, Fla). The residual bone height was recorded using CBCT scans and a computer based software where the measurements were made from the crest of the ridge till the sinus floor lining. The patients were assessed clinically at immediate post-operative, 1 week, 1 month, 3 months and 6 months follow-up recalls post-operatively. Radiographic assessment for bone height was done pre-operatively and at 6 months follow-up recall post-operatively using Cone Beam Computer Tomography scans.
Results:
The post-treatment bone height (11.76+0.97mm) was found to be significantly higher than the pre-treatment bone height (6.8 +0.70mm) in indirect sinus augmentation procedures (t=14.4, p<0.005). In case of direct sinus augmentation group also, the post-treatment bone height (11.27 +0.71mm) came-out to be significantly higher than the pre-treatment bone height (2.44 +0.81mm) (t=32.17, p<0.005). The post-treatment bone grafted sinus floor measurements (1107.6 + 155.6mm) were also found to be significantly higher than the original sinus floor measurements of bone density (Grayscale values) (412+ 65.5mm) (t=16.6, p<0.001) in case of indirect sinus augmentation procedures. Similarly, the post-treatment bone grafted sinus floor measurements (1169.6+136.7mm) were found to be significantly higher than the original sinus floor measurements of bone density (Grayscale values) (416.4+ 0.70mm) (t=17.9, p<0.001) in case of direct sinus augmentation group.
Conclusion:
Calcium Phosphosilicate (CPS) was accepted well at the recipient sites without any complications demonstrating its efficiency and reliability in sinus augmentation procedures.
Author Contributions
Academic Editor: Vinayak Raghunathan, Assistant Professor
Checked for plagiarism: Yes
Review by: Single-blind
Copyright © 2016 S.Girish Rao, et al.
 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Competing interests
The authors have declared that no competing interests exist.
Citation:
Introduction:
With advancing age, loss of teeth is a predictable phenomenon. The goal of modern dentistry is to restore normal stomatognathic system. This perception of modern dentistry has been improvised with the evolution of implants. However, in posterior maxilla, rehabilitation with implants has become a challenging procedure due to anatomic and physiologic limitations including bone atrophy, compromised bone quality and pneumatised maxillary sinus.1, 2, 3, 4 With the advent of sinus augmentation procedures, these limitations have been overcome making implant therapy a more feasible treatment option especially in edentulous posterior maxilla. Sinus augmentation procedures can be done via Lateral window approach or Crestal approach techniques. A wide array of bone-grafting materials have been studied for use in maxillary sinus augmentation procedures to accelerate the bone healing process and prevent re-pneumatisation of the maxillary sinus after grafting.5 Autogenous bone, demineralized freeze-dried bone, xenogeneic bone, and alloplastic materials are the various plethora of options available to the surgeon in the present era. Autologous bone grafts require a second surgical exposure to harvest the graft with a significant risk of post-operative complications and donor site morbidity.6 Employment of allografts potentially eliminates donor site morbidity but carries the potential of causing foreign body immune reactions with a high rate of rejection and failures. Hence, Alloplasts have emerged as novel materials to overcome the drawbacks of autogenous and allogenous bone grafts. Today’s advanced dentistry is enterprising a putty form of calcium phosphosilicate (CPS) into several aspects of reconstructive domain of dentistry including the sinus augmentation procedures, osseous regeneration of periodontal bone defects, cystic cavity defects and alveolar socket preservation. In the present study, we used a pre-mixed composite of bioactive CPS particulate with absorbable binder which is an osteo-conductive graft material. It is available in a device which requires no mixing or preparation prior to application. The non-hardening putty is supplied ready-to-use to be applied directly to the intended graft site. There have been numerous phenomenal studies incorporating this material in bone regeneration procedures with respect to periodontal defects, socket preservation following extractions and for providing good bone prior implant placement (preventing additional secondary grafting procedures) and showing optimal osseo-integration after grafting for immediate implant placement. However, search of literature fell short for the firm evidence on usage and success of this material for sinus augmentation procedures, in particular. Hence, this eccentric multifaceted study was planned as an honest effort on the path of proving the efficiency of CPS as an alloplastic bioactive graft material and aimed at quantitative evaluation of regenerated bone radiographically using Cone Beam Computed Tomography (CBCT) scans following sinus augmentation procedures.
Materials and Methods:
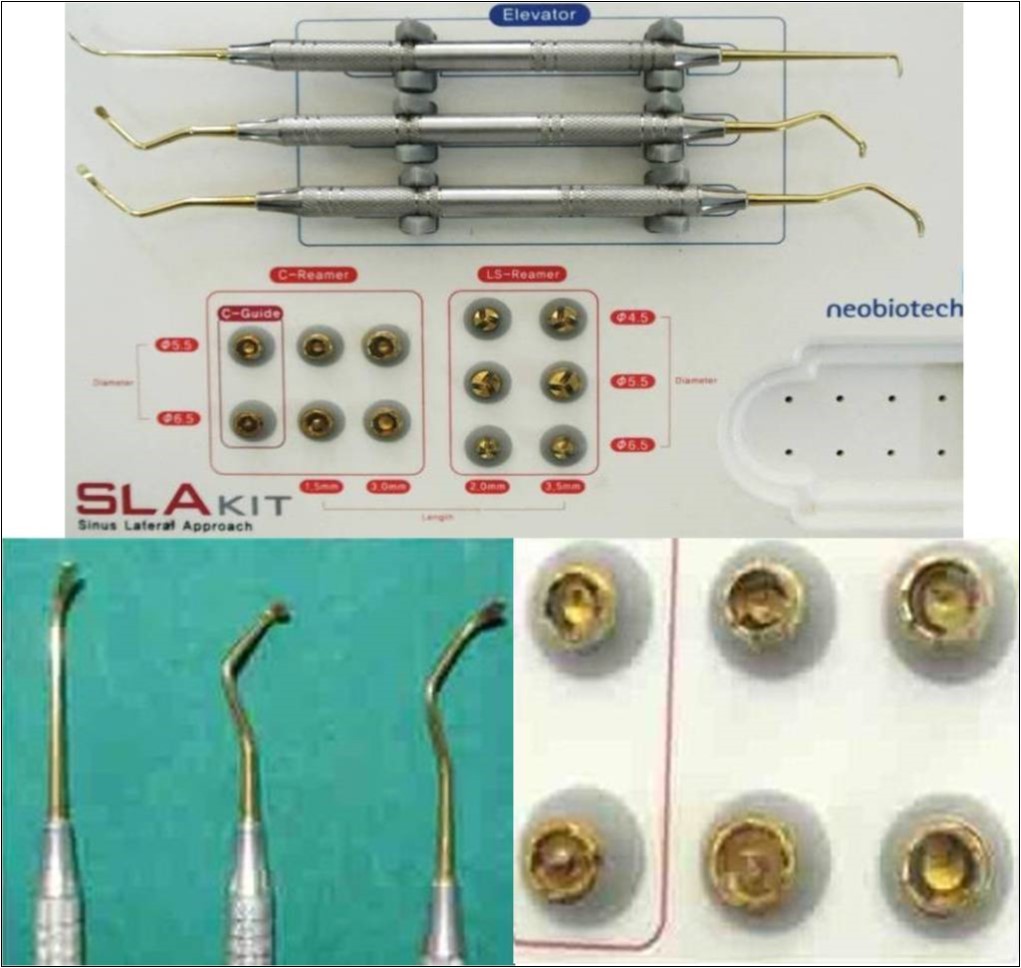
A total of 20 sinus augmentations were carried-out in 17 patients satisfying the criteria (inclusion and exclusion) requiring placement of implants in atrophic maxilla and in other situations of anatomic constraints. The patients were informed about the study including the use of the synthetic graft material and their approval was sought before their inclusion into the study. A written consent was obtained from each of the participating patient. After a detailed history and a thorough clinical examination, including systemic and regional/local examination, patients were taken-up for the sinus augmentation. The type of sinus augmentation procedure, direct or indirect, was decided based on the pre-operative residual bone height evaluated radiographically. The residual bone height was recorded using CBCT scans and a computer based software where the measurements were made from the crest of the ridge till the sinus floor lining. Apically tapered, commercially pure titanium implants (Life Care Devices Private Limited, Mahim, West Mumbai, India) (Figure 1a,b) were used with sinus osteotomes (Figure 2) and associated reamers (Figure 3). The length of implants used were 8, 10 and 11.5mm while the diameter used were 3.5, 4.0 and 5mm. The graft material used was calcium phosphosilicate (CPS) putty (Nova bone dental putty, Novabone