Abstract
To demonstrate that percutaneous coronary intervention (PCI) may in some cases be a safe option for patients with a high-risk surgical category, we report a complex clinical case of revascularization of multivessel coronary artery disease including left main coronary artery (LMCA) quadrifurcation.
Methods
For safety reasons, PCI was done in 2 separate sessions (staged PCI). Stenting of the LMCA quadrifurcation was performed using different stenting techniques in combination: modified balloon mini crush stenting technique was used - for LMCA and intermediate artery (IMA) stenting; modified balloon crush stenting technique was used for LMCA, circumflex artery (CX) and first obtuse marginal branch (OM1) stenting; provisional stenting technique was used for CX stenting, followed by sequential kissing balloon post-dilatation technique between LMCA and every branch; proximal optimization technique (POT) was performed in the LMCA. Left anterior descending artery (LAD), intermediate artery, circumflex artery, first obtuse marginal branch, left main coronary artery and its quadrifurcation were stented with 5 drug-eluting stents (DES) (Resolute Integrity, Medtronic); right coronary artery (RCA) was stented with 3 bare-metal stents (BMS) (Rebel, Boston Scientific).
Results
The interventions ended without complications, the ejection fraction increased from 35% to 48%, congestive heart failure functional class decreased to class I. Subsequent coronary angiography, eight months after the last PCI, revealed patent stents with mild, nonsignificant restenosis. More than three years after the intervention, the patient has no complaints (according to MACE).
Conclusions
It should be considered that in case of the selection of suitable patients and the use of the appropriate revascularization technique, LMCA quadrifurcation lesion can be successfully treated with PCI.
Author Contributions
Academic Editor: Leibundgut G, Universitaets-Herzzentrum Freiburg Bad Krozingen, Germany.
Checked for plagiarism: Yes
Review by: Single-blind
Copyright © 2020 Murman Kantaria, et al.
 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Competing interests
The authors have declared that no competing interests exist.
Citation:
Introduction
It has been estimated that left main coronary artery (LMCA) quadrifurcation encountered in 5.6% of the human population 3, 4, 5 is a very rare finding on coronary angiography (CAG). Due to the anatomical complexity, the atherosclerotic lesion of the LMCA quadrifurcation makes percutaneous coronary intervention (PCI) difficult, although not impossible. Only single PCI reports for LMCA quadrifurcation are available. Coronary artery bypass grafting (CABG) seems to be the gold standard for such lesion treatment, but sometimes PCI is the only option for revascularization, especially for high-risk patients 2.
To demonstrate that PCI may in some cases be a safe option for patients with a high-risk surgical category, we report a complex clinical case of revascularization of multivessel coronary artery disease including LMCA quadrifurcation.
Methods
Stenting Technique
Modified balloon crush stenting technique: after pre-dilatation of the main branch (MB) and side branch (SB), the stent is placed in the SB so that part of the SB stent protrudes in the MB, after that the balloon catheter is loaded in the MB, After deployment of the SB stent, and removal of its balloon and wire, it is crushed by the inflated MB balloon, The SB ostium is re-opened by balloon inflation. The stent is implanted in the MB; the procedure is completed with final kissing balloon inflation. Mini-Crush stenting technique is like the modified balloon crush technique, it differs only by a minor retraction of the side branch stent into the main branch. Provisional stenting technique consists of stenting the MB with the option to rewire the SB, to perform kissing balloon inflation and if necessary to place a stent in the SB 1.
Patient
The study was performed on the 83-year-old male patient with severe multivessel coronary artery disease, including LMCA quadrifurcation, 38 years history of diabetes type II, arterial hypertension (T/A max 200/110 mmHg), amputated right leg (8 years ago), congestive heart failure of functional class II-III (NYHA), periodically developing dyspnea and retrosternal chest pain, hydrothorax, peripheral edema, frequent hospitalizations.
CAG, performed in 2011, revealed multi-vessel coronary artery disease; the patient was assessed as a high-risk patient, denied both to perform the intervention (stenting) as well as CABG, only medication treatment was recommended. With time patient’s symptoms worsened, finally, the patient complained retrosternal chest pain at rest or with minimal exertion.
In March 2016, a patient was hospitalized due to severe chest pain. The patient underwent the Lab tests, electrocardiography (ECG), ultrasonography examination and CAG performed, the SYNTAX score was calculated.
