Abstract
Nigeria is one of the high-burden countries in sub-Saharan Africa for HIV/AIDS and contributes to reproductive health morbidities and mortalities. This study was aimed at determining the prevalence of HIV-discordant rate among pregnant women in Plateau state Nigeria. The study sought to determine the prevalence and trend of HIV sero-discordance among pregnant women in Plateau state, Nigeria. The study was a 5-year descriptive analysis of HIV sero-discordance among pregnant women accessing prenatal care and their partners in Plateau state, Nigeria based on data generated between January 2012 and December 2016. The data was disaggregated by year, HIV concordant negative, HIV concordant positive, and HIV sero-discordant prevalence in the software and analysis were done using excel to obtained the proportions and trend of HIV sero-discordant prevalence among the antenatal population. Out of a total of 7,851 partners of pregnant women studied, 969 (16.3%) were HIV sero-discordant, 5,795 (73.8%) were HIV concordant negative, and 773 (9.9%) were HIV concordant positive. HIV sero-discordant positive males accounted for 12.3% while females were 4.0%. The prevalence of HIV sero-discordance was low with a high proportion of HIV positive male partners in Plateau state with grave public health implications for new HIV infections among partners and eroding the gains made in the Prevention of mother-to-child transmission of HIV.
Author Contributions
Academic Editor: Dr Shivaji Kashinath Jadhav, Mapmygenome India Limited, Hyderabad Previous experience, Sandor Life Sciences Pvt Ltd/ NIMR, Indian Council of Medical Research, Goa, NIRRH ICMR Mumbai, India.
Checked for plagiarism: Yes
Review by: Single-blind
Copyright © 2018 Magaji FA, et al.
 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Competing interests
The authors have declared that no competing interests exist.
Citation:
Introduction
West and Central Africa had approximately 6.5 million people living with HIV in 2015 and women accounted for nearly 60%. In the same year, the region recorded 410,000 new HIV infections and 330,000 people died of AIDS-related causes.1 Nigeria is second to South Africa with the highest burden of HIV globally and in 2014, the country was home to 3,391,546 people living with HIV and recorded 227,518 new HIV infections with males contributing 103,917 and females 123,601 new HIV infections. In the same year, the number of deaths from AIDS-related causes was put at 174,253 in Nigeria.2
The ambitious goal of the global community to end AIDS epidemic as a public health threat by 2030 will be feasible only when a reduction in HIV transmission through 90-90-90 is matched to a much more robust reduction in the risk of HIV acquisition.3,4
It is reported that sub-Saharan Africa (SSA) has the highest prevalence and incidence of HIV infection globally, mostly from heterosexual transmission.5,6The prevalence of HIV among HIV sero-discordant heterosexual couples is high in most SSA countries,7,8 and although the contribution to the spread of HIV by key populations is significant, heterosexual sex, particularly of the low-risk type still makes up about 2% in Rwanda, 13% in Zambia and Lesotho, and in Nigeria 80% of new HIV infections.9,10,11,12 In a study conducted in Nigeria on the mode of HIV transmission in 2008, two-fifths of new HIV infections occurred in the general population, among persons who are not engaging in high-risk sex that includes cohabiting or married sexual partners considered as low-risk population.2
In HIV discordant heterosexual couples in Africa, Men are generally regarded as the source of HIV in the relationship, and are referred to as “index case”.13,14 However, in most studies of sero-discordant relationships, half of the index cases are male and half are female. In a cohort study involving 13,061 sero-discordant couples in SSA and DHS involving 1,145 sero-discordant couples in 14 countries, the proportion of HIV positive women in stable heterosexual sero-discordant relationships was 47%.15
In view of the emerging role of concurrent relationships in fuelling the HIV epidemic,16, 17,18 HIV sero-discordance is now recognized as a priority for HIV prevention activities, as it can influence transmission of infection not only within adults but between mother and child and the development of antiretroviral drug resistance.19,20 Despite growing evidence of its importance; the concept of “sero-discordance” and the frequency of its occurrence are poorly understood by HIV stakeholders in our settings, resulting in the insufficient emphasis on necessary treatment strategies that can protect the negative partner and improve the life of the positive clients. There are few studies on the burden of HIV sero-discordance among cohabiting partners in Plateau state, this study sought to determine the prevalence and pattern of HIV sero-discordance among pregnant women and their partners in Plateau state.
