Abstract
MicroRNAs are short sequences of non-coding RNAs crucial in regulation of cell development, proliferation and differentiation. Some of them showed to be related with the expression of osteogenic genes. Aim of the present review was to evaluate the biological effects of titanium implant surfaces activated with miRNAs or antimiRNAs. A bibliographical electronic research was carried out on PubMed/Medline. Articles investigating the influences of miRNA functionalized surfaces on human or animal cells were included. Reports were excluded if investigating surfaces modified with molecules different from miRNAs, if miRNAs were not loaded to titanium surfaces. Five articles met the inclusion criteria. Surfaces functionalized with miRNAs showed to up-regulate the expression of osteogenic genes like RUNX2, OPN, OCN, BMP, OSX, ALP, COL1 and COL3. Investigated surfaces additionally showed more bone-like mineralized tissues, bone lacunae, osteocytes and new blood vessels. MiRNAs loaded to titanium implant surfaces stimulate the expression of genes related to osteoblasts differentiation, osteogenesis, osseointegration and reparation of mineralized tissues. Vectors used to link titanium surfaces and miRNAs did not show cytotoxicity or interference with cells’ viability.
Author Contributions
Academic Editor: William Cordeiro de Souza, University of Contestado, Brazil.
Checked for plagiarism: Yes
Review by: Single-blind
Copyright 2018 Riccardo Di Gianfilippo
 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Competing interests
No external funding, apart from the support of the authors' institution, was available for this study. The author declares that there are no conflicts of interest in this study and nothing to disclose.
Citation:
Introduction
The role of epigenetics in medicine and in dentistry has grown impressively during the last decade and epigenomics is considered as one of the most important cutting-edge subjects of scientific discovery.1,2,3 The mainly studied epigenetic molecular mechanisms are miRNA production, DNA methylation and histone modification.
MicroRNAs (or miRNAs, or miR) are short sequences of non-coding RNAs (ncRNAs) composed by seventeen/twenty-five nucleotides.1 They are crucial in regulation of development, proliferation, differentiation, apoptosis and response to different extracellular signals and stress. They are thought to be related with the expression of osteogenic genes like RUNX2 and SMAD5.4 MicroRNA pathways regulate gene expression by inducing degradation and/or translational repression of target mRNAs.5 It is believed that more than 40% of all human genes are under the regulation of miRNAs.6 MessengerRNA can bind the promoter of specific microRNAs activating an auto-regulatory feedback loop; thus, when a specific mRNA is up-regulated, the related miRNA is also over-expressed.7 Each miRNA may target hundreds of mRNAs, and some targets are affected by multiple miRNAs. Probably, miRNAs are fundamental in the maintenance of pluripotency and undifferentiation of adult stem cells; indeed, several miRNAs appear to significantly modulate the differentiation of mesenchymal precursors in osteoblast cells, regulating the activity of transcription factors.8
In the field of Periodontology, the expression of miR-181b, mi-R19b, miR-30a, miR-let 7a, and miR-301a were found lower in healthy people if compared with subjects with periodontitis.9 MicroRNA-155 expression was found linked to the IL-1 signaling mechanisms and to the inflammatory response.10 In the field of Implant Dentistry, new titanium surfaces were functionalized to increase the expression levels of osteogenic genes.11 However, despite the interest on the use of biological activators to enhance osseointegration of dental implants, the available knowledge seems to be scarce.
Therefore, aim of the present review was to investigate in vitro and in vivo publications reporting biological effects of the use of microRNAs as activators of implant surfaces on bone formation and osseointegration.
Materials and Methods
This review was conducted following the Cook and Mulrow’s principles.12,13 A bibliographical electronic research was carried out on PubMed/Medline, selecting all potentially relevant articles dealing with the effects of the use of miRNAs as implant surfaces’ activators. All included articles were appraised, synthesized, interpreted and discussed.
Search Strategy
The following key terms and boolean connectors were used: ((miRNA) OR (miR) OR (microRNA)) AND ((implant dentistry) OR (dental implants) OR (orthopedic implant) OR (titanium surfaces) OR (osseointegration) OR (titanium dioxide) OR (zirconia)).