products, Alachua, Fla) (Figure 4) in quantities ranging from 0.5cc to 2cc. It is a pre-mixed moldable material consisting of four components including two bioactive phase components, a 55% standard CPS particulate and a 14% CPS smaller particulate in addition to 12% polyethylene glycol additive phase and 19% glycerine binder phase. Bioactivity is initiated immediately upon implantation. The smaller CPS particles release calcium and phosphorous ions into the area while the binder material gets absorbed over a period of a week exposing the larger CPS particulates to blood. In calcium phosphosilicate, the particle sizes are in micrometer size range of 90-710 micrometer range, irregular, in both size and shape. According to Moore et al, in 2001, bioactive glass granules are more quickly reabsorbed than hydroxyapatite, thus, allowing a much more precocious new bone formation in the repair of bone defects.7 On them, osteoblasts show several cytoplasmic processes, pseudopodia, compact appearance, and disorderly dorsal surface, which is characterized by a high cell membrane activity. Therefore, as to the adhesion and close contact between osteoblasts, bioactivity is considered crucial to the development of new bases for bone tissue bioengineering. Its use in various fields, due to its excellent biocompatibility and its physical and chemical properties, has encouraged studies on the feasibility of implant coating, so as to obtain better biologic fixation, and also as a carrier of osteo-inductive substances such as bone morphogenic proteins and other growth factors.8, 9 Other authors also demonstrated the effectiveness of bioactive glass as they improved the osseo-integration of coated implants providing better bone support and presenting with an increased stability when compared to the machined implants.10
Figure 1.(a,b) Apically tapered, commercially pure titanium implants (Life Care Devices Private Limited, Mahim, West Mumbai, India).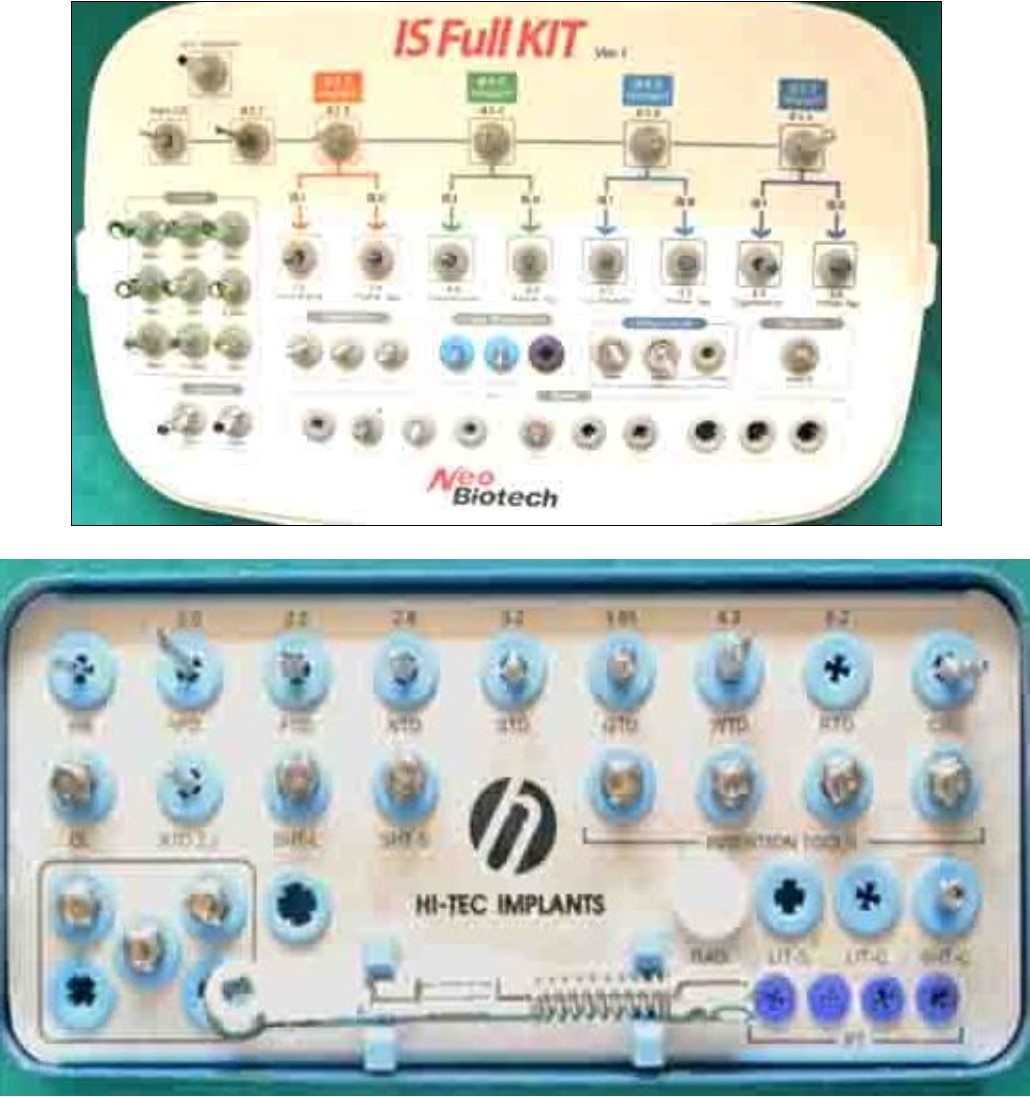
Figure 4.calcium phosphosilicate (CPS) putty (Nova bone dental putty, Novabone products, Alachua, Fla) used as graft material;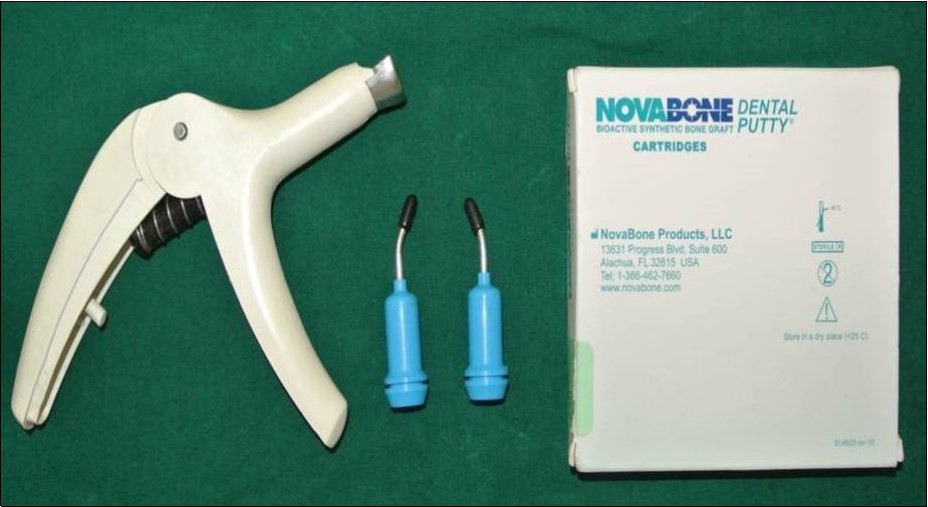
Surgical Technique:
Under complete aseptic conditions, local anaesthesia with vasoconstrictor (2% lignocaine with 1:80,000 adrenaline) was used to obtain ample anaesthesia at the surgical site. Direct sinus membrane elevation was carried-out in cases with residual bone height of <5mm where a lateral spherical bone window was created using the lateral sinus approach technique. No membrane covering was used to cover the defect. (Figure 5a-f) Indirect sinus membrane elevation followed by implant placement was done in cases with residual bone height of >5mm but <9mm. (Figure 6a-h) Alloplastic graft material was then dispensed using the gun and cartridge form either through the bone window or through the crestal osteotomy site before achieving the primary closure. The patients were assessed clinically at immediate post-operative, 1 week, 1 month, 3 months and 6 months follow-up recalls post-operatively. Radiographic assessment for bone height was done pre-operatively and at 6 months follow-up recall post-operatively using Cone Beam Computer Tomography scans. In this comparative study, the measurements were tabulated and statistically analysed to evaluate the difference in increase in bone height between direct and indirect sinus augmentation procedures radiographically.
Figure 5.(a-f) Direct sinus membrane elevation carried-out under complete aseptic conditions and local anaesthesia with vasoconstrictor (2% lignocaine with 1:80,000 adrenaline) in cases with residual bone height of <5mm where a lateral spherical bone window was created using the lateral sinus approach technique; no membrane covering was used to cover the defect;
Figure 6.(a-h) Indirect sinus membrane elevation followed by implant placement done in cases with residual bone height of >5mm but <9mm;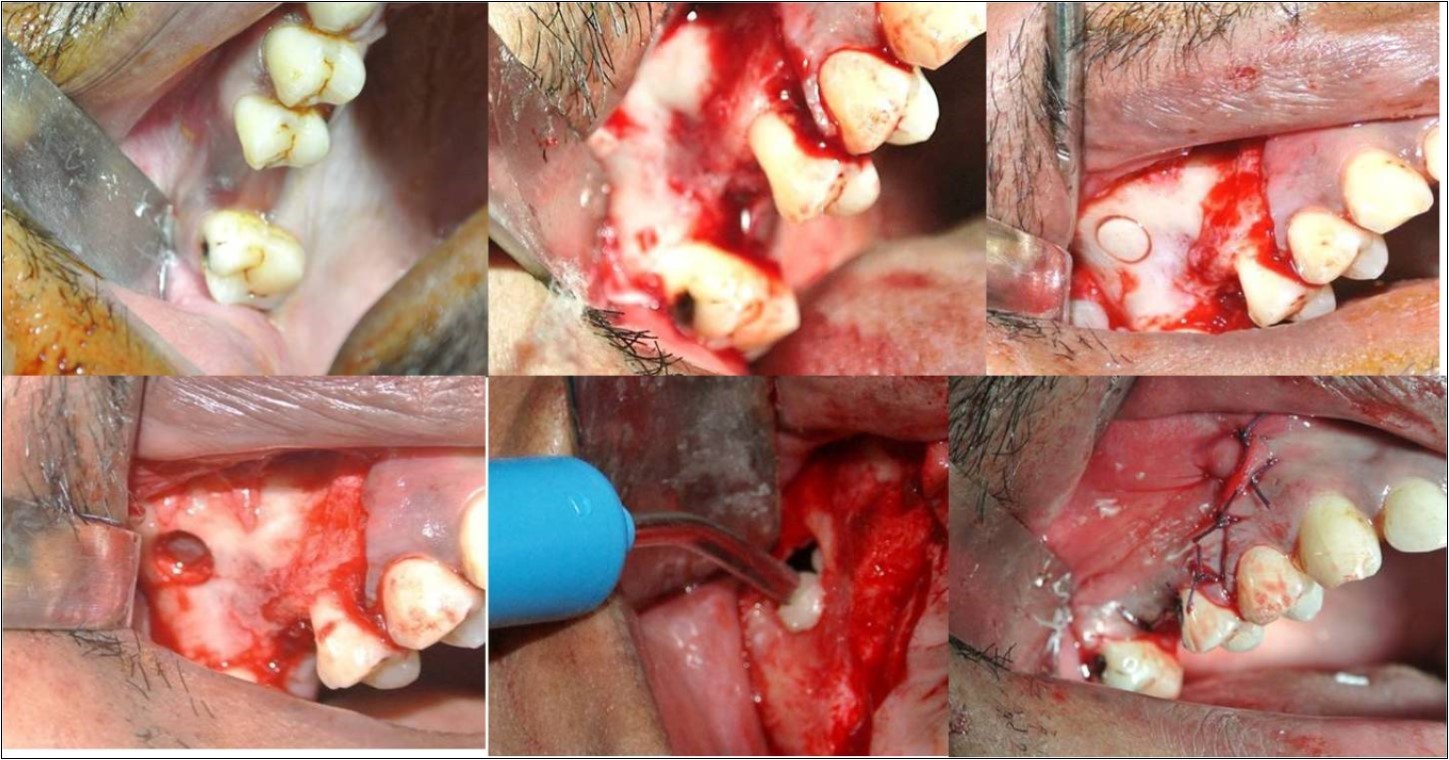
Radiographic Analysis:
Orthopantomographs (OPGs) were taken to rule-out other pathologies and as a part of initial assessment. CBCT scans were assessed for pre-operative and post-operative bone height, bone width and bone density. The CBCT scans were obtained from Kodak 9300 which is a hybrid machine using a CS3D imaging software and flat panel detector sensor with exposure parameters of 90KVp and 10mA and with a resolution of 90 microns. The cross-sections were made 1mm apart. The images acquired were in the Digital Imaging and Communications in Medicine (DICOM) (National Electrical Manufacturers Association, Rosslyn, VA. and American College of Radiology, Reston, VA) data format. DICOM is a standard software for handling, storing, printing and transmitting information in medical imaging. During a single rotation of the source and receptor, the receptor captures the entire volume of anatomy within the FOV. The DICOM data is imported into the viewing software allowing visualization of the axial, coronal and sagital reconstructed images as well as 3D volumes. These third party softwares can serve as an adjunct in treatment planning with common examples of such softwares including SimPlant (Materialise Dental NV, Leuven, Belgium) and Procera Software 2.0 (Nobel Biocare USA, Yorba Linda, California). These convert DICOM data into files that provide information for pre-surgical planning. Few studies which have been carried-out in the past evaluating bone height pre-operatively using CBCT considered the pre-operative bone height as a measurement taken from the crest of the ridge till the sinus floor and post-operatively, the bone height was measured from the crest till the hyper density was evident apically. These measurements obtained were standardized as a computer software drawing tool was used. Bone width measurements were taken as a mean of the bucco-palatal width at three intervals including at the crest, 3mm from the crest and 6mm away from the crest. Bone density was assessed visually by the width of trabecular pattern and was classified based on Misch‘s classification. Another additional bone density tool used was the pixel values (the gray scale values) obtained on the CBCT scan (not truly reliable) and comparison was done pre-operatively and post-operatively. The pixel values contained were a mean of three measurements obtained along the residual bone corresponding with the bone width levels.