Results and Discussion
Ultrasound examination of the patient were revealed: cardiac ejection fraction (CEF) - 35% (versus 55% or more in control), left ventricular apical hypokinesis, hypokinesis of mid and basal segments of the anterolateral wall, diastolic dysfunction type I, moderate aortic valve stenosis and mild regurgitation, mean gradient – 32 mmHg, moderate mitral and mild tricuspid valves regurgitation, systolic pulmonary artery pressure (PAPs) – 61 mmHg. ECG findings were in normal range.
Angiography revealed rare anatomical variation LMCA quadrifurcation (Figure 1, Figure 2), 50% stenosis of the distal part of the LMCA, 40% stenosis of the ostial segment of left anterior descending (LAD) artery and diffuse prolonged 70-75-95% stenosis in mid-segment (Figure 3), 75% stenosis of the ostial segment of the circumflex (CX) artery, 75% stenosis of the ostial segment of the first marginal branch (OM1), 75-90% stenosis of the proximal segment of the intermediate artery (IMA), prolonged diffuse severe 90-95% stenosis of mid-segment of the right coronary artery (RCA) (Figure 4).
Figure 1.Quadrifurcation of the left main coronary artery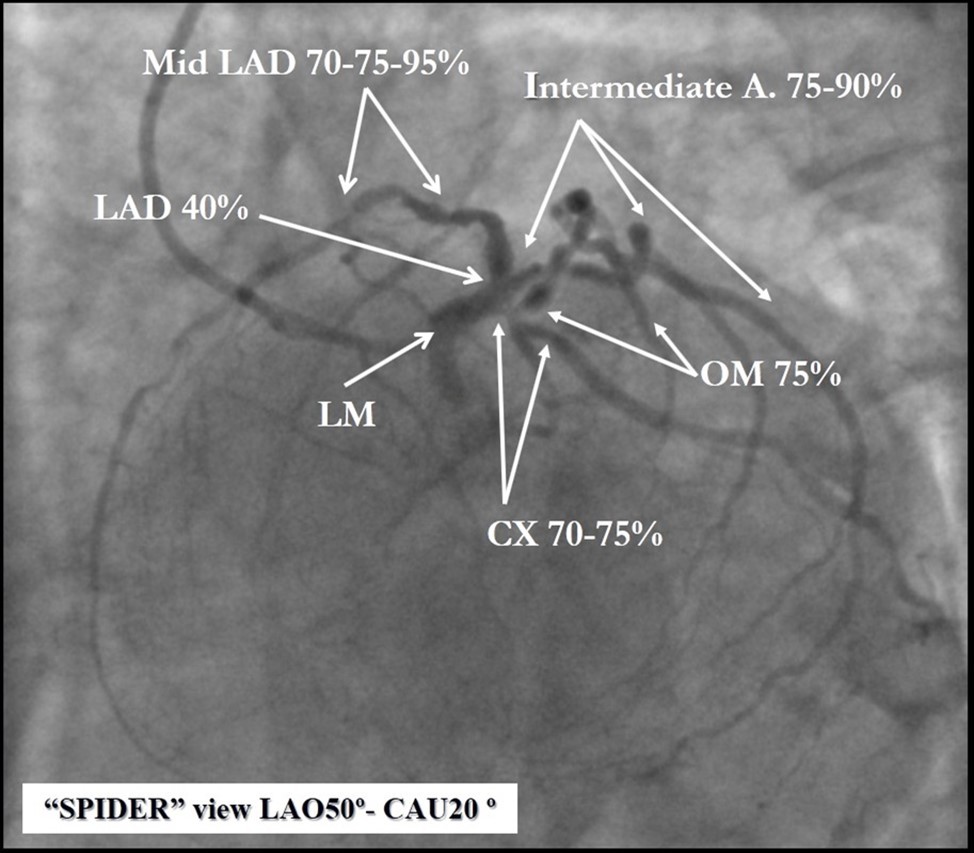
Figure 2.Schematic presentation of the left main quadrifurcation.
Figure 3.Prolonged diffuse severe 90-95% stenosis of mid-segment of the right coronary artery. A - Left anterior oblique 45° projection; B – Right anterior oblique 45° projection.
