Abstract
Allergic angioedema of the airways is a potentially life-threatening condition. The allergen can be difficult to identify. Treatment in the acute phase comprises of antihistamines, steroids, adrenaline and in severe cases prophylactic intubation. Allergic angioedema can be encountered in all medical specialties including odontology. It can develop fast and emergency treatment is lifesaving. Knowledge of symptoms and emergency treatment is important.
We present a case of a 33-year-old female physician who in a matter of hours developed first an atypical urticarial eruption followed by angioedema of the upper airways. She was treated with antihistamines, as she refused other treatments due to lactation. The patient also refused further investigations, however she has not had any further episodes after discontinuing the ingestion of organic tea.
Allergic reactions are unpredictable and have a large variety of triggers. The most likely trigger in this case was fungicide in the organic tea.
Author Contributions
Academic Editor: Vinayak Raghunathan, Assistant Professor
Checked for plagiarism: Yes
Review by: Single-blind
Copyright © 2016 Susanne I Scott, et al
 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Competing interests
SIS has no conflicts of interests to declare.
ERR has received research grants from CLS Behring, Viropharma and Shire. She has furthermore received travel grants and payment for lectures from Shire and MSD Norway.
Citation:
Introduction
Angioedema is a potentially life-threatening condition, which can arise both due to mast-cell activation, but also due to increased levels of bradykinin or other vasoactive mediators. Angioedema can arise during or after dental treatment, but patients with recurrent angioedema can also seek assistance from their dentist, when the condition involves the perioral area or oral cavity. Hence it is an important condition to be able to identify.
Allergic reactions are a heterogeneous group, with mild contact dermatitis in one end of the spectrum to life-threatening anaphylaxis in the other. Angioedema (AE) is a common symptom during allergic reactions 1. AE is for all intentive purposes a clinical diagnosis. It presents as a non-pitting, subdermal swelling, which can be fatal if involving the upper airways including the tongue, pharynx or larynx to the point of obstruction 2. There are several different forms of AE including hereditary, allergic, iatrogenic, idiopathic and acquired (i.e. treatment with angiotensin converting enzyme-inhibitors or gliptins). Allergic AE is driven by the release of histamine and other vasoactive molecules from mast cells and basophilic granulocytes. The incidence of AE is not well described, but the overall lifetime prevalence of AE regardless of aetiology ranges from about 7-15% 3, 4. When minor angioedema episodes occurs in the lips or oral cavity, patients often consult a dentist, as they suspect infections of the teeth or a disease located to the salivary glands or mucosa. In children infections of the sinuses are in fact a significant risk factor for developing AE 5.
The treatment of allergic AE is first and foremost emergency treatment with antihistamine, steroids, adrenaline (when hypotension is present) and intubation or cricotomy in severe cases. Further investigations must be undertaken to identify the trigger, so this can be avoided. It is good practice to prescribe the patient an adrenaline auto-injector for use if a new episode develops, especially if the trigger is unidentified.
The prognosis depends on whether the trigger can be identified and whether cross allergy occurs.
Organic tea is produced using organic farming methods. In organic farming the use of synthetic substances such as synthetic pesticides or fertilisers are generally prohibited. However naturally occurring pesticides and fertilizers are allowed 6.
Chlorothalonil is a fungicide commercially available in a range of products and approved for general use by the U.S. Environmental Protection Agency 7, 8.
There are currently no available systematic reviews or randomised controlled trials investigating allergic reactions to ingested organic or non-organic tea.
Case
A previously healthy 33-year-old female physician with no known allergies developed 5mm itchy red elements in the gluteal region. A few hours later she developed a pressure induced urticarial rash on the thorax. A few minutes after that, shivering and a feverish sensation in the body occurs. Furthermore a tingling sensation in the tongue and cheeks as well as swelling of the lips and around the eyes developed (Figure 1A-D). When the patients symptoms progresses to a sensation of swelling in the throat and dyspnoea, she was rushed to hospital. In the ambulance she was given antihistamine with good treatment response. Upon arrival to the Emergency Department the sensation of throat swelling was subsiding and vital signs were normal. The patient refused treatment with corticosteroids, as she was lactating. She was admitted for observation, but self-discharged after a few hours with a two week course of oral antihistamines. The patient refused any further investigation of her allergy. In the days after the admission the patient experienced nightly worsening of the urticarial rash. She contacted a colleague (professor of dermatology and allergy) and he proposed fungicide in organic tea as the allergen. The patient had started drinking a new brand of organic tea every night a couple of weeks before the development of AE. When this was discontinued the urticarial rash resolved and there have been no relapses in the 6 months which has passed since the episode.