The screening of resulted articles was performed over three phases. The first phase consisted in the exclusion of all publications not related to dentistry, to implantology, and to miRNAs based on title and abstract screening. The second phase consisted in the exclusion of all those articles not aimed to investigate the effects of the loading of miRNAs on implant surfaces after full-text examination. The third phase consisted in the review of included articles.
For each included study, several data regarding authors, type of the study, surfaces tested, cells studied, follow-up, genes investigated, and molecular effects were re-wrote.
The search was conducted on articles published up to August 20th, 2018.
Inclusion Criteria
Articles investigating the effects of implant surfaces functionalized with miRNAs were included in the present review. Studies reporting gene activation or protein production were accepted. No filters like language or date of publication were used.
Exclusion Criteria
Articles were excluded if investigating the effects of dental implant surfaces modified with molecules different from miRNAs, and if miRNAs were not loaded to titanium surfaces or to other dental implant surfaces.
Results
The electronic search started with 91 articles and resulted in the inclusion of 5 articles. All included studies were in vitro articles investigating the genetic effects of surfaces functionalized with miRNAs compared with not functionalized surfaces on human or animal cells.14,15,16,17,18 One of the included studies had an in vivo component based on the unscrew torque of functionalized surfaces.18 Details of the included studies are reported in Table 1.
Table 1. Types of surfaces, cells and cellular effects during the investigated periods of included articles.| Author (Year) | Type | Surfaces tested | Type of cells | Evaluated timepoints | Gene and molecules studied | Molecular effects |
| Song W. (2018) | In vitro. | TN+Ca/antimiR-138;TN+Ca/NC;TN+Milli-Q. | Human mesenchymal stem cells. | 2 weeks. | siBCL2L2, siCKIP-1, miR-29b, miR-26a, antimiR-138. | ↓Focal adhesion kinase signalling in 2TN+Ca/antimiR-138.↓miR-138 in TN+Ca/antimiR-138. |
| Shao D. (2018) | In vitro. | MAO+miR122;miR122 control;blank control. | Rat bone marrow mesenchymal stem cells. | 48 hours, 3 and 7 days, 4 and 8 weeks. | ALP, COL1, RUNX2, OSX, OCN, ERK, p-ERK, BMP-2. | ↑RUNX2, OSX, OCN, COL1, ALP and BMP-2 for MAO+miR122.Bone-like mineralized tissues for MAO+miR122.Bone lacunae and osteocytes containing new blood vessels for MAO+miR122.Fibrous repair for blank control group. |
| Liu X. (2017) | In vitro and in vivo. | Ti+PLGA/AuNP-antagomiR204; PLGA control;blank control. | Rat bone marrow mesenchymal stem cells. | 5-10 days. | miR204, BMP, OPG, ALP, RUNX2, COL1. | ↑BMP, OPG, ALP, RUNX2, and COL1 for PLGA/AuNP-antagomiR204.In vivo: higher removal torque for implant with PLGA/AuNP-antagomiR204. |
| Wang Z. (2015) | In vitro. | MAO;CS/HA/miR-21. | Human bone marrow mesenchymal stem cells. | 3, 6, 9 days | COL1, COL3, RUNX2, OPN, OCN. | ↑COLI, COL3, RUNX2, OPN, OCN in miR-21 group. |
| Wu K. (2013) | In vitro. | MAO+miR29b;MAO+antimiR138;MAO. | Rat bone marrow cells. | 7, 14 days. | BMP, OCN, OSX, RUNX2, COL1, ALP. Collagen secretion. ECM mineralized nodules | ↑BMP, OCN, OSX, RUNX2 for MAO+antimiR-138. ↑ALP for MAO+miR-29b group. ↑COL1 for MAO+miR-29b at day 7. ↑COL1 for MAO+antimiR- 138 at day 14. ↑Collagen secretion for MAO+miR at day 14.↑Mineralization for MAO+miR-29b and MAO+antimiR-138. |
Regarding the surfaces challenged, Song et al.16 used titanium surfaces loaded with calcium and antimiR-138; Shao et al.17 used microarc-oxidated titanium surfaces (MAO) loaded with miR122; Liu et al.18 used titanium surfaces with miR204 inhibitor conjugated with gold nanoparticles and dispersed in the polylactic-co-glycolic acid; Wang et al.14 used MAO surfaces activated with microRNA-21; Wu et al.15 used MAO surfaces with microRNA-21 and MAO surfaces with antimicroRNA-138. As regards the population cells, three authors used rat bone marrow cells15,17,18 while two used human mesenchymal stem cells.14,16 The investigated genes and proteins were alkaline phosphatase (ALP), bone morphogenetic protein (BMP), collagen type 1α1 (COL1), collagen type 3α1 (COL3), osteocalcin (OCN), osteopontin (OPN), runt-related transcription factor (RUNX2), extracellular signal-regulated kinases (ERK), phosphorylated ERK (p-ERK), siBCL2L2, siCKIP-1, miR-29b, miR-26a, antimiR-138.