Figure 4.A - 50% stenosis of the distal segment of the LMCA; B - 70-75-95% stenosis in mid-segment of the LAD.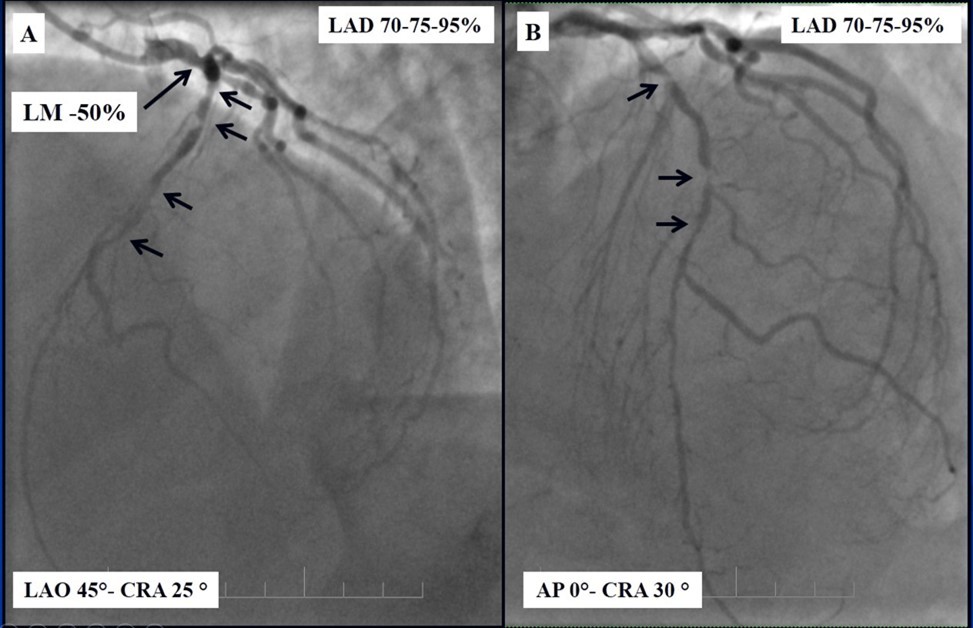
The SYNTAX score II was calculated to be 56.
After CAG, expected risks were re-evaluated, for coronary revascularization CABG was recommended. After consulting with the patient and family members ( based on past experience, they did not agree to the operation) it was decided to perform staged PCI to achieve complete revascularization; without improvement of the coronary blood supply, the patient should have to remain symptomatic and was soon doomed to myocardial infarction and sudden cardiac death.
The goal of the intervention was complete revascularization and improvement of the contractile function of the heart.
The plan of the intervention included 2 stages:
1. Stenting of RCA and mid LAD.
2. Stenting of LMCA and its quadrifurcation.
Both stages were performed with only right radial artery access, using a 6fr sheath, and 6fr Extra Backup coronary guide catheter (Launcher, Medtronic) for left coronary artery, and 6Fr Amplatz Left 1.0 coronary guide catheter (Launcher, Medtronic) for right coronary artery.
In the first stage, despite the fact that BMS is contraindicated in diabetic patients, RCA was stented with 3 bare-metal stents (BMS) (Rebel, Boston Scientific) (due to financial problems - drug-eluting stents was not covered by insurance). We used BMS to have at least temporarily patent RCA during LMCA stenting (Figure 5) (we believe that, when RCA is functional, LMCA stenting is safer). LAD was stented with 2 drug-eluting stents (Resolute Integrity, Medtronic). After the first PCI patient’s symptoms were relieved (Figure 6).