Cases done with pre-operative CBCT evaluations (only 4 representative cases are being discussed to avoid repetition):
Case Report 1:
A 40 years old male patient reported to the Department of Oral and Maxillofacial Surgery, D.A.P.M.R.V Dental College and Hospital with a chief complaint of inability to chew food because of loose teeth from past one year. The teeth were extracted an year ago in the right upper and lower back tooth regions because of gross loss of tooth structure and poor prognosis for root canal treatment. Patient was a controlled diabetic and was on medication for the same. Patient did not give history of any existing sinus pathologies. All possible rehabilitative options were explained to the patient and a treatment plan of replacement of missing teeth with implant supported prosthesis using two dental implants was finalized.
Clinical and Radiological Assessment:
1.Partially edentulous maxillary and mandibular arches with missing 16, 17, 18, 46, 47, 48;
2.Increased pneumatisation of right maxillary sinus;
3.Chronic generalized periodontitis;
4.Inter-ridge space adequate to place implant (25mm).
Treatment: Direct sinus augmentation using calcium phosphosilicate (CPS) in relation to 16,17 followed by implant placement as a single step procedure was advised. Lateral window was created and calcium phosphosilicate putty (2cc) was dispensed as the graft material through the lateral osteotomy site to maintain the elevated sinus membrane followed by placement of two dental implants through the crestal approach measuring 3.75 x 11.5mm under local anaesthesia and strict aseptic protocols. At the end of 6 months, a repeat CBCT scan was advised to evaluate the increase in bone height. (Figure 7a-c, pre-treatment; Figure 8a-c, post-treatment)
Figure 7.(a-c) Pre-treatment OPG and cross sections of CBCT showing residual alveolar bone height for Case No.1;
Figure 8.(a-c) Post-treatment OPG and cross sections of CBCT showing residual alveolar bone height for Case No.1;
Case Report 2:
A 42 years old male patient reported to the Department of Oral and Maxillofacial Surgery, D.A.P.M.R.V Dental College and Hospital with a chief complaint of inability to chew food because of missing teeth in upper right and left back tooth regions from past one year. The teeth were extracted an year ago because of gross loss of tooth structure and poor prognosis for root canal treatment. Patient was a hypertensive since 4 years and was on medication for the same. Patient did not give history of any existing sinus pathologies. All possible rehabilitative options were explained to the patient and a treatment plan of replacement of missing teeth with implant supported prosthesis using one dental implant in 17 region was finalized.
Clinical and Radiological Assessment:
1.Partially edentulous maxillary and mandibular arches with missing 17, 26, 45, 46;
2.Increased pneumatisation of right maxillary sinus;
3.Height of available bone- 6.6mm;
4.Transverse thickness of available bone (CBCT evaluation)- 11mm;
5.Inter-ridge space adequate to place implant (10mm).
Treatment:
Patient underwent the procedure of indirect sinus elevation using sinus osteotomes in relation to 17 region. Calcium phosphosilicate putty was dispensed as the graft material through the crestal osteotomy site to maintain the elevated sinus membrane followed by placement of a dental implant measuring 5 x 10mm under local anaesthesia and strict aseptic protocols .The implant was allowed to osseo-integrate for a period of six months during which the patient was followed-up periodically and was assessed for peri-implantitis, crestal bone loss and mobility. At the end of 6 months, a repeat CBCT scan was advised to evaluate the increase in bone height. (Figure 9a,b, pre-treatment; Figure 10a,b, post-treatment)
Figure 9.(a,b) Pre-treatment OPG and cross section of CBCT showing residual alveolar bone height for Case No.2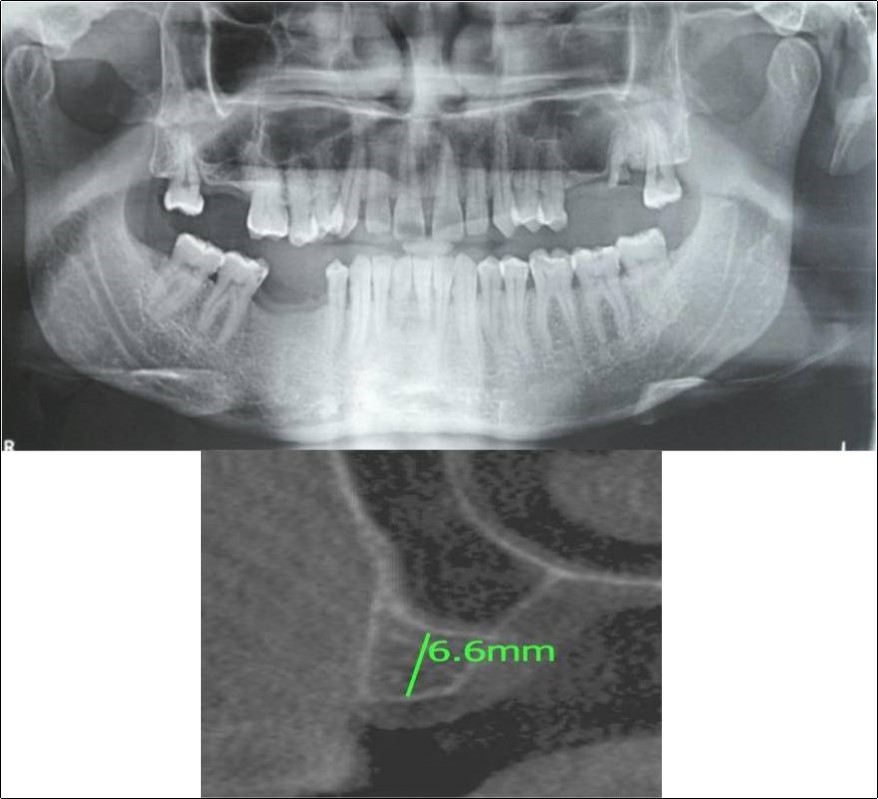
Figure 10.(a,b) Post-treatment OPG and cross section of CBCT showing residual alveolar bone height for Case No.2
Case Report 3:
A 75 years old male patient reported to the Department of Oral and Maxillofacial Surgery, D.A.P.M.R.V Dental College and Hospital seeking options for replacement of his missing tooth in right upper back tooth region with a fixed prosthesis. The tooth was extracted around 10 years ago because of pain and infection associated with the tooth. No prosthetic rehabilitation was carried-out in the past. 16 was found to be missing and the patient reported that healing was uneventful post-extraction of the tooth. The patient was a controlled diabetic and hypertensive and was on medications for the same. Patient did not give history of any existing sinus pathologies. All possible rehabilitative options were explained to the patient and a treatment plan of replacement of missing 16 with implant supported prosthesis using one dental implant was finalized
Clinical and Radiological Assessment:
1.Partially edentulous maxillary arch with missing 16;
2.Increased pneumatisation of right maxillary sinus;
3.Height of available bone- 5.3mm;
4.Transverse thickness of available bone (CBCT evaluation)- 10.2mm;
5.Inter-ridge space adequate to place implant (10mm).