All the challenged test surfaces did not exhibit any apparent cytotoxicity, nor affected cells’ viability if compared to control samples. All articles found that test surfaces up-regulated the expression of osteogenic genes. Shao et al.17 found that the expression of RUNX2, OSX, OCN, COL1, ALP and BMP-2 was increased around surfaces loaded with miR122. Moreover, while test surfaces showed more bone-like mineralized tissues, bone lacunae, osteocytes and new blood vessels, control ones showed fibrous repair processes. Liu et al.18 reported that test surfaces induced higher expression of BMP, OPG, ALP, RUNX2 and COL1, and that reached higher level of osseointegration evaluated with unscrew torque. Song et al.16 reported less focal adhesion kinase signaling and miR-138 expression in test surfaces. Wang et al.14 found an increased activity for COL1, COLIII, RUNX2, OPN and OCN on titanium surfaces functionalized with miRNA-21. Wu et al.15 found that the expression of BMP, OCN, OSX and RUNX2 was higher for MAO surfaces linked to antimiRNA-138; that the ALP expression was greater for MAO surfaces with miRNA-29b; and that the expression of collagen was also influenced by the passing of time with higher values at day 7 for surfaces with miRNA-29b and higher values at day 14 for surfaces with antimiRNA- 138. Moreover, the functionalized surfaces inducted a greater amount of secreted collagen and mineralized nodules.
Discussion
MicroRNAs are a group of non-coding RNAs which contribute to epigenetic processes by preventing transcription of RNA from DNA or by destroying mRNAs after they are produced.1 Application of the modern knowledge in the field of epigenetics could be helpful to develop new surfaces able to reduce bone resorption, to stimulate bone deposition and to improve the osseointegration. Therefore, aim of the present study was to review all the available articles comparing the biological effects of not- functionalized implant surfaces with surfaces functionalized with miRNAs or antimiRNAs.
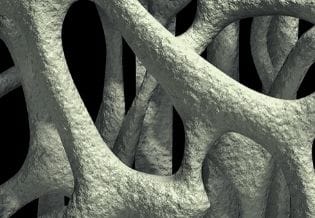
Interestingly, microarc oxidated surfaces were a common choice for control groups. Micro-rough and nano-rough surfaces proved to facilitate interactions with bone cells19,20 and, in particular, the microarc oxidated titanium surfaces (MAO) showed to have favourable effects on implant osseointegration through the induction of apatite deposition and promotion of osteoblast functions.21 However, improvements in implant topography alone could be not enough to stimulate the maximum osteogenic potential. An effective strategy for promoting an even better osseointegration involves the loading of advantageous biomolecules on implant surfaces to stimulate cellular differentiation, migration, gene expression and deposition of extracellular matrix.22,23,24 Even though there are available studies investigating the loading of oligonucleotides or peptides25,26 only a few studies investigated miRNAs. Articles challenging small-interfering RNAs (siRNA) observed a 30−45% reduction in cell viability27 and this evidence may support the idea that miRNAs are more biologically friendly than siRNAs. At present, the miRNAs used as activators for implant surfaces are miR122, miR-21, miR-29b, antimiR204 and antimiR138.
