Abstract
Purpose
Is it safe to excise only the external portion of the pacemaker wires? This presentation aims to find out the proper way to manage pacing wires postoperatively.
Methods
We report 5-cases of sub-xiphoid abscesses and sinuses after valve surgery. Each case presented with a recurrent abscess that opens and drains its contents through a sinus around the lower-most portion of the xiphoid process. The duration between open heart surgery and evolution of these abscesses varied between 18 and 60 months. Valve surgeries were mitral and/or aortic valve replacement. Surgeons usually insert pacemaker wires to control any persistent post-operative arrhythmias that can affect hemodynamic circulation. On the day of discharge, some surgeons (not in our center) usually excise the pacemaker wires.
Results
The remaining intra-thoracic portions underwent some degree of corrosion that caused a state of chronic inflammation, sinus track formation and abscess evolution. This indicated radiological examination and surgical exploration to extract these foreign bodies. These 5 cases were diagnosed and operated upon between 15th January 2022 and 1st March2022, all at Abo-Khalifa Emergency Hospital-Ismailia, Egypt.
Conclusions
This confirms the significance of total withdrawal of the external pacemaker wires. Surgeons should not apply tight sutures at the site of insertion of the wires.
Author Contributions
Academic Editor: ANUBHA BAJAJ, Consultant Histopathology, A.B. Diagnostics, New Delhi, India.
Checked for plagiarism: Yes
Review by: Single-blind
Copyright © 2022 Hamdy Dosoky Elayouty, et al.
 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Competing interests
The authors have declared that no competing interests exist.
Citation:
Introduction
Temporary pacemaker wires (leads) are usually inserted in patients after valve replacement. These may be beneficial for optimizing myocardial function in patients that develop postoperative hemodynamically-significant arrhythmias 1.
Pacemaker wires have two ends - one end has a small needle, which is passed into the epicardial surface, then it`s cut off. The needles may be coiled or clipped for better fixation. On the other end, the larger needle is used to penetrate the body wall, to pass the wire through to the body surface. The most common site of insertion is into the epicardial surface of the right ventricle 2. The complications of extraction of pace maker wires include: bleeding, tamponade, arrhythmias, and even retention with its serious hazards. During removal of wires, there may be atrial or ventricular lacerations which lead to bleeding and to developing tamponade. This may prolong the hospital stay of patients, especially patients on anticoagulant medications 5.
Case Description
We are reporting 5 cases. These 5 cases were diagnosed and operated upon during the last two months at AboKhalifa Emergency Hospital, Ismailia, Egypt.
After weaning from cardiopulmonary bypass, as per institutional protocol for heart-valve operations, right atrial and /or right ventricular epicardial and diaphragmatic pacing wires (Quad Polar, 250 cm, Medical Concepts Europe (MCE), MCE Gemert, Netherlands) were inserted. Atrial wires were fixed with 5/0 prolene sutures taking superficial bites on the surface of the epicardial surface layer just to ensure gentle contact with the heart muscles and minimize complication rate 3, 5. The exit site in the epigastrium to the right of the midline was secured with a 2/0 silk suture. After an uneventful recovery in intensive care, each patient was transferred to the ward. As per institutional protocol, all postoperative cardiac surgical patients receive low molecular weight heparin subcutaneously as a prophylaxis against deep vein thrombosis The DVT-prophylaxis is continued until the day of discharge or when the patient is fully ambulatory. We do not stop the prophylaxis before temporary Pacemaker Wire-removal. On the 4th postoperative day, the pacing wires were pulled out with gentle traction. In centers other than ours, some surgeons only excise the external portion of the wires. This was complicated with chronic abscess and sinus formation years after surgery (Table 1). Diagnosis was confirmed radio-logically (Figure 1).