Materials and Methods
The study was conducted in Plateau State, North-Central zone of Nigeria located between latitude 80 024’ N and longitude 80 0 32’ and 100 0 38’ East. The state is bounded in the North-East by Bauchi state, North-West by Kaduna state, South-East by Taraba state and to the South-West by Nasarawa state. It has an Area of 26,899 square kilometers and administratively divided into 17 Local Government Areas (LGAs). The population of the state from 2006 census was 1,598, 998 males and 1,607,533 females, and a total of 3,206,531. With an annual growth rate of about 2.7%, the projected population in the state was approximately 4,185,427 people as of the year 2016.
This was a 5-year descriptive study of HIV sero-discordance among pregnant women accessing prenatal care and their partners in Plateau state, Nigeria between January 2012 and December 2016. Ethical approval was obtained from the ethical review committee of the Jos University Teaching Hospital (JUTH) and the authorization to use the Plateau state HIV data source was obtained from Plateau State Ministry of Health. The data were collected on a continuous basis from PEPFAR supported health facilities in all the 17 Local Government Areas of Plateau state. Pregnant women accessing prenatal care in the PEPFAR supported health facilities and their partners were included. Pregnant women accessing prenatal care in health facilities not supported by PEPFAR were excluded in the study.
The data on HIV/AIDS were managed through the electronic Nigerian National HIV/AIDS Response Information Management System (eNNRIMS) which was a web-based software. The data were captured into the PMTCT Tools (Registers) and referred to as source document and the tools included; PMTCT Register and monthly summary form in hardcopies domiciled at the health facility. The eNNRIMS was centrally coordinated with a hierarchy of privileges from the facilities, through the Local Government level, the state, and the national levels.
At the state level, monthly Monitoring & Evaluation (M & E) meetings were held with the participation of key M & E stakeholders from implementing partners (IPs), State Ministry of Health, Plateau State Agency for the Control of AIDS (PLACA) and Local Government officers. The monthly meetings were aimed at ensuring the completeness, adequacy, and accuracy of the data. Validation meetings were held quarterly to review source documents for PMTCT across facilities against the electronic data platform for correctness and appropriateness. The same validations were held on semester bases at the national level with M & E officers from IPs, Federal Ministry of Health, National Agency for the Control of AIDS (NACA) and state officers to finalize and confirm the correctness of the data across states including Plateau state. The data was retrieved from the database manually for analysis using excel. Results were presented in line graphs for the years, and Bar charts to represent the prevalence of HIV sero-discordance among pregnant women and their partners in Plateau state Nigeria.
Results
The total number of pregnant women and their partners tested and counseled for HIV was 7,851, and on the average, 73.8% were HIV sero-concordant negative, 9.9% were HIV sero-concordant positive while 16.3% were HIV sero-discordant between 2012 and 2016 in Plateau state (Table 1, Figure 1). The total HIV sero-discordant positive males were 12.3% while that of positive females were 4.0%.
Table 1. The disaggregation of Prevalence of HIV-Discordant Pattern by year of Pregnant Women in Plateau state between 2012 - 2016| Years | 2012N (%) | 2013N (%) | 2014N (%) | 2015N (%) | 2016N (%) | TotalN (%) |
| Both Negative | 460 (71.0) | 2027 (78.3) | 1194 (55.5) | 1597 (87.8) | 517 (80.0) | 5795 (73.8) |
| Discordant Male Positive | 19 (2.9) | 243 (9.4) | 591 (27.5) | 96 (5.3) | 20 (3.1) | 969 (12.3) |
| Discordant Female Positive | 52 (8.0) | 83 (3.2) | 79 (3.7) | 54 (3.0) | 46 (7.1) | 314 (4.0) |
| Both Positive | 117 (18.1) | 235 (9.1) | 286 (13.3) | 72 (3.9) | 63 (9.8) | 773 (9.9) |
| Discordant | 71 (10.9) | 326 (12.6) | 670 (31.2) | 150 (8.3) | 66 (10.2) | 1283 (16.3) |
Figure 1.Pattern of HIV sero-Discordance among Pregnant Women in Plateau state between 2012 - 2016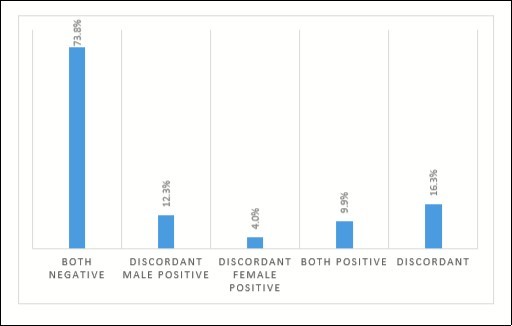
The result also showed that the highest HIV sero-discordance prevalence of 31.2% was recorded in 2014 and the least (8.3%) in 2015 (Figure 2).