MicroRNA-122 is one of the main regulators of osteogenic differentiation of bone marrow mesenchymal stem cells through the alteration of the ERK signaling pathway.28 MicroRNA-21 is highly expressed during the osteogenic differentiation to repress stemness maintenance in osteoblasts.29 MicroRNA-21 exert its osteogenic function through the stabilization and accumulation of β-catenin, interfering with the PI3K-AKT-GSK3β pathway.30 Its overexpression accelerate osteogenesis in both human umbilical cord mesenchymal stem cells and human bone marrow MSCs.30 MicroRNA-29b has been demonstrated to be a phenotype regulator of osteoblasts by targeting anti-osteogenic factors such as histone deacetylase 4 and modulating bone extracellular matrix proteins.31 AntimiRNA-204 inhibit the effect of microRNA-204 as a negative regulator of RUNX2 during the osteogenic differentiation of mesenchymal stem cells.32 AntimiR-138 has been shown to enhance in vivo bone formation by inhibiting miRNA-138.33 Indeed, downregulating endogenous levels of miRNAs that play a negative role in osteogenesis has also been demonstrated to promote osteogenesis.34
Gene expression of several osteogenic genes was evaluated and found influenced by the use of miRNAs. Runt-related transcription factor 2 (RUNX2) is a transcription factor that regulates the differentiation of osteoblasts. It plays a major role in the synthesis of bone extracellular matrix proteins, including collagen type I, osteopontin, bone sialoprotein, osteocalcin, fibronectin, and other factors.35 Osteoprotegerin (OPN) is a mediator of cell-matrix and matrix-matrix cohesion during the formation, turnover and repair of normal and pathological mineralized tissues. The production of OPN is one of the earliest and latest, secretory activities of the osteoblast lineage and this activity manifests itself morphologically as a cement line or a lamina limitans at bone matrix interfaces.36 Osteocalcin (OCN) secreted by mature osteoblast is the non-collagenous bone matrix protein. The exact function of OCN still remain unclear, however, it is the determinant of bone formation and could regulate the rate and direction of mineral formation.35 Bone morphogenic proteins (BMP) promote differentiation of mesenchymal stem cells in osteoblasts and stimulate osteogenesis in mature osteoblasts.37,38 Osterix (Osx) is an osteoblast-specific transcription factor fundamental for bone formation and osteoblast differentiation. Osx, downstream of RUNX2, is specifically expressed in osteoblasts and chondrocytes.39,40,41,42 Alkaline phosphatase (ALP) is a glycoprotein that catalyzes the hydrolysis of phosphate monoesters at basic pH values. It is divided into 4 isoenzymes, the bone isoenzyme in involved in mammalian bone calcification.43 Type I collagen (COL) is the major constitutive protein of bone tissue. It has satisfactory biocompatibility and has the function to induce the bone formation.44
Because of the exiguous number of existing articles, further studies are required for a better comprehension of the effects induced by implants activated with miRNAs on osseogenetic genes. At present, only studies with an indirect evidence are available. Besides, if the increased expression of osseogenetic genes caused by miRNAs could lead to a high rate of osseointegration in human still remains undocumented. Despite the small amount of data, all the included studies agreed that implant surfaces functionalized with miRNAs or antimiRNAs stimulated a higher expression of osseogenic genes, higher differentiation and higher deposition of collagen and mineralized nodules.
Conclusion
The present review confirmed the effectiveness of miRNAs loaded to titanium implant surfaces in stimulating the expression of genes related to osteoblasts differentiation, osteogenesis, osseointegration and reparation of mineralized tissues. More studies are needed for a complete comprehension of the effects induced by miRNAs on osteoblast precursors. Further studies are required to define the role of time and to investigate the effects of miRNA functionalized surfaces with in vivo models. The knowledge in the field of epigenetics could be used to develop new miRNA activated surfaces, genetically and biologically friendly, able to enhance bone deposition.
References
- 1.S D Williams, T E Hughes, C J Adler, A H Brook, G C Townsend. (2014) Epigenetics: a new frontier in dentistry. Aust Dent J;59 Suppl 1, 23-33.
- 2.M A Rothstein, Cai Y, G E Marchant. (2009) The ghost in our genes: legal and ethical implications of epigenetics. , Health Matrix Clevel 19, 1-62.
- 3.S P Barros, Offenbacher S. (2009) Epigenetics: connecting environment and genotype to phenotype and disease. J Dent Res;88:. 400-408.
- 4.Fakhry M, Hamade E, Badran B, Buchet R, Magne D. (2013) Molecular mechanisms of mesenchymal stem cell differentiation towards osteoblasts. , World J Stem Cells;5: 136-148.
- 5.Palmieri A, Pezzetti F, Brunelli G, Lo Muzio L, Scarano A. (2008) Short-period effects of zirconia and titanium on osteoblast microRNAs. Clin Implant Dent Relat Res;10:. 200-205.