Figure 1.A) Urticarial rash of the back B) Urticarial rash on the wrist C) Urticarial rash and angioedema of the thorax – note the angioedematous areas where the patient has been scratching (characteristic pattern) D) Angioedema of lips and periorbital area.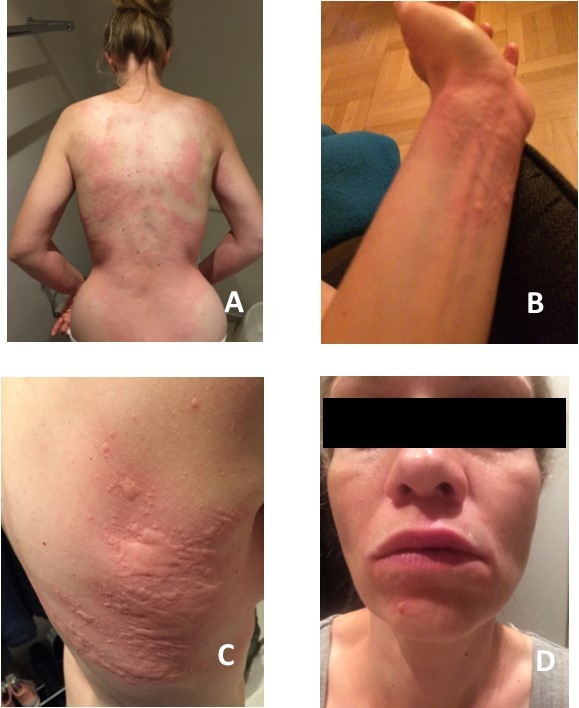
Discussion
The interesting thing to learn from this case is that it might be difficult to identify an allergen, as many patients do not themselves have an idea of the association. However by patiently going through the patient’s routines and newly introduced items (i.e. foods, perfume, clothing, and medicine) the suspected allergen can often be narrowed down to few items. Those items can then be withdrawn from the patient one by one to assess the effect on the symptoms. Unfortunately it was not possible to persuade the patient to undergo investigations to establish what triggered her AE. It is therefore impossible to ascertain the allergen with certainty. To further complicate the matter, the patient had several different types of organic tea from the same brand over the period from when she developed the first urticarial rash, until it resolved permanently. We are of the opinion that this case of AE was caused by an allergy to traces of fungicide. When searching the literature there are several reported cases of tea allergy, most of them are to one of the main flavour ingredients 9, 10. In this case, the patient has had all the same types and flavours of teas from a different brand since without any reaction. The authors are therefore convinced that the allergen must be something else in the teas, not the tea itself. Counterintuitively it is not illegal to use fungicides on organic crops. The law on the area varies from country to country. In Denmark, where the authors are from, the use of certain fungicides is legal in the context of acute danger of losing the crops, it is however not legal to use fungicides routinely 9, 10. Another possible allergen is a food additive in the organic tea. In a recently published review Skypala et al. describe allergy to food additives such as sulphites and benzoates 11.There are several described cases where fungicides have caused allergic reactions ranging from contact dermatitis, asthma to severe cases of AE and anaphylaxis. The fungicide chlorothalonil have been reported to cause all of the above, and is used in India where many herbs for Pukka tea is produced 12, 13.There are currently no available literature citing the incidence of angioedema after organic tea ingestion.
In conclusion, allergic AE is a medical emergency, which requires immediate treatment especially when involving the upper airways as obstruction and asphyxiation can occur. It is unfortunately not always possible to identify the allergen that triggered the episode, and health personnel can sometimes be challenging patients. It is our belief that the patient reacted to traces of fungicide, which to the best of our knowledge is the first reported case where ingestion of fungicide traces in organic tea has caused AE and anaphylaxis.
References
- 1.FER Simons, LRF Ardusso, Bilò M B, Dimov V, Ebisawa M et al. (2012) Update: World Allergy Organization Guidelines for the assessment and management of anaphylaxis. Curr Opin Allergy Clin Immunol. 12, 389-399.
- 2.Krizova A, Gardner T, Little D L, Arcieri-Piersanti V, Pollanen M S. (2015) Fatal laryngeal angioedema: a case report and a workup of angioedema in a forensic setting. Forensic Sci Med Pathol. 11, 558-563.
- 3.Madsen F, Attermann J, Linneberg A. (2012) Epidemiology of Non-hereditary Angioedema. Acta Derm Venereol. 92, 475-479.
- 4.Rasmussen E R, Fast S, Tagesen J, Bygum A. (2013) Angioedema with and without urticaria - a dental perspective. , Tandlaegebladet; 117, 474-480.
- 5.Krishnamurthy A, Naguwa S M, Gershwin M E. (2008) Pediatric angioedema. Clin Rev Allergy Immunol. 34, 250-259.
- 6. (2016) The National List | Agricultural Marketing Service [Internet].[cited2016May17]. Available from: https://www.ams.usda.gov/rules-regulations/organic/national-list.
- 7. (2016) Chlorothalonil - Toxipedia [Internet].[cited2016May17]. Available from: http://www.toxipedia.org/display/toxipedia/Chlorothalonil.
- 8. (2016) EXTOXNETPIP - CHLOROTHALONIL [Internet].[cited2016May17]. Available from: http://extoxnet.orst.edu/pips/chloroth.htm.
- 9.Andres C, Chen W C, Ollert M, Mempel M, Darsow U et al. (2009) Anaphylactic reaction to camomile tea. Allergol Int. 58, 135-136.
- 11.Skypala I J, Williams M, Reeves L, Meyer R, Venter C. (2015) Sensitivity to food additives, vaso-active amines and salicylates: a review of the evidence. Clini Transl Allergy. 5-34.