Treatment:
Patient underwent the procedure of indirect sinus elevation using sinus osteotomes in relation to 16 region. Calcium phosphosilicate putty was dispensed as the graft material through the crestal osteotomy site to maintain the elevated sinus membrane followed by placement of a dental implant measuring 5 x 10mm under local anaesthesia and strict aseptic protocols. The implant was allowed to osseo-integrate for a period of six months during which the patient was followed-up periodically and was assessed for peri-implantitis, crestal bone loss and mobility. At the end of 6 months, a repeat CBCT scan was advised to evaluate the increase in bone height. (Figure 11a,b, pre-treatment; Figure 12a,b, post-treatment)
Figure 11.(a,b) Pre-treatment OPG and cross section of CBCT showing residual alveolar bone height for Case No.3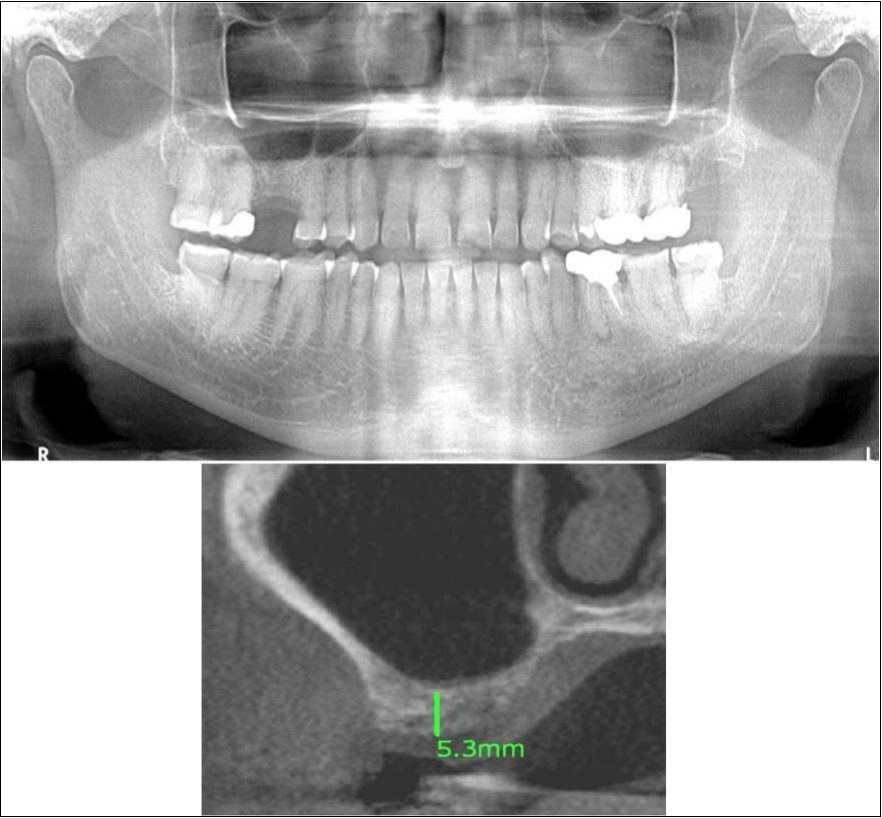
Figure 12.(a,b) Post-treatment OPG and cross section of CBCT showing residual alveolar bone height for Case No.3;
Case Report 4:
A 19 years old young female patient reported to the Department of Oral and Maxillofacial Surgery, D.A.P.M.R.V Dental College and Hospital seeking options for replacement of her missing right and left upper first molars with a fixed prosthesis as she was uncomfortable with the removable partial denture i.r.t 16 and 26. The teeth were extracted 6 months ago because of gross loss of crown structure and poor prognosis for root canal treatment. Patient was also undergoing fixed orthodontic treatment for proclined upper anteriors. Patient did not give history of any existing sinus pathologies. All possible rehabilitative options were explained to the patient and a treatment plan of replacement of missing teeth with implant supported prosthesis using two dental implants was finalized.
Clinical and Radiological Assessment:
1.Partially edentulous maxillary arch with missing 16 and 26;
2.Increased pneumatisation of right and left maxillary sinus;
3.Height of available bone-
16 region: 6.5mm;
26 region: 6.2mm;
4.Transverse thickness of available bone (CBCT evaluation)-
16 region: 8.3mm;
26 region: 10.5mm;
5.Fixed orthodontic appliance;
6.Inter-ridge space adequate to place implant (11mm).
Treatment:
Patient underwent the procedure of indirect sinus elevation using sinus osteotomes in relation to 26 region. Calcium phosphosilicate putty was dispensed as the graft material through the crestal osteotomy site to maintain the elevated sinus membrane followed by placement of 5 x 10mm dental implant under local anaesthesia and strict aseptic protocols. The implant was allowed to osseo-integrate for a period of six months during which the patient was followed-up periodically and was assessed for peri-implantitis, crestal bone loss and mobility. Patient was taken-up for direct sinus elevation via lateral window approach for sinus augmentation i.r.t 16 region. Under aseptic conditions and local anaesthesia, lateral wall of maxilla was exposed after muco-periosteal flap elevation. A window was created of 1cm diameter corresponding to apical aspect of 16. Sinus membrane was identified and elevated using sinus elevators and reamers without perforating the lining. Once the sinus membrane was elevated, phosphosilicate putty was dispensed through the lateral osteotomy site as the graft material to achieve an augmentation of 1cm assessed clinically and confirmed using post-operative OPG. At the end of 6 months, a repeat CBCT scan was advised to evaluate the increase in bone height. (Figure 13a,b, pre-treatment; Figure 14a,b, post-treatment)
Figure 13.(a,b) Pre-treatment OPG and cross section of CBCT showing residual alveolar bone height for Case No.4;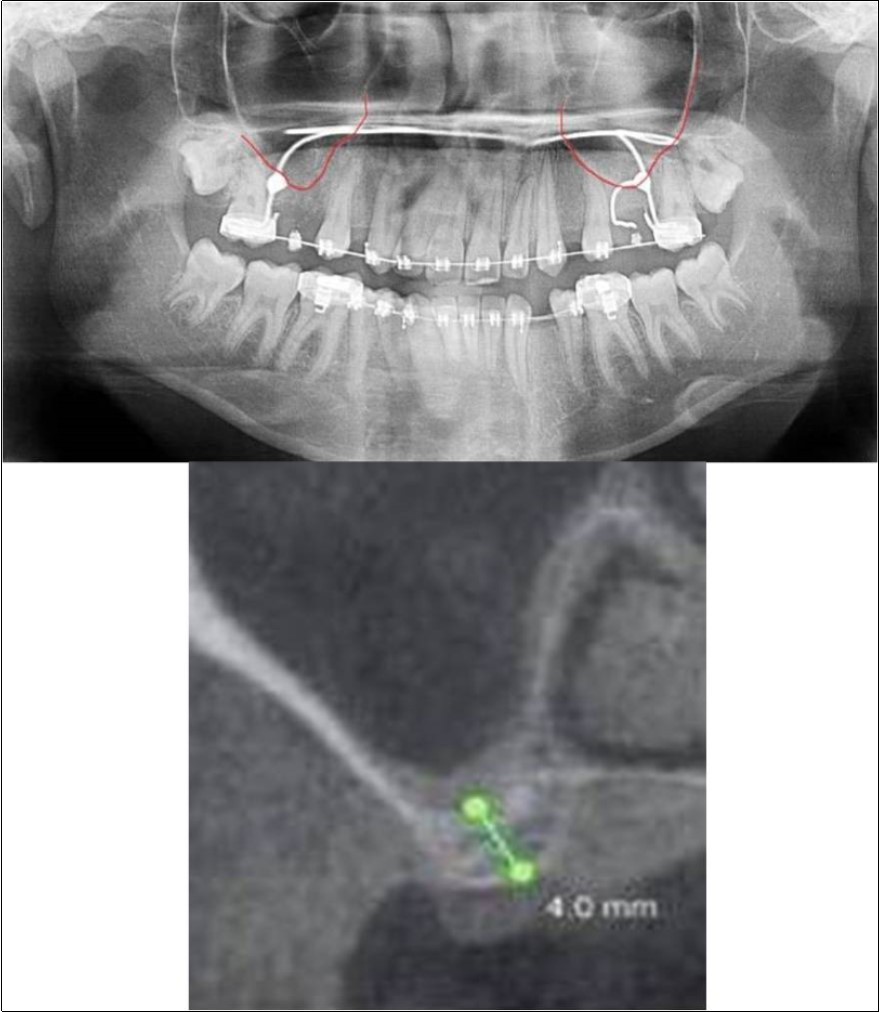
Figure 14.(a,b) Post-treatment OPG and cross section of CBCT showing residual alveolar bone height for Case No.4;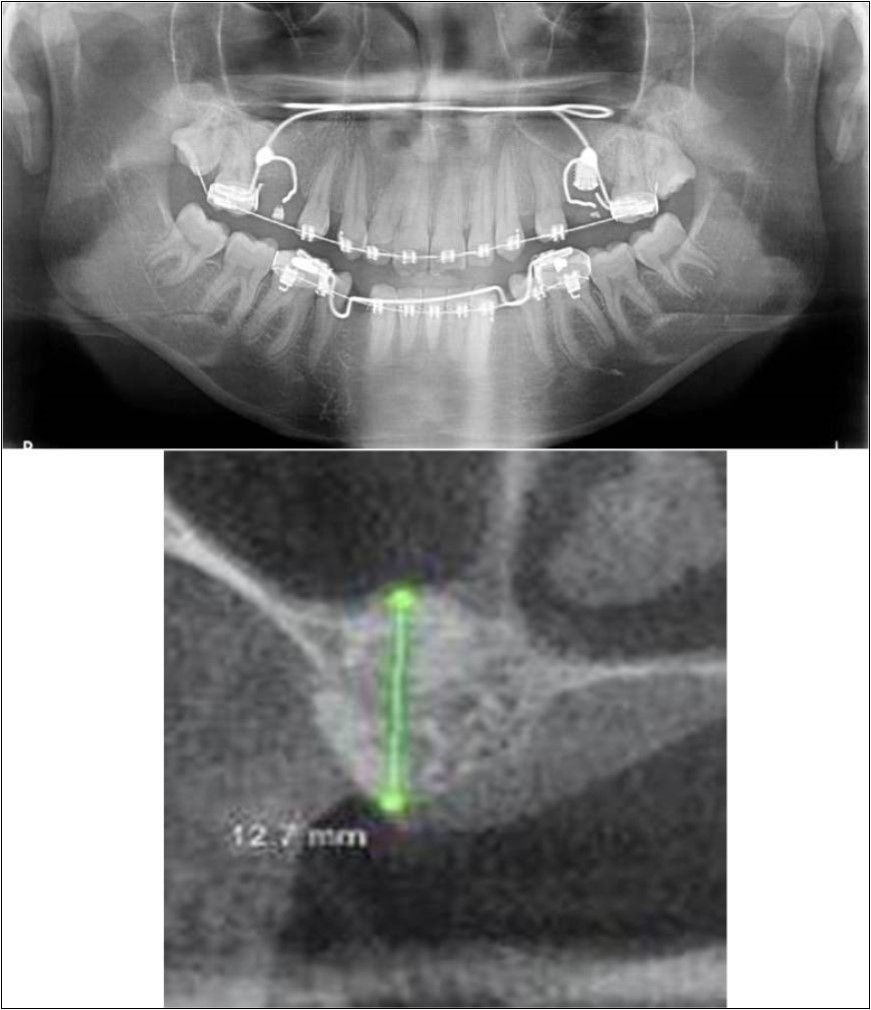
Case Report 5:
A 63 years old male patient reported to the Department of Oral and Maxillofacial Surgery, D.A.P.M.R.V Dental College and Hospital seeking options for implant prosthesis for replacement of missing teeth in upper left back tooth region. The teeth were extracted two years ago because of extensive caries and failure of root canal treated 26, 27. No prosthetic rehabilitation was carried-out in the past. Patient was a known case of diabetes mellitus since 20 years which was under control and was on medication for the same. His general health was satisfactory with no other co-morbidities. Patient did not give history of any existing sinus pathologies.