- 6.Bentwich I, Avniel A, Karov Y, Aharonov R, Gilad S. (2005) Identification of hundreds of conserved and nonconserved human microRNAs. Nat. Genet;37: 766-770.
- 7.Sylvestre Y, V De Guire, Querido E, U K Mukhopadhyay, Bourdeau V. (2007) An E2F/miR-20a autoregulatory feedback loop. , J Biol Chem;282: 2135-2143.
- 8.J O Gordeladze, J E Reseland, Duroux-Richard I, Apparailly F, Jorgensen C. (2009) From stem cells to bone: phenotype acquisition, stabilization, and tissue engineering in animal models. , ILAR J 51, 42-61.
- 9.Y H Lee, H S Na, S Y Jeong, S H Jeong, H R Park. (2011) Comparison of inflammatory microRNA expression in healthy and periodontitis tissues. Biocell;35: 43-49.
- 10.Ceppi M, Pereira P M, Dunand-Sauthier I, Barras E, Reith W. (2009) MicroRNA-155 modulates the interleukin-1 signaling pathway in activated human monocyte-derived dendritic cells. Proc Natl Acad Sci U S A;106: 2735-2740.
- 11.R Di Gianfilippo, C Di Gianfilippo, Prato Pini, G. (2017) The Role of Epigenetics on Dental Implant Therapy: A Systematic Review. , Epigenomes 1.
- 12.D J Cook, C D Mulrow, R B Haynes. (1997) Systematic reviews: synthesis of best evidence for clinical decisions. Ann Intern Med;126:. 376-380.
- 13.Mulrow C, Langhorne P, Grimshaw J. (1997) Integrating heterogeneous pieces of evidence in systematic reviews. Ann Intern Med;127: 989-995.
- 14.Wang Z, Wu G, Feng Z, Bai S, Dong Y. (2015) Microarc-oxidized titanium surfaces functionalized with microRNA-21-loaded chitosan/hyaluronic acid nanoparticles promote the osteogenic differentiation of human bone marrow mesenchymal stem cells. , Int J Nanomedicine;10: 6675-6687.
- 15.Wu K, Song W, Zhao L, Liu M, Yan J. (2013) MicroRNA functionalized microporous titanium oxide surface by lyophilization with enhanced osteogenic activity. , ACS Appl Mater Interfaces;5: 2733-2744.
- 16.Song W, Yang C, Svend Le DQ, Zhang Y, Kjems J.(2018).Calcium-MicroRNAComplex-Functionalized Nanotubular Implant Surface for Highly Efficient Transfection and Enhanced Osteogenesis of Mesenchymal Stem Cells. , ACS Appl Mater Interfaces;10: 7756-7764.
- 17.Shao D, Wang C, Sun Y, Cui L. (2018) Effects of oral implants with miR122modified cell sheets on rat bone marrow mesenchymal stem cells. Mol Med Rep;17:. 1537-1544.
- 18.Liu X, Tan N, Zhou Y, Wei H, Ren S. (2017) Delivery of antagomiR204-conjugated gold nanoparticles from PLGA sheets and its implication in promoting osseointegration of titanium implant in type 2 diabetes mellitus. , Int J Nanomedicine;12: 7089-7101.
- 19.J W Park, Y J Kim, J H, T G Kwon, Y C Bae. (2010) Effects of phosphoric acid treatment of titanium surfaces on surface properties, osteoblast response and removal of torque forces. , Acta Biomater;6: 1661-1670.
- 20.J W Park, Y J Kim, Jang J H, Song H. (2010) Osteoblast response to magnesium ion-incorporated nanoporous titanium oxide surfaces. Clin Oral Implants Res;21:. 1278-1287.
- 21.Li L H, Y M Kong, H W Kim, Y W Kim, Kim H E. (2004) Improved biological performance of Ti implants due to surface modification by micro-arc oxidation. Biomaterials;25: 2867-2875.
- 22.Wildemann B, Lubberstedt M, N P Haas, Raschke M, Schmidmaier G. (2004) IGF-I and TGF-beta 1 incorporated in a poly(D,L-lactide) implant coating maintain their activity over long-term storage-cell culture studies on primary human osteoblast-like cells. , Biomaterials; 25, 3639-3644.