Table 1. Patient characteristics| PatientNo. | Age | Sex | Type of surgery | Duration in-between | No. of extracted wires |
| 1 | 32 Y. | M. | Aortic and mitral replacement | 18 months | 2 |
| 2 | 38 Y. | F. | Aortic replace.. | 2 Y | 1 |
| 3 | 46 Y. | F/ | Mitral and tricuspid repair | 4 Y | 2 |
| 4 | 42 Y | M. | CABG and mitral replacement | 5Y. | 2 |
| 5 | 52Y. | F. | Aortic replace. | 2 Y. | 1 |
Figure 1.Sagittal CT-section of chest showing the extension of the sinus track containing the contrast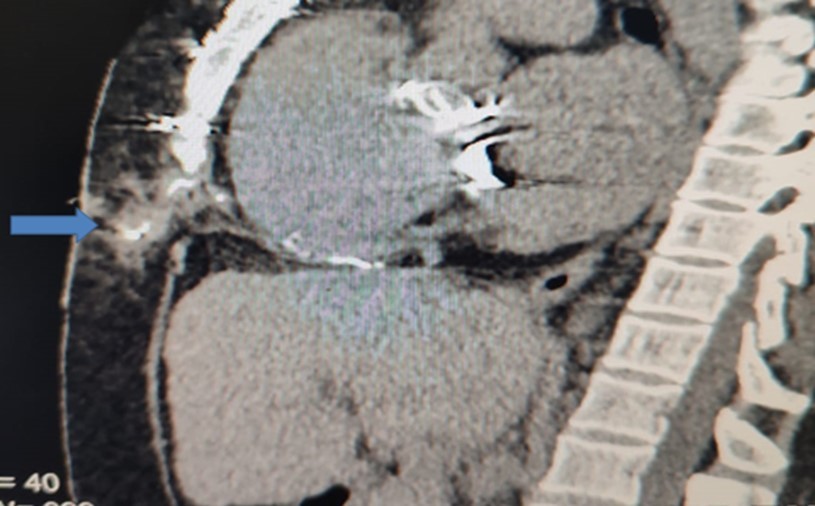
Discussion
All pacemaker leads make use of a coil for current transfer that is made of a metal alloy. This alloy consists of chromium cobalt, nickel and chromium. The conductive coil is not in direct contact with the patient tissues. Significant corrosion was reported to affect all pacemaker-electrodes. Corrosion is directly related to the duration of implantation4, 5, 6. The above-mentioned metals are not corrosion proof but they are susceptible to slow degeneration. Corrosion occurs when most or all of the atoms of the metal surface are oxidized; they tend to lose electrons to oxygen in the air or water. A low grade-chronic infection plays a role 7, 8. This explains the appearance of the sinus tracks and abscesses years after open heart surgery & insertion of pacemaker-electrodes (Table 1).
Temporary pacing is undertaken to treat dysrhythmias and to improve hemodynamics. Replacing the aortic or the mitral valve can be followed by edema and compression with or without damage of the conduction system and necessitate the implantation of a temporary and /or permanent pacemaker.
Steps of the Procedure
a) Adjustment of the bleeding profile, stoppage of oral anticoagulant and replace it by parenteral one.
b) Computerized tomography with mild push of contrast to the sinus track (Figure 1)
c) Under general anesthesia with the patient in the supine position, and after sterilization and draping , we inject methylene blue into the track
d) Excision of the track we usually find the offending wire(s) at the base of the track (Figure 2)
e) Mild and slow traction on each wire to extract it. No undue force was required and the pacing wires came out easily
f) Echocardiography was done after closure of the wound in layers.
Figure 2.One of the offending pacing wires found adjacent to back of the xyphoid process. It is held with forceps.
Conclusions
These cases demonstrated the necessary extraction of the whole length of the external pacemaker-wires. Surgeons can apply tight sutures at the site of insertion of pacing wires to make their withdrawal safe and easy.
Ethical Considerations
The study protocol was approved by the research ethics committee of the Faculty of Medicine, Suez Canal University, in Ismailia, Egypt
An informed consent for carrying out special investigations was taken from patients undergoing this study. This consent contained:
a) Explanation of aim, procedure, and potential benefits of the study in a simple way easy to understand.
b) No harmful maneuver will be used, potential risks will be minimized by performing the procedure by our team.
c) All data will be considered confidential and will not be used outside this study without patient approval.
d) Researcher phone number and all communicating methods will be identified to patients.
e) Patients will be announced by results of study.
f) Patient has the right to withdraw from this study at any time without affecting their routine medical care.
g) Signature or finger prints of patients.
References
- 1.Russell S J, Tan C, O'Keefe P, Ashraf S, Zaidi A et al. (2012) Temporary epicardial cardiac re-synchronisation versus conventional right ventricular pacing after cardiac surgery: study protocol for a randomized control trial. 13-20.
- 2.Reade M C. (2007) Temporary epicardial pacing after cardiac surgery: a practical review: part 1: general considerations in the management of epicardial pacing Anaesthesia. 62, 264-71.
- 3.Aser R, Orhan C, Niemann B, Roth P, Perepelitsa A et al. (2014) Temporary epicardial pacemaker wires: significance of position and electrode type. Thorac Cardiovasc Surg. 62, 66-9.
- 4.Medina R, Michelson E L. (1985) Update on cardiac pacemakers: description, Complications, indications, and followup. Cardiovasc Clin. 16, 177-213.
- 5.Viktorsson S A, Orrason A W, Vidisson K O, Gunnarsdottir A G, Johnsen A et al. (2020) Gudbjartsson T: Immediate and long-term need for permanent cardiac pacing following aortic valve replacement. Scand Cardiovasc J. 54, 186-191.