Clinical and Radiological Assessment:
1.Partially edentulous maxillary arch with missing 24, 25, 26, 27, 28;
2.Increased pneumatisation of left maxillary sinus;
3.Height of available bone- 2.5mm;
4.Transverse thickness of available bone (CBCT evaluation)- 10.9mm;
5.Inter-ridge space adequate to place implant (12mm).
Treatment:
Patient underwent the procedure of direct sinus elevation using sinus lateral approach kit. After crestal and vertical release incisions, muco-periosteal flap was raised to expose the buttress region. A bony window of 1cm diameter was created; sinus lining identified and elevated up to receive calcium phosphosilicate as graft material and closure was achieved under local anaesthesia and strict aseptic protocols. Implant placement was planned to be carried-out after a period of 6 months to allow for the consolidation for graft and naive bone formation. At the end of 6 months, a repeat CBCT scan was advised to evaluate the increase in bone height. (Figure 15a,b, pre-treatment; Figure 16a,b, post-treatment)
Figure 15.a,b. Pre-treatment OPG and cross section of CBCT showing residual alveolar bone height for Case No.5;
Figure 16.a,b. Post-treatment OPG and cross section of CBCT showing residual alveolar bone height for Case No.5;
Case Report 6:
A 25 years old young male patient reported to the Department of Oral and Maxillofacial Surgery, D.A.P.M.R.V Dental College and Hospital seeking options for implant supported prosthesis for rehabilitation of missing right first molar. The tooth was extracted 6 months ago because of gross loss of tooth structure and poor prognosis for root canal treatment. Patient did not give history of any existing sinus pathologies. All possible rehabilitative options were explained to the patient and a treatment plan of replacement of missing tooth with implant supported prosthesis was finalized.
Clinical and Radiological Assessment:
1.Partially edentulous maxillary arch with missing 16;
2.Increased pneumatisation of right and left maxillary sinus;
3.Height of available bone- 1.8mm;
4.Transverse thickness of available bone (CBCT evaluation)- 6.2mm;
5.Implant supported prosthesis i.r.t 35 and 36;
6.Fixed partial denture i.r.t 45, 46, 47;
7.Inter-ridge space adequate to place implant (12mm).
Treatment:
Patient underwent the procedure of direct sinus elevation using sinus lateral approach kit. After crestal and vertical release incisions, muco-periosteal flap was raised to expose the buttress region. A bony window of 1cm diameter was created; sinus lining identified and elevated up to receive calcium phosphosilicate as graft material and closure was achieved under local anaesthesia and strict aseptic protocols. Implant placement was planned to be carried-out after a period of 6 months to allow for the consolidation for graft and naive bone formation. At the end of 6 months, a repeat CBCT scan was advised to evaluate the increase in bone height. (Figure 17a,b, pre-treatment; Figure 18a,b, post-treatment)
Figure 17.a,b. Pre-treatment OPG and cross section of CBCT showing residual alveolar bone height for Case No.6;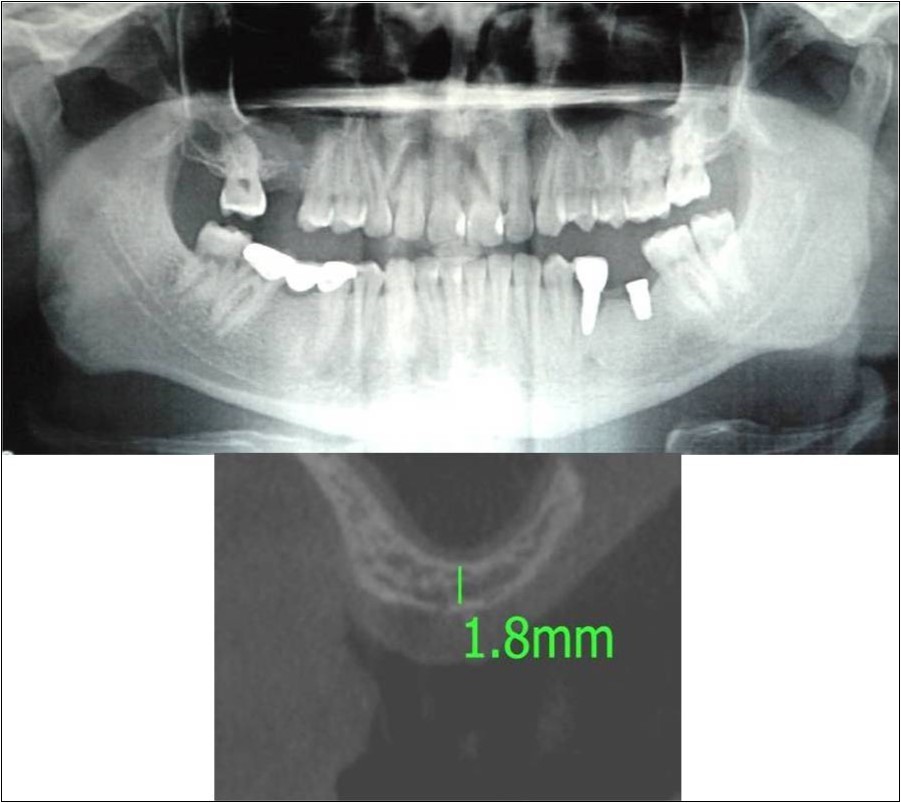
Figure 18.(a,b) Post-treatment OPG and cross section of CBCT showing residual alveolar bone height for Case No.6;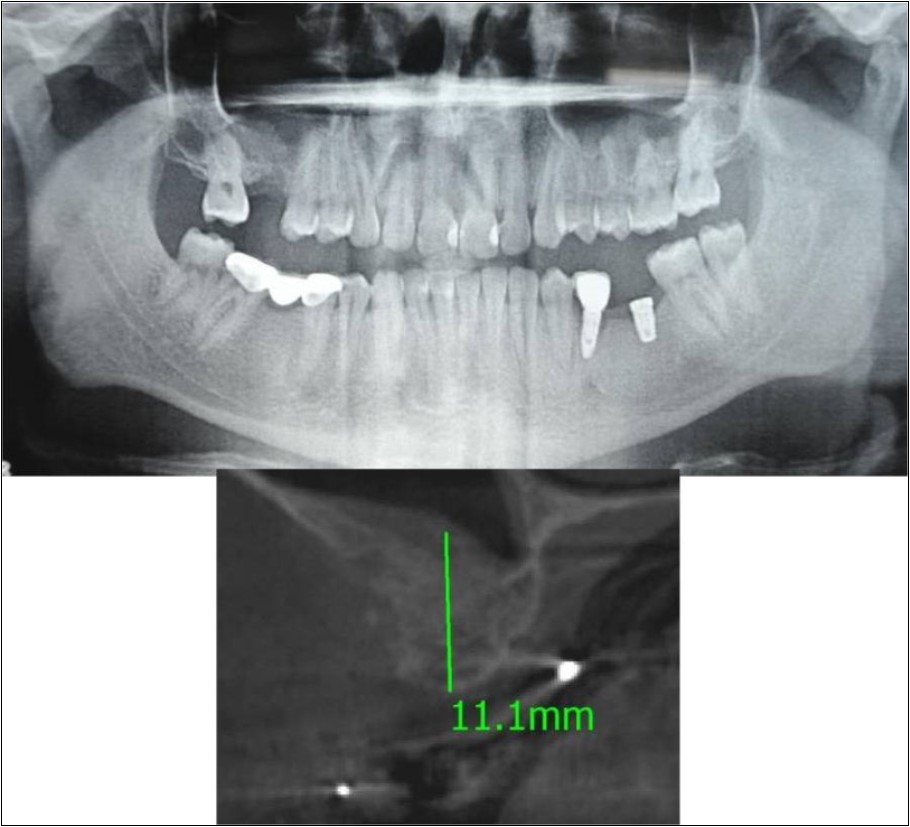
Results:
This study aimed at evaluating the use of calcium phosphosilicate (CPS) putty for its efficacy in enhancing bone regeneration following sinus lift procedures. Calcium phosphosilicate putty, being an alloplastic material in putty form, had an advantage of easy and convenient dispensing at the intended site after the sinus lift procedures. Regenerative potential was radiographically evaluated by assessing the increase in bone height of the alveolar ridge which was a direct determinant of the efficiency of calcium phosphosilicate putty as an alloplastic graft material. This prospective study included a sample of 20 segments requiring sinus augmentation either by an indirect or a direct approach. The study included 9 males (53%) and 8 females (47%) with a mean age of 46.05 years. The gender distribution in the indirect sinus augmentation was 4 males and 6 females while in direct sinus augmentation, there were 6 males and 3 females. 2 patients (one male and one female) underwent both direct and indirect sinus augmentation on their right and left maxillary quadrants in this study. The pre-operative height of bone ranged from 5.3mm to 7.7mm with an average being 6.8mm while the post-operative height of bone ranged from 10mm to 13mm with the average bone height being 11.86mm in case of indirect sinus augmentation procedures as measured by CBCT. A paired sample t-test was carried-out to know the difference between pre-and post-treatment measurements of bone height with indirect sinus augmentation procedures wherein the post-treatment bone height (11.86+1.11mm) was found to be significantly higher than the pre-treatment bone height (6.8 +0.70mm) (t=12.9, p<0.005). (Table 1)
Table 1. Comparison of mean Pre-and post-treatment bone height with Indirect Sinus Augmentation measured by CBCT| Indirect Sinus Augmentation | Bone Height (mm) | Difference | Paired t-test | ||
| Mean | Std. Deviation | t | p-value | ||
| Pre-treatment | 6.8 | 0.7 | 5.06 + 1.24 | 12.9 | <0.005 (Significant) |
| Post- treatment | 11.86 | 1.11 | |||
In case of direct sinus augmentation group, the pre-operative height of bone ranged from 1.5mm to 4mm with the average height being 2.44mm while the post-operative height of bone ranged from 10.2mm to 12.2mm with an average bone height being 11.27mm as measured by CBCT. A paired sample t-test carried-out in this group also revealed the post-treatment bone height (11.27 +0.71mm) to be significantly higher than the pre-treatment bone height (2.44 +0.81mm) (t=32.17, p<0.005). (Table 2)
Table 2. Comparison of mean Pre-and post-treatment bone height with Direct Sinus Augmentation measured by CBCT| Direct Sinus Augmentation | Bone Height (mm) | Difference | Paired t-test | ||
| Mean | Std. Deviation | t | p-value | ||
| Pre-treatment | 2.44 | 0.81 | 8.83 + 0.9 | 32.17 | <0.005 (Significant) |
| Post- treatment | 11.27 | 0.71 | |||
In case of OPG, the average pre-operative height of bone came-out to be 7.2mm while 10.2mm was the post-operative height of bone in case of indirect sinus augmentation procedures. A paired sample t-test was carried-out to know the difference between pre-and post-treatment measurements of bone height with indirect sinus augmentation procedures wherein the post-treatment bone height (10.2+0.92mm) was found to be significantly higher than the pre-treatment bone height (7.2 +1.23mm) (t=10.06, p<0.005). (Table 3)