Figure 5.A, B, C - Stenting of the RCA with BMS; D - Angiography result.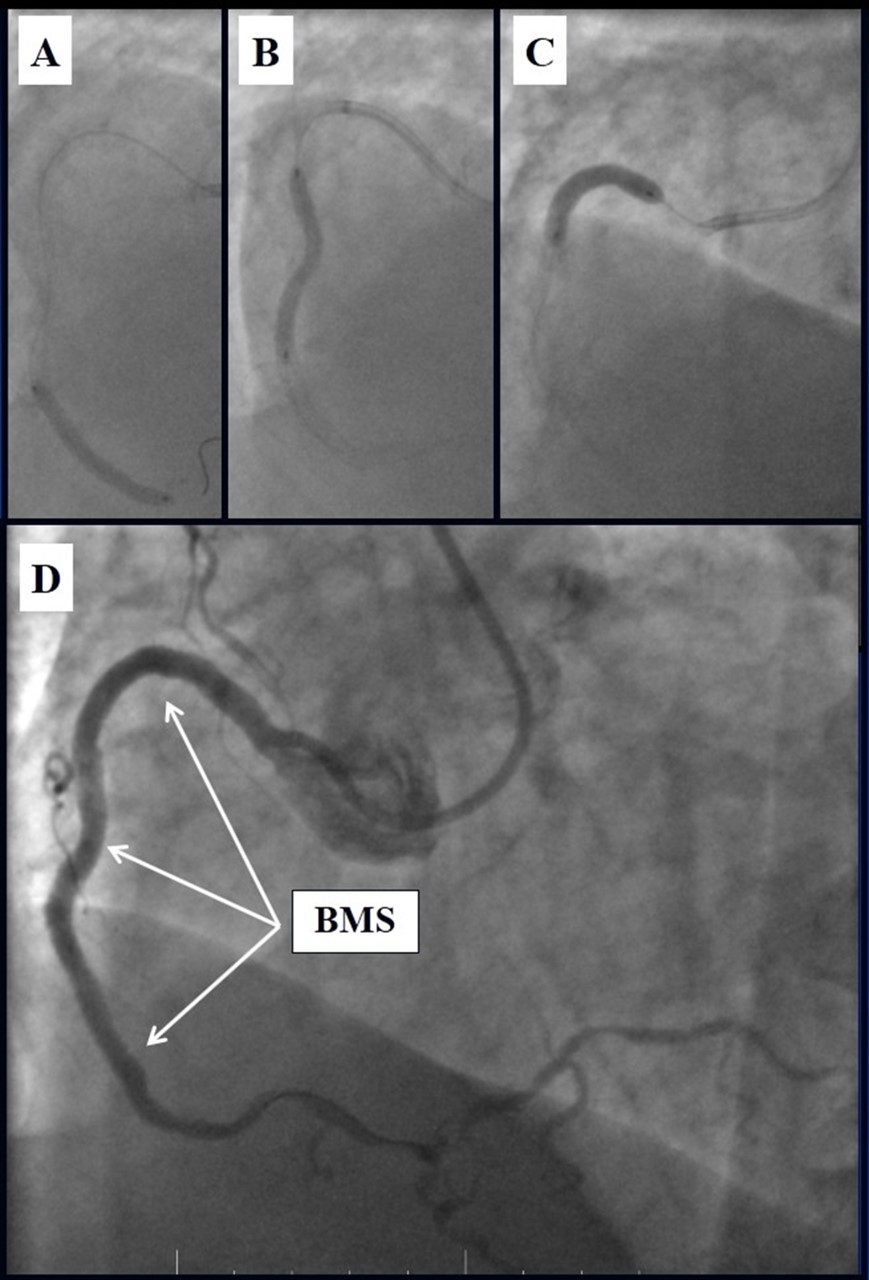
Figure 6.A, B - Stenting of the LAD with DES; C - Angiography result.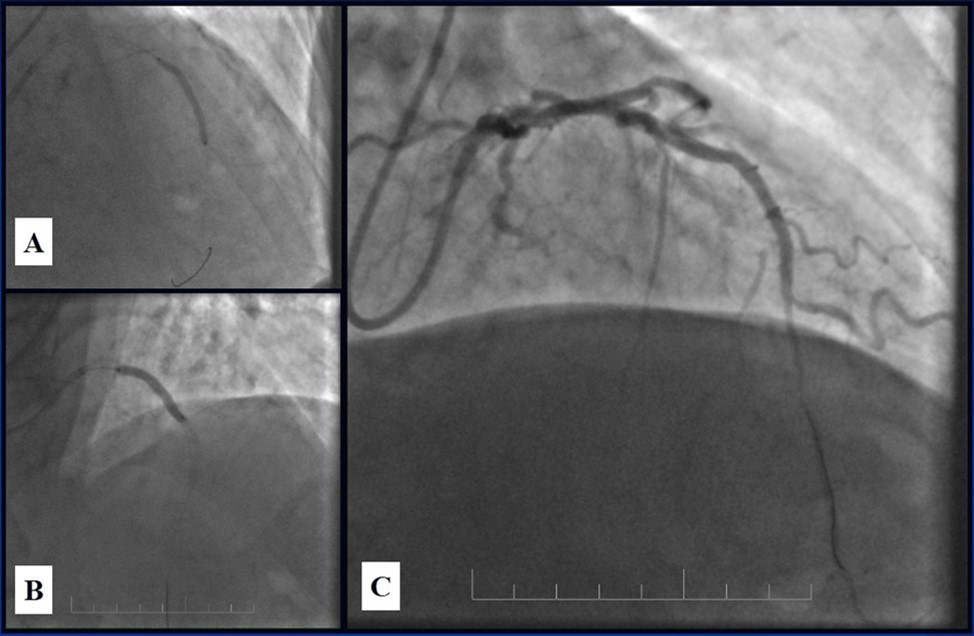
Due to financial problems the second stage was performed after 3 months (during this time the patient solved his financial problems). CAG revealed patent stents in LAD (Figure 7), and 60-70% restenosis by BMS in RCA (Figure 8). In-stent restenosis was treated by plain old balloon angioplasty (POBA), the optimal result was obtained (Figure 9). After LMCA quadrifurcation balloon predilation, 2.5×26 mm DES (Resolute Integrity, Medtronic) was implanted in the IMA, using a modified balloon mini-crush technique. The stent was minimally protruded in the LMCA and its edge was crushed by preloaded MB balloon. Next 2.5×30 mm DES (Resolute Integrity, Medtronic) was implanted in OM1 through the CX (first marginal and circumflex arteries in this particular case have the same ostium). The stent was protruded in the LMCA as in conventional modified balloon crush stenting technique, after stent deployment, its balloon was pulled back and overinflated, then protruded stent was crushed by preloaded MB balloon (Figure 10). 