Figure 2.Prevalence of HIV sero-discordant among pregnant women in Plateau state between 2012 - 2016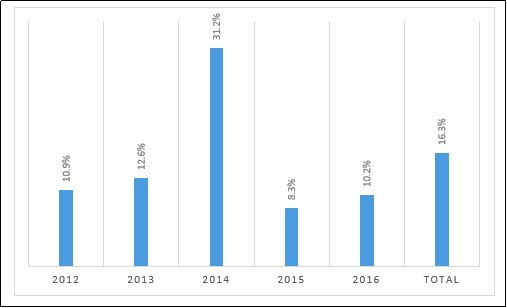
The study also showed that on the average, the proportion of HIV sero-discordant HIV positive male partners was 75.5% while that for females was 24.5% with the highest (88.2%) proportion of male HIV positive partners was recorded in 2014 (Figure 3).
Figure 3.Proportion of HIV sero-discordant by sex of partner of Pregnant Women in Plateau state between 2012 – 2016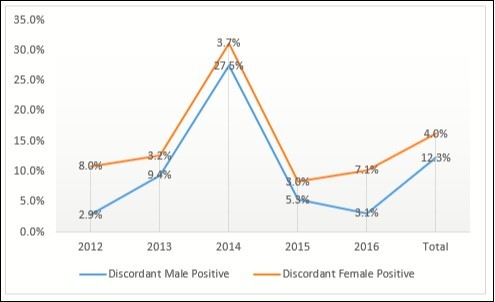
Discussion
Our study showed that on the average, the prevalence of HIV sero-discordance was 16.3%, HIV sero-concordant negative was 73.8% and HIV sero-concordant positive was 9.9% among pregnant women in Plateau state. The prevalence of HIV sero-discordant pregnant women in this study was similar to the reported prevalence of 7.7% to 78.8% in Nigeria and in other west and east African countries.21 This is however, higher than the reported prevalence of 2% in Rwanda and 13% in Zimbabwe.22 The variation in prevalence of HIV sero-discordant may be due to differences in study population and the settings as most studies are cross-sectional and hospital-based.
With regards to the pattern of HIV sero-discordance, this study has shown that there is a predominance of male HIV sero-discordance. This was however not the case in Osogbo, southwest, and Enugu, southeast Nigeria as HIV positive female partners predominate as index cases.23,24 Also, in Kenya and some other parts of sub-Saharan Africa, findings showed that female HIV positive partners predominate in HIV sero-discordant couples.25 A Tanzanian HIV and AIDS Population-Based survey showed that among couples in the current union, 93% were HIV sero-concordant negative, 2% were HIV sero-concordant positive while 5% were HIV discordant. The same survey also showed that 3% of the sero-discordant relationships had male partners as index cases, even as in most instances, similar proportions were recorded.26,27
This study also showed that 12.3% of the sero-discordant relationships had male partners as index cases, and 4.0% had females as index cases. In order words, out of the 16.3% HIV sero-discordance, we had 75.5% of the males as the positive partner while 24.5% were females. This is however not the findings in Enugu where 68.1% of females were the positive partner and 31.9% were males.24 In HIV discordant heterosexual couples in Africa and just as reported in this study, men are generally regarded as the source of HIV in the relationship, and are referred to as “index case”.28,29 However, in most studies of sero-discordant relationships, half of the index cases are male and half are female. In a cohort study involving 13,061 sero-discordant couples in sub-Saharan Africa (SSA) and Demographic Health Surveys (DHS) involving 1,145 sero-discordant couples in 14 countries, the proportion of HIV positive women in stable heterosexual HIV sero-discordant relationships was 47%.30
The proportion of HIV sero-discordance resulting from infection before couples got together versus infections introduced into the stable relationships through infidelity is unknown. However, people in HIV sero-discordant relationships, are at especially high risk of becoming infected. The yearly risk of infection for a partner of a person with HIV is about 10%,5,31 with higher annual transmission rates of 20-25% per year32,33 and up to 95% of new HIV infections in Rwanda and Zambia are in couples living together. 5,6 Living in HIV sero-discordant relationships increase the odds of HIV negative partner being infected by 8-26% yearly as compared to those who live in HIV sero-concordant negative relationships.34,35 The risk of HIV infection in HIV sero-discordant relationships increase when the regular partner is newly infected and when there is a desire to have children in which case, use of a condom during sex is limited.36,37,38
The application of the reported findings would be limited considering the fact that besides the potential for incorrect data entry by M & E officers, retrospective study gave us little opportunity to include other variables in the analysis especially that the secondary data was not disaggregated into individual subjects for multivariate logistic regression analysis of predictors for HIV sero-discordance among pregnant women. However, these findings could be used at the policy level to strengthen strategies towards achieving 90% knowledge of HIV status of partners of pregnant women in Plateau state.