Table 3. Comparison of mean Pre-and post-treatment bone height with Indirect Sinus Augmentation measured by OPG| Indirect Sinus Augmentation | Bone Height (mm) | Difference | Paired t-test | ||
| Mean | Std. Deviation | t | p-value | ||
| Pre-treatment | 7.2 | 1.23 | 3.0 + 0.94 | 10.06 | <0.005 (Significant) |
| Post- treatment | 10.2 | 0.92 | |||
In case of direct sinus augmentation group, the average pre-operative height of bone came-out to be 1.3mm while 8.85mm was the post-operative height of bone. A paired sample t-test carried-out in this group also revealed the post-treatment bone height (8.85 +1.00mm) to be significantly higher than the pre-treatment bone height (1.3 +0.92mm) (t=19.33, p<0.005). (Table 4)
Table 4. Comparison of mean Pre-and post-treatment bone height with Direct Sinus Augmentation measured by OPG| Direct Sinus Augmentation | Bone Height (mm) | Difference | Paired t-test | ||
| Mean | Std. Deviation | t | p-value | ||
| Pre-treatment | 1.3 | 0.92 | 7.55 + 1.23 | 19.33 | <0.005 (Significant) |
| Post- treatment | 8.85 | 1 | |||
A comparative analysis of mean pre-treatment bone height with indirect sinus augmentation as measured by OPG and CBCT concluded with the values of 7.2 +1.23mm in case of OPG while 6.8 +0.70mm in case of CBCT with t=1.48, and p=0.173 which was not found to be statistically significant. (Table 5)
Table 5. Comparison of mean Pre-treatment bone height with Indirect Sinus Augmentation measured by OPG and CBCT| Pre-treatment | Bone Height (mm) | Difference | Paired t-test | ||
| Mean | Std. Deviation | t | p-value | ||
| OPG | 7.2 | 1.23 | 0.4 + 0.86 | 1.48 | 0.173 (Not significant) |
| CBCT | 6.8 | 0.7 | |||
Similarly, a comparative analysis of mean post-treatment bone height with indirect sinus augmentation as measured by OPG and CBCT came-out with values of 10.2+0.92mm in case of OPG while 11.86+1.11mm in case of CBCT with t=10.39, and p<0.005 which was statistically significant. (Table 6)
Table 6. Comparison of mean Post-treatment bone height with Indirect Sinus Augmentation measured by OPG and CBCT| Post-treatment | Bone Height (mm) | Difference | Paired t-test | ||
| Mean | Std. Deviation | t | p-value | ||
| OPG | 10.2 | 0.92 | 1.66 + 0.84 | 6.21 | <0.005 (Significant) |
| CBCT | 11.86 | 1.11 | |||
A comparative analysis of mean pre-treatment bone height with direct sinus augmentation as measured by OPG and CBCT concluded with the values of 1.3 +0.92mm in case of OPG while 2.44 +0.81mm in case of CBCT with t=10.39, and p<0.005 which was statistically significant. (Table 7)
Table 7. Comparison of mean Pre-treatment bone height with Direct Sinus Augmentation measured by OPG and CBCT| Pre-treatment | Bone Height (mm) | Difference | Paired t-test | ||
| Mean | Std. Deviation | t | p-value | ||
| OPG | 1.3 | 0.92 | 1.14 + 0.35 | 10.39 | <0.005 (Significant) |
| CBCT | 2.44 | 0.81 | |||
Similarly, a comparative analysis of mean post-treatment bone height with direct sinus augmentation as measured by OPG and CBCT came-out with values of 8.85 +1.00mm in case of OPG while 11.27 +0.71mm in case of CBCT with t=8.71, and p<0.005 which was statistically significant. (Table 8)
Table 8. Comparison of mean Post-treatment bone height with Direct Sinus Augmentation measured by OPG and CBCT| Post-treatment | Bone Height (mm) | Difference | Paired t-test | ||
| Mean | Std. Deviation | t | p-value | ||
| OPG | 8.85 | 1 | 2.42 + 0.88 | 8.71 | <0.005 (Significant) |
| CBCT | 11.27 | 0.71 | |||
A comparison of mean increase in bone height with indirect sinus augmentation measured by OPG and CBCT concluded with the values of 3.00+0.94mm in case of OPG while 5.06+1.24mm in case of CBCT with t=7.15, and p<0.005 which was found to be statistically significant. (Table 9)
Table 9. Comparison of mean increase in bone height with Indirect Sinus Augmentation measured by OPG and CBCT| Indirect Sinus Augmentation | Increase in Bone Height (mm) | Mean Difference | Unpaired t-test | |
| (Mean + SD) | t | p-value | ||
| OPG | 3.00 + 0.94 | 2.06 + 0.91 | 7.15 | <0.005 (Significant) |
| CBCT | 5.06 + 1.24 | |||
| Direct Sinus Augmentation | Increase in Bone Height (mm) | Mean Difference | Unpaired t-test | |
| (Mean + SD) | t | p-value | ||
| OPG | 7.55 + 1.23 | 1.28 + 0.92 | 4.39 | <0.005 (Significant) |
| CBCT | 8.83 + 0.87 | |||
Similarly, a comparison of mean increase in bone height with direct sinus augmentation measured by OPG and CBCT concluded with the values of 7.55+1.23mm in case of OPG while 8.83+0.87mm in case of CBCT with t=4.39, and p<0.005 which was also found to be statistically significant. (Table 10)
A paired sample t-test was also carried-out to know the difference in original and grafted sinus floor measurements for bone density (Grayscale values) with indirect as well as direct sinus augmentation procedures wherein the post-treatment bone grafted sinus floor measurements (1107.6 + 155.6mm) were found to be significantly higher than the original sinus floor measurements of bone density (Grayscale values) (412+ 65.5mm) (t=16.6, p<0.001) in case of indirect sinus augmentation procedures. Similarly, the post-treatment bone grafted sinus floor measurements (1169.6+136.7mm) were found to be significantly higher than the original sinus floor measurements of bone density (Grayscale values) (416.4+ 0.70mm) (t=17.9, p<0.001) in case of direct sinus augmentation group, however, when the difference between the original and grafted sinus floor measurements obtained was compared amongst the indirect and direct sinus augmentation groups, the difference was not found to be statistically significant.
Discussion:
A successful implant therapy requires the presence of an adequate quantity and quality of bone .With advancing age and loss of teeth, there is depletion of bone quantity and quality in both the maxillary as well as mandibular arches but the posterior maxillary region presents with an addition challenge with increased pneumatisation of the maxillary sinus further posing with an additional anatomic constraint for implant based rehabilitation procedures. Following tooth extraction, edentulous areas continue to atrophy causing increased antral pneumatisation due to increased osteoclastic activity of the periosteum of the Schneiderian membrane, affecting the overall bone height and density. Lekholm and Zarb developed a grading scheme for the quality of bone in the proposed implant site in terms of the relative proportion and density of cortical and medullary bone and divided the bone of the alveolar process into 4 classes:
1.Almost the entire jawbone is composed of homogeneous compact bone (D1);
2.A thick layer of compact bone surrounds a core of dense trabecular bone (D2);
3.A thin layer of compact bone surrounds a core of dense trabecular bone of favorable strength (D3);
4.A thin layer of compact bone surrounds a core of low density trabecular bone (D4).
