Abstract
Cutaneous ciliated cyst is cogitated as a benign, exceptional lesion and can be additionally termed as cutaneous Mullerian cyst or a cystadenoma. Cutaneous ciliated cyst was initially described by Da Hess in 1890 and further elucidated in 1978 by Farmer and Helwig as a cyst predominantly occurring in young females within the second and third decades of life 1, 2. Cutaneous ciliated cyst is a lesion of post- pubertal females, can appear in the reproductive phase and frequently enlarges during menstruation or pregnancy due to hormonal effects. Cutaneous ciliated cyst is commonly situated within deep-seated dermal or subcutaneous tissue of the upper extremities and perianal region. Cutaneous ciliated cyst delineates as Mullerian derivation in females and a distinct, foetal eccrine duct origin in males 1, 2.
Author Contributions
Academic Editor: Pietro Scicchitano, Cardiology Department, Hospital of Ostuni (BR) - Italy.
Checked for plagiarism: Yes
Review by: Single-blind
Copyright © 2019 Anubha Bajaj
 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Competing interests
The authors have declared that no competing interests exist.
Citation:
Preface
Cutaneous ciliated cyst is cogitated as a benign, exceptional lesion and can be additionally termed as cutaneous Mullerian cyst or a cystadenoma. Cutaneous ciliated cyst was initially described by Da Hess in 1890 and further elucidated in 1978 by Farmer and Helwig as a cyst predominantly occurring in young females within the second and third decades of life 1, 2.
Cutaneous ciliated cyst is a lesion of post- pubertal females, can appear in the reproductive phase and frequently enlarges during menstruation or pregnancy due to hormonal effects. Cutaneous ciliated cyst is commonly situated within deep-seated dermal or subcutaneous tissue of the upper extremities and perianal region. Cutaneous ciliated cyst delineates as Mullerian derivation in females and a distinct, foetal eccrine duct origin in males 1, 2.
Disease Characteristics
Cutaneous ciliated cyst classically enunciates as a painless benign nodule on the lower extremities of adolescent girls. Additionally scalp, scapula, thumb, abdomen, umbilicus, perineum, thigh, neck, ankle, knee, inter-scapular, lumbar, inguinal and gluteal region are sites which delineate cutaneous ciliated cyst. Males are also implicated. Aberrant locations such as fingers, cheek, scrotum, shoulders and mediastinum can be incriminated 2, 3.
Cutaneous ciliated cyst can be designated into two subgroups as Mullerian cysts and ii) cutaneous ciliated eccrine cysts. Cutaneous ciliated cysts demonstrating an immune reactivity to oestrogen receptors (ER) and progesterone receptors (PR) are essentially cogitated as cutaneous Mullerian cysts whereas immune non reactive cysts to aforesaid biomarkers are designated as cutaneous ciliated eccrine cysts 4.
Disease Pathogenesis
Cutaneous ciliated cyst is a condition of obscure aetiology. Various theories have been propounded. Theories are contemplated as Mullerian heterotopia, metaplasia of sweat glands and cysts engendered from embryonic remnants.
a) An ectopic reserve of Mullerian tissue recapitulates the epithelium lining fallopian tubes and evolves on account of hormonal stimulation following puberty. Majority of functional, circumscribing epithelial cell rests depict Mullerian heterotrophy. The fallopian tubes emerge within embryologic phase from the remnants of paramesonephric duct in the sixth or seventh week of gestation. Aforesaid hypertrophied Mullerian cells can migrate to the lumbar region, anterior abdominal wall, lower extremities, scalp, fingers, heels and knees during sixth or seventh week of antenatal period. Mullerian cell rests can enlarge and configure a cyst secondary to pubertal hormonal stimulation4, 5.