3.5×15 mm DES was implanted in the LMCA so that distal part of the stent covered ostial and proximal segments of the LAD. Sequential post-dilatations were performed using a kissing balloon technique (1. LMCA-LAD-IMA,2. LMCA-LAD-CX-1OM). After post-dilatations, through the stent implanted in CX-OM1, coronary wire and smaller diameter balloon (2.0 mm) were advanced in direction of the CX mid-segment and by balloon dilatation stent’s strut was opened (provisional stenting technique for CX). Finally, the proximal optimization technique was performed in the LMCA using a 3.5 mm diameter non-compliant balloon (Figure 11). The final angiographic image was good, the intervention ended without complications (Figure 11, Figure 12). We could not confirm the result with IVUS or OCT due to several technical and financial problems (not covered by insurance). 1 month after PCI, at regular checkout, the ejection fraction was 48%, the functional class of the Congestive Heart Failure decreased from class II-III to class I and the patient complaints have been disappeared.
Figure 7.Patent stents in LAD; A – AP-cranial 30° projection, B – Right anterior oblique 20°/caudal 20° projection.
Figure 8.RCA, 60-70% in-stent restenosis in BMS
Figure 9.RCA; A, B - Plain old balloon angioplasty; C - Angiography result.
Figure 10.Stenting of the LMCA quadrifurcation: A, B - balloon modified mini crush stenting of the IMA, C - angiography result, D,E - modified balloon crush stenting of the CX-OM1, F - angiography result.
Figure 11.Stenting of the LMCA quadrifurcation: A, B – Stenting of the LMCA; C –Kissing balloon post dilatation of the IMA-LMCA-LAD; D - Kissing balloon post dilatation of the CX-OM1-LMCA; E, F - angiography result.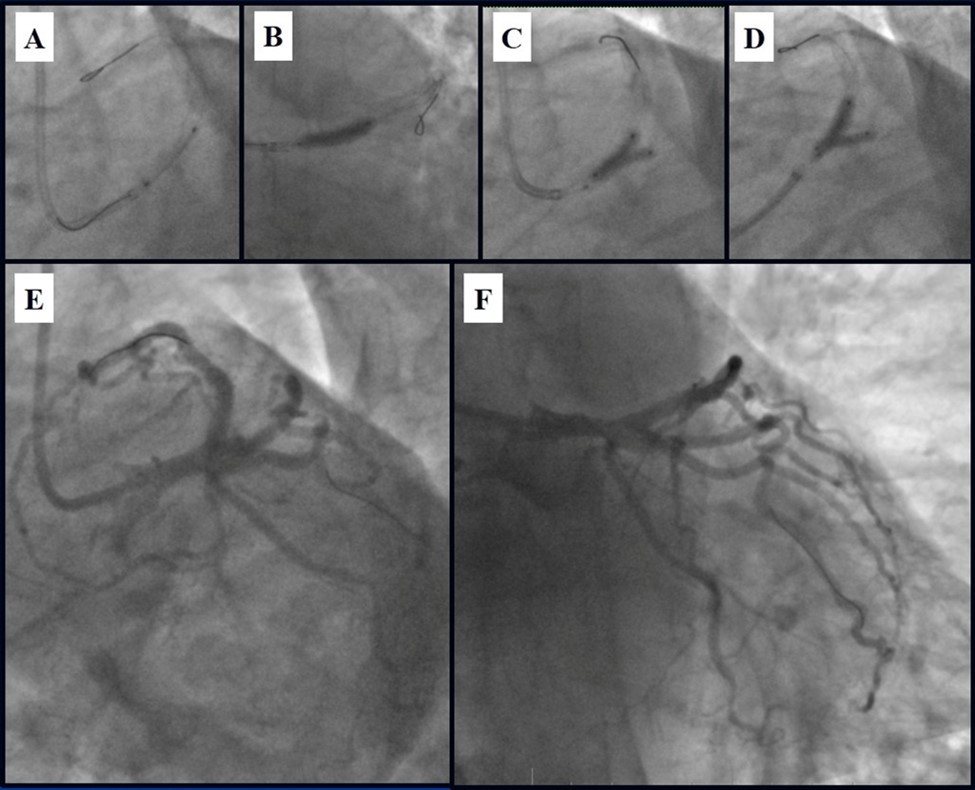
Figure 12.Schematic presentation of the implanted stents, “spider” projection.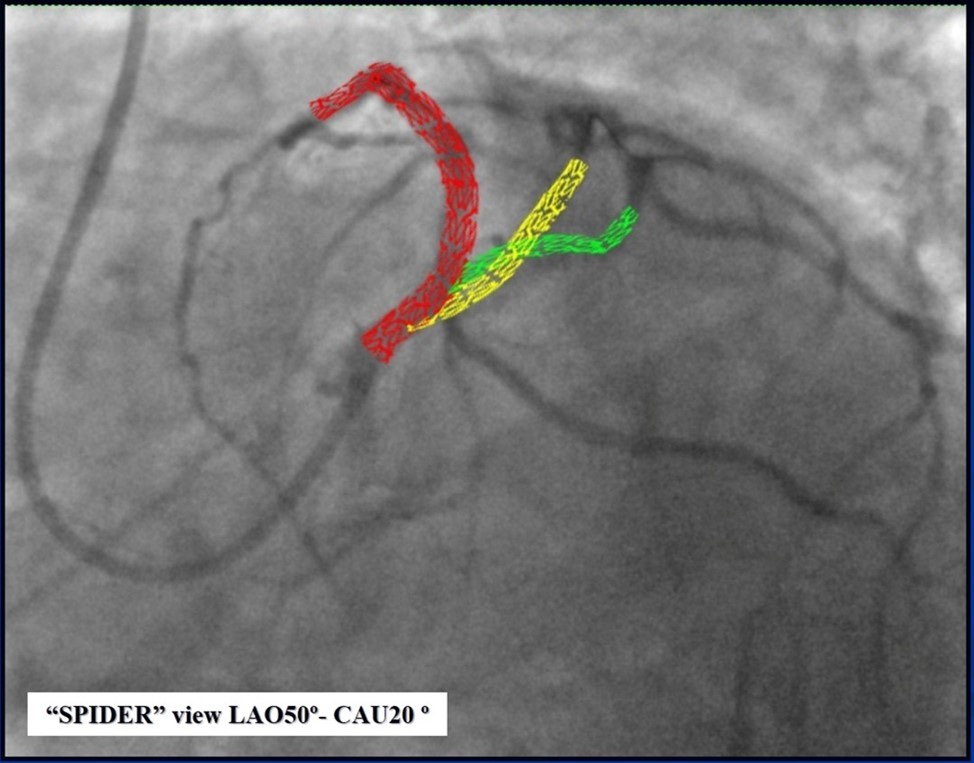
Subsequent coronary angiography eight months after the last PCI revealed patent stents with mild, non-significant restenosis in DES and 50-60% in-stent restenosis in BMS (Figure 13, Figure 14).