On assessment, the D3 type of bone is composed of thinner porous cortical bone on the crest and fine trabecular bone within the ridge. The trabecula in D3 type is not only fifty percent weaker than those in D2 bone, the bone-implant contact is also less favorable. These additive factors increase the risk of implant failure. In D4 type of bone, the density is very poor with little or no cortical crestal bone and is most commonly seen in the posterior regions of the maxilla. Its bony trabeculae may be upto ten times weaker and sparse than the cortical bone of D1 and the bone-implant contact after initial loading is often less than twenty five percent. This can prove as a surgical challenge for the initial fixation of any implant design. Maxillary sinus augmentation has become a pivotal replacement procedure in advanced implant dentistry. A sinus-lift procedure was first performed by Dr. Hilt Tatum Jr in 1974 during his period of preparation to begin sinus grafting. In keeping with the past provinces, currently, two proficient techniques of sinus floor elevation for dental implant placements are in use: a lateral window approach followed by implant placement as a two-stage technique and a one-stage, lateral or trans-crestal approach. The decision to use one these techniques is primarily based on the amount of residual bone and on the possibility of achieving primary stability of the implants. Depending on the available bone height, Carl E Misch developed a protocol to categorize implant placement in posterior maxilla. In the same context, the relation between residual bone height and the success of implants has been analyzed and described by various authors. In a landmark review study, which analyzed 349 implants for a mean follow-up period of 3.2 years, the observations of the study showed that the majority of implants, which were lost and subsequently, led to failures, were placed in the residual bone height of <4mm.11 In 2003, Wallace and Froum studied the effect of maxillary sinus floor elevations and the survival of dental implants and concluded that the survival rate of implants placed with the lateral approach technique was at an average 91.8%.12 When implants were placed in grafted sinuses, rough surfaced implants yielded higher survival rates than the machined surface implants. For implants inserted in osteotome mediated sinus floor elevation, another excellent review paper by Tan WC and Pjetursson BE provided data on the survival of a total of 12,020 implants revealing a 3-year implant survival of 90.1%.13 These results were comparable to yet another study by Geurs et al in 2001 inferring that the amount of residual bone height significantly influences the implant survival after sinus floor elevations.14 In our study, 10 patients qualified for the SA-3 of Misch’s criteria out of whom 60% were males and 40% were females. We followed the technique described by Summers and showed a success rate of 100% in comparison to Summers study which showed a 96% success rate.15 This marginal increase in success rate could partly be attributed to the short term follow-up for upto 6 months in comparison to a period of 5 years in the said study. Hitherto, the most important parameters to be considered for successful sinus augmentation include the cortical irregularity, trabecular bone density, amount of bone available for implant placement and the orientation of the alveolar bone. While the success of the implants in indirect sinus elevation procedures is mainly dependent on the residual bone height and the type of implants used, success of direct augmentations in a two stage procedure is mainly attributed to the quality of bone formed and the height achieved post-operatively. A study on histo-morphometric bone analysis has shown that the bone formed following the direct sinus augmentation procedures consisted of 35% and 65% of lamellar bone and woven bone respectively and the bone density formed was of the D3-D4 quality which is a poor quality bone with questionable stability for osseo-integration of implants.16 While our study was performed as per vigilant treatment protocols, statistical analysis was done as a sequel. When a paired sample t-test was carried-out to know the difference in pre-and post-treatment bone height with indirect sinus augmentation procedures, it was seen that the post-treatment bone height (11.86 + 1.11) was significantly higher than the pre-treatment bone height (6.80+0.70) (t=12.9, p<0.005) as measured by CBCT. This was congruent with the direct sinus augmentation procedures wherein the post-treatment bone height (11.27 +0.71) was significantly higher than pre-treatment bone height (2.44 +0.81) (t=32.17, p<0.005). The results obtained were in accordance with the study conducted by Seung-MiJeong. Although our study achieved a greater increase in average bone height, it involved a comparatively smaller sample size with less number of implants placed.17 Contributory researches have shown that in order to achieve a substantial increase in bone height, use of graft material is mandatory. Autogenous bone graft is the gold standard for such procedures due to its osteogenic potential. Allogenous grafts such as decalcified freeze dried bone grafts are inappropriate bone substitutes because of the risk of transmission of diseases and pronounced eventual resorptions. Due to the various limitations of autologous and allogenous graft materials, alloplastic materials are gaining popularity because of their ease of availability and improved results in bone regeneration. However, their use alone is limited when the volume required for grafting is exceptionally high. According to the review paper by Tan WC and Pjetursson BE, autogenous bone and bone substitutes showed significantly lower annual failure rates (1.47%) than bone substitutes used alone as graft material.18 It must, however, be kept in mind that all types of graft materials have high survival rates ranging between 96.3% and 99.8% after 3 years as concluded from various studies conducted. When implants were grouped according to the surgical technique utilized i.e. one stage or two stage sinus augmentations, it was concluded that the implants inserted with the one stage technique had a slightly higher survival rate than implants inserted with the two stage procedures. The utilization of grafts consisting of 100% autogenous bone or the inclusion of autogenous bone as a component of composite grafts did not affect implant survival. Hence, alloplastic bio-composite material can be used alone and in preference to other materials available. Calcium phosphosilicate (CPS) putty biomaterial (FDA 510, 2006) is a third generation biomaterial which has been able to achieve results similar to autogenous bone grafts. This material has recently attracted attention due to its osteo-conductive and osseo-stimulative properties i.e. its ability to stimulate osteo-progenitor cells.19 When implanted, this material undergoes both physical and chemical dissolution as a result of ion release mechanism and leads to the formation of hydroxyl carbonite apatite (HCA). It is a pre-mixed moldable material consisting of four components including two bioactive phase components, a 55% standard CPS particulate and a 14% CPS smaller particulate in addition to 12% polyethylene glycol additive phase and 19% glycerine binder phase. Bioactivity is initiated immediately upon implantation. The smaller CPS particles release calcium and phosphorous ions into the area while the binder material gets absorbed over a period of a week exposing the larger CPS particulates to blood. In calcium phosphosilicate, the particle sizes are in micrometer size range of 90-710 micrometer range, irregular, in both size and shape. According to Moore et al, in 2001, bioactive glass granules are more quickly reabsorbed than hydroxyapatite, thus, allowing a much more precocious new bone formation in the repair of bone defects.7 On them, osteoblasts show several cytoplasmic processes, pseudopodia, compact appearance, and disorderly dorsal surface, which is characterized by a high cell membrane activity. Therefore, as to the adhesion and close contact between osteoblasts, bioactivity is considered crucial to the development of new bases for bone tissue bioengineering. Its use in various fields, due to its excellent biocompatibility and its physical and chemical properties, has encouraged studies on the feasibility of implant coating, so as to obtain better biologic fixation, and also as a carrier of osteo-inductive substances such as bone morphogenic proteins and other growth factors.8, 9 Other authors also demonstrated the effectiveness of bioactive glass as they improved the osseo-integration of coated implants providing better bone support and presenting with an increased stability when compared to the machined implants.10 To brief, CPS consists mainly of 2 phases: a Phase 1 (bioactive glass particles of 90-710microns) and Phase 2 (calcium phosphosilicate particles of sizes ranging from 32 to 125microns). It provides a Young’s modulus of 30–35GPa, which is close to that of cortical bone. Following its placement into the sinus cavity and clot formation, the smaller particles of the phase 2 release an initial burst of calcium and phosphorous and form a virtual porous network in the defect. Spaces between the particles promote bone in-growth and create multiple foci of osseous regeneration through the defect, thus, enhancing the rate of bone formation. Also, due to its osseo-stimulative properties on osteoblasts, the osteoblasts undergo recruitment, proliferation and differentiation at the site of defect. This stimulation leads to increased DNA content and elevated osteo-calcin and alkaline phosphatase levels. Moreover Xynos et al, described modulation of osteoblastic cell cycle by a controlled release of ionic dissolution products from CPS particles.20 High percentage of vital bone content after a relatively short healing phase suggests that bioactive calcium phosphosilicate putty can be a reliable choice for osseous regeneration in cases of crest preservation and implant related surgeries. Osseous regenerative potential of CPS putty has been explored through histological analysis of the sites grafted with CPS and a plenitude of human clinical studies have verified the findings. Histo-morphometric results from the use of CPS putty in well-contained defects have been very promising providing a vital bone from 31% to 49% depending upon the healing time. Additionally, previous histological studies have verified the positive effects of CPS particles in the percentage of vital bone present in extraction sockets and in augmented maxillary sinuses. A prime pre-requisite for a predictable success of these procedures, however, solely depends on gathering information on quantity and quality of bone available for implant placement and to localize the anatomical structures which is of utmost importance. Dental implant imaging, thus, provides information about the implant site with regards to the osseous morphology, developmental variations, post-extraction irregularities and approximation of the crest of the ridge to the sinus floor, in addition to pneumatisation of the maxillary sinuses and presence of septae (in case of posterior maxilla) which do influence the success and outcome of the procedure. Investigating our study on radiological grounds, orthopantomographs (OPGs)/panoramic imaging are worth mentioning. Panoramic radiographs have previously been used to study the grafted sinus floors and their relationship with dental implants. The panoramic radiographs, with an effective dose of 16-28 microSv, and variable exposure parameters (including Kvp, mA, and time in seconds depending on the manufacturers) are the most commonly used radiographic tools for implant assessment. However, the position of the maxillary sinus floor may be difficult to assess on these two-dimensional radiographs primarily due to poor visualization and superimpositions inherent in these types of radiographic projections. Also, panoramic radiography has the disadvantage of magnification in horizontal as well as vertical dimensions which might derogate the diagnostic information desired from these radiographs. Due to these disadvantages, there has been a shift toward the more advanced three dimensional, cross-sectional imaging modalities, with the computed tomography (CT) scans enabling the evaluation of the proposed implant sites and providing diagnostic information that varied imaging techniques cannot possibly provide. Computed tomography (CT) scans have several advantages over conventional radiography. First, CT scans eliminate the superimposition of images of structures outside the area of interest. Second, because of the inherent contrast and high resolution in CT scans, differences between the tissues that differ in physical density of less than 1% can be distinguished as against conventional radiography which requires a minimum of 10% difference in physical density to distinguish between tissues. Third, the data from a single CT imaging procedure consists of either multiple contiguous or one helical scan. This can be viewed as images in the axial, coronal or sagittal planes or in any arbitrary plane depending on the diagnostic information desired. Denta Scan (CT for implant assessment) provides programmed reformatting of the images and organization and display of the imaging study. The radiologist simply indicates the curvature of the maxillary and mandibular arches and the computer is programmed to generate referenced cross-sectional and tangential or panoramic images of the alveolus along with three-dimensional images of the arch. The cross-sectional and panoramic images are spaced 1mm apart and enable accurate pre-operative treatment planning.21 The utility of CT for dental implant treatment planning is evident but access to these imaging techniques is still limited due to either limited availability or, not being so cost-effective as against the conventional radiological investigative procedures. Nevertheless, CT scans are not without their limitations/concerns such as a high radiation exposure (240-1200 microSv) and obviously, a higher cost as already mentioned and a huge carbon footprint.22, 23, 24 Due to these factors associated with CT scans, Cone Beam Computed Tomography (CBCT) was developed. As the name implies, CBCT generates well-collimated, cone-shaped beams and the images are acquired in only one rotation by an image intensifier of flat panel detector resulting in reasonably low levels of radiation dosage (42-50 microSv) with an added advantage of higher resolution due to narrowly collimated, cone-shaped beam.25, 26, 27 During the rotation, multiple sequential planar projection images in the field of view (FOV) are acquired in a complete or partial arch which provides a shorter examination time, increased x-ray tube efficiency, reduced image unsharpness caused by the translation of the patient and image distortion caused due to internal patient movements. 