Hypothesis of heterotopic Mullerian epithelium origin defines sequestration of the Mullerian cell rests which occurs during the early phase of embryogenesis within sixth and seventh week of gestation. As the Mullerian rests are adjacent to Mullerian canal, aforesaid rests are elucidated within the pelvis, perineum, abdominal wall, deep- seated dermis and subcutaneous tissue of the lower extremities. Hormone responsive Mullerian cell rests configure identical Mullerian cysts contingent to enhanced hormone production following puberty or during pregnancy.
b) Cutaneous ciliated cysts are frequent in the pubescent females with a distinctive occurrence, are immune reactive to oestrogen receptors, progesterone receptor and display variable reactivity to carcino-embryonic antigen (CEA). Aforesaid manifestations support the hypothesis of Mullerian heterotrophy. Nevertheless, cutaneous cilated cyst can be observed on the cheek, scrotum and shoulders of male subjects. Heterotopic Mullerian epithelium secretes serous fluid during the pubertal phase and can engender a cutaneous ciliated cyst on account of hormonal factors 4, 5.
c) An alternative theory propounds the premise of ciliated metaplasia of the eccrine gland. According to the theory of ciliated metaplasia of eccrine glands , foetal eccrine ducts are essentially layered with ciliated epithelium, thus generation of cilia can ensue in concordance with eccrine differentiation of cutaneous cyst. Aforesaid theory adequately propounds the pathogenesis of cutaneous ciliated cyst in males and within anomalous locations.
Cutaneous ciliated cysts at aberrant sites and cysts in males can represent metaplastic alterations of a pre- existent simple cyst with a lining derived from a sweat duct. Alternatively, an entirely diverse histogenesis can be implicated4, 5.
d) Leonforte in 1982 examined the cutaneous ciliated cyst for simulating sweat glands and described two specific features of apocrine sweat glands as identified in aforesaid ciliated cysts. The specific attributes are cogitated as the appearance of granules stained with periodic acid Schiff’s (PAS) stain and the emergence of epithelial apical caps.
The specified epithelial modifications recapitulate normal fallopian tube on account of metaplastic alterations secondary to chronic irritation of the pleuri-potent cells 3.
e) Cutaneous ciliated cyst of the perineum designates cyst origin from the embryonic remnants of cloacal membrane, especially segments arising from the primitive caudal gut.
Irrespective of alternative theories, Mullerian heterotopia theory remains a cogent alternative on account of morphological similarities of fallopian tube epithelium and nuclear immune reactivity to hormone receptors such as oestrogen receptor and progesterone receptors.
Theory of heterotopia or heterotopic origin of ciliated epithelium arising from Mullerian epithelium is considered as a precise hypothesis.
Cutaneous ciliated cysts can be observed in diverse regions on account of vascular and lymphatic distribution of engendering epithelium4, 5.
Clinical Elucidation
Cutaneous ciliated cyst commonly delineates as an asymptomatic, solitary, cystic to soft, fluctuant, non-inflamed, gradually evolving, mobile, painless nodule with an unremarkable cutaneous covering and variable dimension at the aforementioned sites. Pre-sacral region can depict a tender, soft, solitary mass a few centimetres in diameter, which can reoccur following aspiration. Cutaneous ciliated cyst appears in the deep dermal or subcutaneous tissue. Cutaneous ciliated cyst is devoid of adherence to adjacent muscle or tendons. The cyst is preponderant in females within the age group of 12 years to 42 years. Commonly, the order of disease incrimination with cutaneous ciliated cyst is thigh, buttock, calf and foot 6, 7.
Histological Elucidation
Typically, cutaneous ciliated cyst is a simple cyst which demonstrates a layering of pseudostratified ciliated columnar epithelium recapitulating conventional epithelial lining of the fallopian tube. As the cutaneous ciliated cyst demonstrates a morphological similarity to the fallopian tube lining epithelium, a Mullerian origin is indicated. Gross examination of cutaneous ciliated cyst depicts a solitary, mobile, non-tender, fluctuant, firm or soft to cystic lump with a fibrous wall and abundant amount of circumscribing adipose tissue. Cutaneous ciliated cysts are of a variable dimension. Cut surface usually displays a unilocular cyst impacted with clear, serous fluid, an attenuated smooth, greyish/ white cyst wall incorporated with incomplete septa traversing the cyst 6, 7.
Morphological analysis preponderantly demonstrates a solitary, uni-locular or multi-locular cyst of Mullerian origin with an epithelial lining recapitulating the epithelium of fallopian tube.
Cutaneous ciliated cyst is layered with a singular layer of ciliated epithelial cells which are chiefly constituted by cuboidal to columnar epithelium, traversed by partially configured fibrous tissue septa with an admixture of randomly dispersed, intraluminal papillary projections akin to those cogitated in the fallopian tube. Superimposed epithelium is inundated with well vascularized, parallel bundles of collagen although smooth muscle is absent 7, 8.