Conclusion
The prevalence of HIV sero-discordant pregnant women was relatively low in Plateau state and had a higher proportion of male partners as the index cases. This has grave implications to heterosexual transmission of HIV with greater risk to the woman for HIV infection and worsening mother-to-child transmission of HIV in Plateau state Nigeria.
Acknowledgment
Research reported in this publication was supported by the Fogarty International Centre (FIC); Office of the Director (OD/NIH); National Institutes of Neurological Disorders and Stroke (NINDS/NIH); and the National Institute of Nursing Research (NINR/NIH) of the National Institutes of Health under award number D43TW010130. The content is solely the responsibility of the authors and does not necessarily represent the views of the National Institutes of Health. The authors also thank the Hon. Commissioner for Health Plateau state, the Coordinator and staff of the state HIV/AIDS and STI Control programme, the staff of Plateau state HIV/AIDS Control Agency, Civil Society Networks/NGOs on HIV/AIDS, and Implementing Partners for providing the HIV services and generating the data used in this study.
References
- 2. (2012) Nigerian National Agency for the Control of AIDS. Global AIDS Response: Country Progress Report. , GARPR, Abuja, Nigeria
- 5.Dunkle K L, Stephenson R, Karieta E, Chomba E, Kayitenkore K et al. (2008) New heterosexually transmitted HIV infections in married or cohabiting couples in urban Zambia and Rwanda: an analysis of survey and clinical data. The Lancet. 371(9631), 2183-2191.
- 6.Bellan S E, Fiorella K J, Melesse D Y, Getz W M, Williams B G et al. (2013) Extra-couple HIV transmission in sub-Saharan Africa: a mathematical modeling study of survey data. The Lancet. 381(9877), 1561-1569.
- 7.Sagay A S, Onakemhor J, Galadanci H, Emuveyan E E. (2006) HIV status of partners of HIV positive pregnant women in different regions of Nigeria: matters arising. Afr J Med Sci. , 35 Suppl: 125, 9.
- 8.Lurie M N, Williams B G, Zuma K. (2003) Who infects whom? HIV-1 concordance and discordance among migrant and non-migrant couples in South Africa. AIDS. 17, 2245-52.
- 9. (2006) . Institut National de la Statistique du Rwanda (INSR), ORC Macro. Rwanda Demographic and Health Survey2005. Calverton, MD, USA:INSR and ORL Macro; .
- 10. (2007) CSO,ORC Macro.Zimbabwe Demographic and Health Survey2005-06.Harare,Zimbabwe: Central Statistical Office, and Calverton,MD,USA:ORL Macro.
- 11. (2005) MOHSW,BOS,ORL Macro.Lesotho Demographic and Health Survey2004.Maseru, Lesotho: Ministry of Health and Social Welfare. , Bureau of Statistics, and Calverton,MD,USA:ORC Macro
- 12.Olagbuji B N, Ezeanochie M C, Agholor K N, Olagbuji Y W, Ande A B et al. (2011) Spousal disclosure of HIV serostatus among women attending antenatal care in urban Nigeria. , Journal of Obstetrics and Gynaecology 31(6), 486-488.
- 13.Serwadda D, Gray R H, Wawer M J. (1995) The social dynamics of HIV transmission as reflected through discordant couples in rural Uganda. , AIDS 9, 745-50.
- 14. (2004) UNAIDS,UNFPA and UNIFEM.Women and HIV/AIDS: Confronting the crisis. , Geneva and New-York:UNAIDS,UNFPA and UNIFEM 7, 16.
- 15.Eyawo O, D de Walque, Ford N, Gakii G, Lester R T. (2011) HIV status in discordant couples in sub-Saharan Africa: a systemic review and meta-analysis. , Lancet Infect Dis 11, 263-4.