3D planar imaging dedicated to the maxillofacial region at low cost and low dose of radiation, thus, makes CBCT a lucrative modality of imaging. Due to the various above mentioned advantages, we intended to use CBCT scans for the height evaluation over the conventional two-dimensional radiographs and computed tomography. In accordance to our study, a study by Nishida et al, in 2013, assessed the radiographic appearance of bone graft domes longitudinally after osteotome sinus floor elevation using cone beam computed tomography (CBCT) scans. This study presents the radiological findings of a 6 months follow-up CBCT study in maxillary osteotome sinus floor elevation procedures. Implant survival was dependent on both bone quantity and quality. Bone mineral density (quality) was of extreme importance for primary implant stability, especially when considering either the immediate loading protocol. Investigating our study further, we conducted paired samples t-test to know the difference in original and grafted sinus floor measurements of bone density (Grayscale values) with indirect as well as direct sinus augmentation procedures. The post-treatment bone grafted sinus floor measurements (1107.6 + 155.6mm) were found to be significantly higher than the original sinus floor measurements of bone density (Grayscale values) (412+ 65.5mm) (t=16.6, p<0.001) in case of indirect sinus augmentation procedures. Similarly, the post-treatment bone grafted sinus floor measurements (1169.6+136.7mm) were found to be significantly higher than the original sinus floor measurements of bone density (Grayscale values) (416.4+ 0.70mm) (t=17.9, p<0.001) in case of direct sinus augmentation group. The outcome of this study suggested that CBCT can be used as a potential tool in predicting the success of grafting in direct and indirect sinus augmentation procedures and is highly recommended in all cases to improve surgeon’s confidence and the accuracy of the sinus lift procedures. Whatever the place or period, surgical complications have been an inevitable part of the surgical practice. The most common intra-operative complication reported was the perforation of the sinus membrane ranging from 0-58.3%. However, controversy still hovers whether this complication influences the survival rate of the implants. Some authors reported a correlation between membrane perforation and implant failure while other studies did not report any such correlation.28 Perforations are usually closed by using tissue fibrin glue, suturing or by covering them with a resorbable barrier membrane. However, in our study, we encountered displacement of implant into the sinus during the time of the implant placement due to widening of the osteotomy site. The implant was retrieved methodically via Caldwell-Luc approach and a larger size (4 x 11.5mm) implant was placed for acceptable implant stability. Physiological adaptation of sinus mucosa has been proven experimentally leading to development of chronic sinusitis after maxillary sinus floor augmentations. Penetration of the sinus by implants might further increase the risk of infections and can be regarded as a contraindication. However, Branemark et al in 1984, reported that sinus penetration by implants caused no undesirable effects.29 Wallace experienced only 7 of 100 cases of Schneiderian membrane perforation in their study when using piezosurgery.30 Similarly, Vercelloti et al, in his study observed perforation of the Schneiderian membrane in only 5% of patients.31 Although in our study, sinus membrane perforation was encountered in 1 of the 17 patients, which was due to the adherence of the membrane onto the medial surface of the bony window, favorably, we did not encounter any complications associated with the perforation and healing occurred uneventfully despite the fact that no corrective procedures were carried-out for the membrane perforation. CPS putty material proved to be highly efficient with excellent ease of handling and dispensing characteristics. Apart from the superior results obtained with the use of CPS as a graft material of choice, the patients with severely atrophic maxillae, enrolled in the study, had immensely positive response to treatment as never before, with respect to the vertical bone height achieved, increased bone density and superior quality of post-operative trabecular bone formation. We were able to bring in explicitly informative result about the components of the studies and the superior outcome of our prospective study on patient management. Also, CBCT scans proved to be an effective tool for the radiographic assessment of various parameters (height, width and density) and surgical anatomy of the maxillary sinus pre-operatively and in quantifying the results achieved post-operatively.
Limitations of the study:
An insight into the impediment of the present study suggested the following limitations overcoming which the value of the study would have increased significantly:
Histo-morphometric analysis was not done to evaluate the quality of bone formed;
Small sample size with a relatively short term follow-up;
Osseo-integration of implants was not considered.
Conclusion:
Use of CBCT scans gave exact and precise details of the naive and augmented bone after a period of 6months;
Calcium Phosphosilicate (CPS) was accepted well at the recipient sites without any complications demonstrating its efficiency and reliability in sinus augmentation procedures;
In indirect sinus augmentation group, the implants had osseo-integrated well, thus, confirming the efficiency of Calcium Phosphosilicate (CPS) and the technique of its usage.
References
- 1.Kent J N, Block M S. (1989) Simultaneous maxillary sinus floor bone grafting and placement of hydroxylapatite-coated implants. , Journal of Oral and Maxillofacial Surgery; 47, 238-242.
- 2.Jensen J, Simonsen E K, Sindet-Pedersen S. (1990) Reconstruction of the severely resorbed maxilla with bone grafting and osseointegrated implants: A preliminary report. , Journal of Oral and Maxillofacial Surgery; 48, 27-32.
- 3.Blomqvist J E, Alberius P, Isaksson S, Linde A, Obrant K. (1998) Importance of bone graft quality for implant integration after maxillary sinus reconstruction. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology and Endodontics;. 86, 268-274.
- 4.Jensen J, Sindet-Pedersen S. (1991) Autogenous mandibular bone grafts and osseointegrated implants for reconstruction of the severely atrophied maxilla: A preliminary report. , Journal of Oral and Maxillofacial Surgery; 49, 1277-1287.
- 5.Jurisic M, Markovic A, Radulovic M, Brkovic B M, Sandor G K. (2008) Maxillary sinus floor augmentation: Comparing osteotome with lateral window immediate and delayed implant placements: An interim report. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology and Endodontics;. 106, 820-827.
- 6.Merkx M A, Maltha J C, Stoelinga P J. (2003) Assessment of the value of anorganic bone additives in sinus floor augmentation: A review of clinical reports. , International Journal of Oral and Maxillofacial Surgery; 32, 1-6.
- 7.Moore W R, Graves S E, Bain G I. (2001) Synthetic bone graft substitutes. , ANZ Journal of Surgery; 71, 354-361.
- 8.Hamadouche M, Meunier A, Greenspan D C, Blanchat C, Zhong J P et al. (2000) Bioactivity of sol-gel bioactive glass coated alumina implants. , Journal of Biomedical Materials Research; 52, 422-429.
- 9.Keeting P E, Scott R E, Colvard D S, Anderson M A, Oursler M J et al. (1992) Development and characterization of a rapidly proliferating, well-differentiated cell line derived from normal adult human osteoblast-like cells transfected with SV40 large T antigen. , Journal of Bone and Mineral Research; 7, 127-136.
- 10.Turunen T, Peltola J, Helenius H, Yli-Urpo A, Happonen R P. (1997) Bioactive glass and calcium carbonate granules as filler material around titanium and bioactive glass implants in the medullar space of the rabbit tibia. Clinical Oral Implants Research;. 8, 96-102.
- 11.Jensen O T, Shulman L B, Block M S, Iacono V J. (1998) . Report of the Sinus Consensus Conference of1996. The International Journal of Oral and Maxillofacial Implants1998; 13, 11-45.
- 12.Wallace S S, Froum S J. (2003) Effect of maxillary sinus augmentation on the survival of endosseous dental implants: A systematic review. Annals of periodontology2003;. 8, 328-343.
- 13.Pjetursson B E, Tan W C, Zwahlen M, Lang N P. (2008) A systematic review of the success of sinus floor elevation and survival of implants inserted in combination with sinus floor elevation. , Journal of Clinical Periodontology2008; 35, 216-240.
- 14.Geurs N C, Wang I C, Shulman L B, Jeffcoat M K. (2001) Retrospective radiographic analysis of sinus graft and implant placement procedures from the. Academy of Osseointegration Consensus Conference on Sinus Grafts. The International Journal of Periodontics and Restorative Dentistry2001; 21, 517-523.
- 15.Summers R B. (1994) The osteotome technique: Part 3- Less invasive methods of elevating the sinus floor. , Compendium1994; 15, 698-700.
- 16.Xynos I D, Edgar A J, Buttery L D, Hench L L, Polak J M. (2001) Gene expression profiling of human osteoblasts following treatment with the ionic products of Bioglass 45S5 dissolution. , Journal of Biomedical Materials Research2001; 55, 151-157.
- 17.Komarnyckyj O G, London R M. (1998) Osteotome single-stage dental implant placement with and without sinus elevation: a clinical report. , The International Journal of Oral and Maxillofacial Implants; 13, 799-804.
- 18.Pjetursson B E, Tan W C, Zwahlen M, Lang N P. (2008) A systematic review of the success of sinus floor elevation and survival of implants inserted in combination with sinus floor elevation. , Journal of Clinical Periodontology2008; 35, 216-240.
- 19.Turunen T, Peltola J, Helenius H, Yli-Urpo A, Happonen R P. (1997) Bioactive glass and calcium carbonate granules as filler material around titanium and bioactive glass implants in the medullar space of the rabbit tibia. Clinical Oral Implants Research1997;. 8, 96-102.
- 20.Xynos I D, Edgar A J, Buttery L D, Hench L L, Polak J M. (2001) Gene expression profiling of human osteoblasts following treatment with the ionic products of Bioglass 45S5 dissolution. , Journal of Biomedical Materials Research2001; 55, 151-157.
- 21.Resnik L, Liu D, Hart D L, Mor V. (2008) Benchmarking physical therapy clinic performance: Statistical methods to enhance internal validity when using observational data. Physical Therapy2008;. 88, 1078-1087.
- 22.White S C, Pharoah M J. (2013) Oral Radiology: Principles and Interpretation: Elsevier - Health Sciences Division;.
- 23.Chan H L, Misch K, Wang H L. (2010) Dental imaging in implant treatment planning. Implant Dentistry2010;. 19, 288-298.
- 24.Scarfe W C, Farman A G. (2008) What is cone-beam CT and how does it work? Dental clinics of North America2008;. 52, 707-730.
- 25.Chan H L, Misch K, Wang H L. (2010) Dental imaging in implant treatment planning. Implant Dentistry2010;. 19, 288-298.
- 26.Scarfe W C, Farman A G. (2008) What is cone-beam CT and how does it work? Dental clinics of North America2008;. 52, 707-730.
- 27.Arai Y, Tammisalo E, Iwai K, Hashimoto K, Shinoda K. (1999) Development of a compact computed tomographic apparatus for dental use. Dento Maxillofacial Radiology1999;. 28, 245-248.
- 28.Khoury F. (1999) Augmentation of the sinus floor with mandibular bone block and simultaneous implantation: A 6-year clinical investigation. , The International Journal of Oral and Maxillofacial Implants1999; 14, 557-564.
- 29.Branemark P I, Adell R, Albrektsson T, Lekholm U, Lindstrom J et al. (1984) An experimental and clinical study of osseointegrated implants penetrating the nasal cavity and maxillary sinus. , Journal of Oral and Maxillofacial Surgery1984; 42, 497-505.