Cystic structures cogitated within deep dermal or subcutaneous tissue can be impacted with haemorrhagic fluid. Cyst lining is smooth, regular and is essentially composed of a singular layer of columnar epithelium with focally pseudostratified columnar epithelium, a circumscription of loosely configured, well vascularized, fibroconnective or fibrocollagenous tissue and an absence of inflammatory infiltrate.
Alternatively, cutaneous ciliated cyst can be lined by non ciliated cuboidal or columnar epithelium with intermingled intercalated, dark or round peg cells. Foci of squamous metaplasia can be occasionally exemplified in the adherent epithelium whereas mucinous cells or apocrine-like features are exceptional 6, 8. Figure 1, Figure 2, Figure 3, Figure 4, Figure 5, Figure 6, Figure 7, Figure 8, Figure 9, Figure 10, Figure 11, Figure 12. 11, 12, 13, 14, 15, 16, 17, 18, 19.
Figure 1.Ciliated cutaneous cyst lined by pseudostratified ciliated columnar epithelium and a supporting fibro-connective tissue stroma 11.
Figure 2.Ciliated cutaneous cyst with an undulating layer of ciliated cuboidal epithelium and supporting fibrous tissue framework (12).
Figure 3.Ciliated cutaneous cyst with a coating of plump, ciliated columnar epithelium and a circumscribing fibro - connective tissue (12).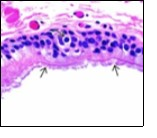
Figure 4.Cutaneous ciliated cyst with a ciliated, pseudostratified columnar epithelium and vascularized fibrous tissue stroma (13).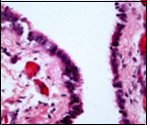
Figure 5.Cutaneous ciliated cyst with incomplete intervening septa and a lining of attenuated, ciliated epithelium along with supporting fibrous tissue (13).
Figure 6.Cutaneous ciliated cyst with a ciliated cuboidal lining, undulations within the cyst cavity and a wall comprised of fibro-connective tissue (14).
Figure 7.Cutaneous ciliated cyst with papillary structures, a coating of ciliated columnar epithelium supported by a connective tissue framework (15).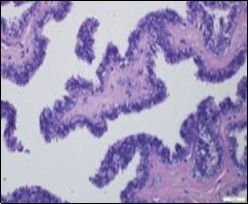
Figure 8.Cutaneous ciliated cyst with incomplete septa and a layer of pseudostratified, ciliated columnar epithelium surrounded by fibrous tissue (16).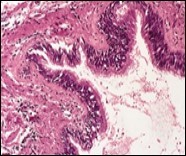
Figure 9.Cutaneous ciliated cyst with abundant, circumscribing fibro-connective tissue and a cyst lined by ciliated columnar epithelium (17).
Figure 10.Cutaneous ciliated cyst with nuclear immune reactivity to progesterone receptors (18).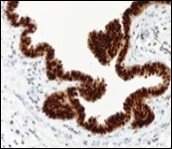
Figure 11.Cutaneous ciliated cyst with immune reactivity to cyto-keratin (19).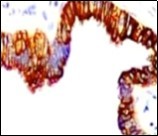
Figure 12.Cutaneous ciliated cyst with nuclear immune reactivity to oestrogen receptors (19).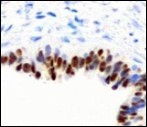
Immune Histochemical Elucidation
Epithelium of cutaneous ciliated cyst is immune reactive for pan cytokeratin (CKae1/ae3) antigens, epithelial membrane antigen (EMA), oestrogen receptors (ER), progesterone receptors (PR), Wilm’s tumour protein (WT-1) and paired box gene 8 (PAX8). Immune non reactivity is cogitated for S100, smooth muscle actin (SMA), carcino-embryonic antigen (CEA), desmin, thyroid transcription factor(TTF1), p63 and glial fibrillary acidic protein (GFAP).