Figure 13.Subsequent CAG eight months after last PCI; A - Patent stents with mild, non-significant restenosis in left coronary artery; B - 50-60% in-stent restenosis in RCA.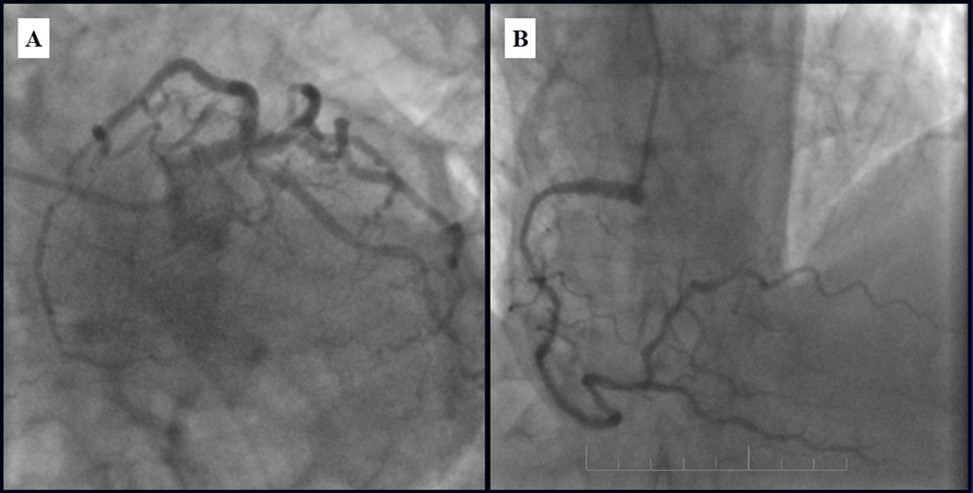
Figure 14.Left coronary artery, follow-up CAG eight months after last PCI.
Revascularization of the LMCA quadrifurcation lesion in patients with the use of PCI and CABG methods is associated with a certain procedural risk. According to experience CABG operation in the LMCA quadrifurcation lesion usually, give a good procedural result and good prognosis. New tools and techniques have allowed interventional cardiologists to accomplish more and more complex lesions, but PCI for LMCA quadrifurcation lesion is so rare that there is not enough data to compare to CABG.
In the case presented above, although the high SYNTAX score would have indicated the need for surgical revascularization (CABG), because of the poor functional status (NYHA II-III class), diabetes, amputated lower leg, patients old age (83 y), and finally due to patient refusal of the CABG, we found, that PCI was good option and in case of success could provide the optimal remote result.
In the literature available to us, have been reported only a single case using the femoral assess, and large diameters guide catheters (2). Our case is unique because we have achieved an optimal result without IVUS guidance, using only single radial artery asses, and comparably small-sized single guide catheter (6Fr). The final angiographic result was good; however, we could not confirm the optimal result with IVUS or OCT, due to several technical and financial (this procedures were not covered by insurance) problems in our hospital.
Conclusion
As a result of interventional measures and optimal medication treatment:
The patient received complete revascularization.
The quality of life has improved significantly.
The risks were significantly reduced, and the prognosis improved.
More than three years after the intervention, the patient has no complaints (according to MACE), there is no need for hospitalization, the patient performs regular physical activity without angina, echocardiography data remains unchanged, ejection fraction ranges is from 45-48%. At the present time the patient is 87 years old, he drinks one glass of red wine every day and feels pretty good.
It should be concluded that in case of the selection of suitable patients and the use of the appropriate revascularization technique, LMCA quadrifurcation lesion can be successfully treated with PCI.
We believe that IVUS or OCT guidance are not obligatory, but are very important for proper stent sizing, deployment, and also it is important to confirm final optimal result.
Abbreviations
References
- 1.Latib A, A. (2008) Colombo, Bifurcation disease: what do we know, what should we do?. , J Am Coll Cardiol Intv 1, 218-226.
- 2.Tyczyński P, Pręgowski J, Skowroński J, Wojtkowska I, Brutkiewicz A et al. (2017) Left main coronary artery quadrifurcation and acute coronary syndrome.KardiolPol. 75(4), 398.
- 3.Khona P, Kulkarni D, U. (2019) Branching pattern of left coronary artery in north Karnataka population. , IP Indian Journal of Anatomy and Surgery of Head, Neck 3(4), 93-96.
- 4.BAPTISTA C A C, DIDIO L J A, JPRATES C. (1991) Types of Division of the Left Coronary Artery and the Ramus Diagonalis of the Human Heart. Japanese heart journal. 32(3), 323-335.