- 16.Halperin D T, Epstein H. (2004) Concurrent sexual partnerships help to explain Africa’s high HIV prevalence: implications for prevention. , Lancet 364, 4-6.
- 17.Mah T L, Halperin D T. (2010) Concurrent sexual partnerships and the HIV epidemics in Africa: evidence to move forward. , AIDS Behav 14, 11-16.
- 19.Bunnell R, Mermin J, De Cock KM. (2006) HIV prevention for a threatened continent: implementing positive prevention in Africa. , JAMA 296, 855-58.
- 20.Malamba S S, Mermin J H, Bunnell R. (2005) Couples at risk: HIV-1 concordance and discordance among sexual partners receiving voluntary counseling and testing in Uganda. , J Acquir Immune Defic Syndr 39, 576-80.
- 21.Sagay A S, Onakewhor J, Galadanchi H, Emuveyan E E. (2006) HIV status of partners of HIV positive pregnant women in Different regions of Nigeria: matters arising. Afr J Med Sci. 35, 125-129.
- 22.Dunkle K L, Stephenson R, Karita E, Chomba E, Kayitenkore K. (2008) New heterosexually transmitted HIV infections in married or cohabiting couples in urban Zambia and Rwanda: an analysis of survey and clinical data. , Lancet 371, 2183-2191.
- 23.Kola M O, Adetunji O A, Adewale S A, Adeleye A A, Adeola F A. (2015) . HIV sero-discordance: Prevalence and Pattern at LAUTECH Teaching Hospital Osogbo, Southwest Nigeria. Int J Med and Pharm Sci 5(1), 25-34.
- 24.Okafor Asimadu EE, Okenwa W O. (2015) Prevalence of couple Human Immunodeficiency Virus (HIV) Discordance. and Prevention of New HIV Infection in the Negative Partner in Enugu, southeast Nigeria. Gynecol obstet 5(11), 337.
- 25.Desgrees du L, Annablel. (2008) Couple-centered testing and counseling for HIV sero-discordant heterosexual couples in sub-Saharan Africa. Reproductive Health matters. 16(32), 151-61.
- 26.Eyawo O, D de Walque, Ford N, Gakii G, Lester R T et al. (2010) HIV status in discordant couples in sub-Saharan Africa: a systematic review and meta-analysis. The Lancet Infectious diseases. 10(11), 770-7.
- 27.Kaiser R, Bunnell R, Hightower A. (2011) Factors associated with HIV infection in married or cohabiting couples in Kenya: results from a nationally representative study. , PLoS One 6(3), 17842.
- 28.Serwadda D, Gray R H, Wawer M J. (1995) The social dynamics of HIV transmission as reflected through discordant couples in rural Uganda. , AIDS 9, 745-50.
- 29. (2004) UNAIDS,UNFPA and UNIFEM.Women and HIV/AIDS: Confronting the crisis. , Geneva and New-York:UNAIDS,UNFPA and UNIFEM: 7, 16.
- 30.Eyawo O, D de Walque, Ford N, Gakii G, Lester R T. (2011) HIV status in discordant couples in sub-Saharan Africa: a systemic review and meta-analysis. , Lancet Infect Dis 11, 263-4.
- 31.Hugonnet S, Mosha F, Todd J. (2002) Incidence of HIV infection in stable sexual partnerships: a retrospective cohort study of 1802 couples in Mwanza Region. , Tanzania, J Acquir Immune Defic Syndr 30, 73-80.
- 32.Guthrie B L, G de Bruyn, Farquhar C. (2007) HIV-1-discordant couples in sub-Saharan Africa: explanations and implications for high rates of discordancy. , Curr HIV Res 5, 416-429.
- 33.Hira S K, Nkowane B M, Kamanga J, Wadhawan D, Kavindele D. (1990) Epidemiology of human immunodeficiency virus in families in. , Lusaka, Zambia, J Acquir Immune Defic Syndr 3, 83-86.
- 34.Glynn J R, Carael M, Musonda R M, Kahindo M. (2003) HIV risk in relation to marriage in areas with high prevalence of HIV infection.(1999)Journal of Acquired immune deficiency syndromes. 33(4), 526-35.
- 35.Kapiga S H, Sam N E, S Mlay J Aboud, Ballard R C, Shao J F. (2006) The epidemiology of HIV-1 infection in Northern Tanzania: results from a community-based study. AIDS Care. 18(4), 379-87.
- 36.DeWalque D. (2007) Sero-discordant couples in five African countries: Implications for prevention strategies. Population and Development Review 33(3):. 501-22.