- 23.U M Wikesjo, Qahash M, Polimeni G, Susin C, R H Shanaman. (2008) Alveolar ridge augmentation using implants coated with recombinant human bone morphogenetic protein-2: histologic observations. , J Clin Periodontol 35, 1001-1010.
- 24.Polimeni G, U M Wikesjo, Susin C, Qahash M, R H Shanaman. (2010) Alveolar ridge augmentation using implants coated with recombinant human growth/differentiation factor-5: histologic observations. , J Clin Periodontol 37, 759-768.
- 25.Monaghan M, Pandit A. (2011) RNA interference therapy via functionalized scaffolds. Adv Drug Deliv Rev;63:. 197-208.
- 26.C M Jewell, D M Lynn. (2008) Surface-Mediated Delivery of DNA: Cationic Polymers Take Charge. Curr Opin Colloid Interface Sci;13:. 395-402.
- 27.M O Andersen, J V Nygaard, J S Burns, M K Raarup, J R Nyengaard. (2010) siRNA nanoparticle functionalization of nanostructured scaffolds enables controlled multilineage differentiation of stem cells. Mol Ther;18:. 2018-2027.
- 28.Qiu Z, Dai Y. (2014) Roadmap of miR-122-related clinical application from bench to bedside. Expert Opin Investig Drugs;23:. 347-355.
- 29.Mei Y, Bian C, Li J, Du Z, Zhou H. (2013) miR-21 modulates the ERK-MAPK signaling pathway by regulating SPRY2 expression during human mesenchymal stem cell differentiation. , J Cell Biochem;114: 1374-1384.
- 30.Y B Meng, Li X, Z Y Li, Zhao J, X B Yuan. (2015) microRNA-21 promotes osteogenic differentiation of mesenchymal stem cells by the PI3K/beta-catenin pathway. , J Orthop Res 33, 957-964.
- 31.Li Z, M Q Hassan, Jafferji M, R I Aqeilan, Garzon R. (2009) Biological functions of miR-29b contribute to positive regulation of osteoblast differentiation. , J Biol Chem;284: 15676-15684.
- 32.Huang J, Zhao L, Xing L, Chen D. (2010) . MicroRNA-204 regulates Runx2 protein expression and mesenchymal progenitor cell differentiation. Stem Cells;28: 357-364.
- 33.Eskildsen T, Taipaleenmaki H, Stenvang J, B M Abdallah, Ditzel N. (2011) MicroRNA-138 regulates osteogenic differentiation of human stromal (mesenchymal) stem cells in vivo. Proc Natl Acad Sci U S A;108: 6139-6144.
- 34.Stenvang J, Petri A, Lindow M, Obad S, Kauppinen S. (2012) Inhibition of microRNA function by antimiR oligonucleotides. Silence;3: 1
- 35.Meng W, Zhou Y, Zhang Y, Cai Q, Yang L. (2013) Effects of hierarchical micro/nano-textured titanium surface features on osteoblast-specific gene expression. Implant Dent;22:. 656-661.
- 36.McKee M D, Nanci A. (1996) Osteopontin at mineralized tissue interfaces in bone, teeth, and osseointegrated implants: ultrastructural distribution and implications for mineralized tissue formation, turnover, and repair. Microsc Res Tech;33: 141-164.
- 37.Chen G, Deng C, Y P Li. (2012) TGF-beta and BMP signaling in osteoblast differentiation and bone formation. , Int J Biol Sci;8: 272-288.
- 38.Murray S S, J Brochmann Murray E, J C Wang, Duarte M E. (2016) The history and histology of bone morphogenetic protein. Histol Histopathol;31:. 721-732.
- 39.Chen D, Li Y, Zhou Z, Xing Y, Zhong Y. (2012) Synergistic inhibition of Wnt pathway by HIF-1alpha and osteoblast-specific transcription factor osterix (Osx) in osteoblasts. PLoS One;7:e52948
- 41.L J Raggatt, N C Partridge. (2010) Cellular and molecular mechanisms of bone remodeling. , J Biol Chem;285: 25103-25108.
- 42.P J Meunier. (1986) Cellular mechanisms of bone remodeling evaluated at the intermediary level of organization of bone. Adv Exp Med Biol;208:. 247-254.