Smooth muscle actin (SMA) is immune non reactive, thereby suggesting an absence of smooth muscle within the cyst wall. Intense immune reactivity can be cogitated within epithelial nuclei for oestrogen receptors (ER) and progesterone receptors (PR). Aforesaid immune reactions are indicative of Mullerian origin of cutaneous ciliated cyst.
Focal epithelial staining for periodic acid Schiff’s(PAS) stain is enunciated 4, 5. Pan cytokeratin (CKae1/ae3) are diffusely immune reactive.
Cutaneous ciliated cyst demonstrates immune reactivity to Dyein, akin to the reaction elicited in normal fallopian epithelium. Nevertheless, atypical locations of cutaneous ciliated cyst or those arising in males are immune non- reactive with oestrogen receptors (ER) and progesterone receptors (PR) on account of enunciated eccrine glandular epithelium. However, particular instances are immune reactive with carcinoembryonic antigen (CEA), p63, S100 and gross cystic fluid disease protein (GCFDP-15) 8, 9.
Ultrastructural examination displays cilia with a characteristic morphology exemplifying a centric pair of micro tubules, nine radially oriented pairs of micro tubules, basal bodies and cross striated rootlets.
Differential Diagnosis
Cutaneous ciliated cysts necessitate a demarcation from conditions such as inclusion cysts, dermoid cysts, lipomas, adnexal cysts, thymic cysts, bronchogenic cysts, meningocoele, myelomeningocoele, abscesses or pilonidal cysts. Additionally, cutaneous ciliated cyst requires a segregation from branchial cleft cyst, mature cystic teratoma or thyroglossal duct cysts. Infrequently chondroma, sweat gland tumours, metastatic masses, giant cell tumours and neurofibromas can require a demarcation4, 5.
Cutaneous ciliated cyst demonstrates specific features such as absence of mucous glands, appearance of cysts on the lower extremities, nuclear immune reactivity for oestrogen receptors (ER) and progesterone receptors (PR) and non reactivity for carcinoembryonic antigen (CEA). Myelomeningocoele and meningocoele, can be segregated from cutaneous ciliated cyst by analysing cyst fluid and employing imaging technologies revealing a blind cutaneous ciliated cyst which is immune non reactive for glial fibrillary acidic protein (GFAP).
A pilonidal cyst can demonstrate typical drainage of purulent material. Monodermal teratoma can display a focus of ciliated respiratory epithelium. Immune reactivity for TTF-1 can be employed for differentiation 9, 10.
Investigative Assay
Ultrasound usually depicts a well defined, subcutaneous, painless, lobulated, hyper-intense cyst or nodule with a uniform outline, a regular, smooth contour, fine internal septa traversing the cyst and minimal quantities of fluid. The cyst can be devoid of calcification or enhanced vascularity.
Therapeutic Options
Optimal therapy for managing a cutaneous ciliated cyst is comprehensive surgical excision of the cyst. Cogent surgical eradication and appropriate immune- histochemical evaluation of cyst are crucial in arriving at an appropriate conclusion. Competent surgical eradication is followed by an absence of cyst reoccurrence 9, 10.
References
- 1.Butterworth S, Stewart M. (1970) Heterotopic ciliated epithelium- Mullerian origin? Lancet. 1, 1400-1401.
- 4.Anbarserry I. (2018) Alhamar M et al” Cutaneous ciliated cyst”. , Bahrain Medical Bulletin 40(4), 240-241.
- 5.Gun Seda, Kuru Duygu. (2018) A cutaneous ciliated cyst mimicking a pilonidal cyst”. , Journal of Clinical and Diagnostic Research 12(10), 06-08.
- 6. (2018) Cutaneous ciliated cyst in an unusual location: between two scapulas” Case Reports in Surgery. 1-3.
- 7.Fabian- Dupuis C, Cooper B. (2016) Mullerian type ciliated cyst of the thigh with PAX-8 and WT-1 positivity : a case report and review of literature “ Case reports in Medicine. 1-5.
- 8.Joehlin- Price AS, Huang J H. (2014) PAX-8 expression in cutaneous ciliated cyst : evidence for mullerian origin”. , Am J Dermatopathol 36(2), 167-70.
- 9.Kim Y, Kim H. (2015) The cutaneous ciliated cyst in young male: the possibility of ciliated cutaneous eccrine cyst “ Case Rep Med:. 589831.
