Abstract
With an increased intake of processed carbohydrates and refined sugars, the obesity rate has shot up in the past decade giving rise to mental and physical health problems. These individuals are also the most vulnerable to a number of other diseases including the current pandemic of Covid-19. This paper aims to address the knowledge gap that is required to promote a healthy lifestyle for mental and physical wellbeing. The paper also analyses a number of different studies conducted and helps in understanding obesity as a strong risk factor to various disorders. Despite constant recommendations from healthcare organisations to address the importance of weight regulation, the process to do so often remains uncertain to the general population. The paper analyses the effects of the ketogenic diet for fat loss as well as treating mental illnesses and aims to address the influence of high carbohydrate diets on mental illnesses.
Author Contributions
Academic Editor: Sasho Stoleski, Institute of Occupational Health of R. Macedonia, WHO CC and Ga2len CC, Macedonia.
Checked for plagiarism: Yes
Review by: Single-blind
Copyright © 2020 Vaishnavi Nashte, et al.
 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Competing interests
The authors have no conflicts of interest to declare.
Citation:
Introduction
It has been observed over the years that the rate of obesity has been increasing at an alarming rate. With an easier transition towards sedentary lifestyle and junk food, the Covid-19 lockdown has resulted in imbalanced diets, sleep and physical exercises. This has adversely affected weight regulation. Nutrition and diet have become as important as the lockdown isolation for the overweight and obese individuals during the pandemic as significant increase in BMI (body-mass index) also leads to reduced immunity. Obesity is defined as having a high BMI. For adults, W.H.O. (World Health Organization) classifies overweight as a BMI greater than or equal to 25; and obesity is a BMI greater than or equal to 30. According to “Our World in Data”, along with heart disease, strokes, diabetes and cancer, obesity is one of the leading causes of death. 1 It has been seen that obesity cases do not directly cause the aforementioned diseases but they are a significant risk contributor in their occurrence.
Exercise and nutrition is not important to simply maintain physical health but also mental health. But what kind of diet will help in doing so? Diets have evolved over time because of factors such as changes in food availability, food prices, and level of income. A hunter gatherer diet, that is high in fat and protein and consisted of whole foods and animal meat, has now been replaced with food high in sugar, starch and processed grains. This major transition towards different macronutrients has affected our mental and physical health. In order to understand these effects, we shall compare diets high in carbohydrates with diets high in fat and evaluate the long term effects of diets high in carbohydrates.
Dietary Patterns in Last 50 Years
The leading causes of death in the 20th century were majorly infectious agents, but today, due to the lifestyle factors and dietary patterns, caused by diseases of civilization such as diabetes, obesity, cardiovascular diseases and cancer. In fact, these diseases have become the major cause of death in the 21st century. 2 Increasing numbers of evidence suggest the link between the prevailing dietary habits with the risk of developing various diseases of civilization. Today, identifying certain dietary components that help in the prevention of these diseases is a major global concern. The investigative studies conducted in the USA, Canada and Western Europe found the association of prevailing dietary patterns with a number of chronic diseases. The 1970's marked a transition towards processed food, cheap edible oils and sugar sweetened beverages. Furthermore, the 1990’s marked a transition towards decreased physical activity and eventually adopting the sedentary lifestyle. These changes in lifestyle weren’t given any attention until diabetes, hypertension, depression and the other diseases of civilization started dominating the world.
The domestication of agriculture was easily adopted worldwide because of the huge harvests and cheap prices. It brought along with it a plethora of issues such as slipped disks, arthritis, hernias, obesity and other diseases which were virtually absent in the hunter gatherers or even the non-westernised population. Before the agricultural revolution, grains made up only a small fraction of our diet. Today, our diet that comprises majorly cereals, lacks in vitamins and minerals.
The transition to a Western diet has led to a drastic increase in insulin resistance (defined as an impaired ability of the hormone to suppress the glucose output), as well as obesity, hypertension, cancer and other critical diseases. On the other hand, studies show that a traditional Palaeolithic diet consisting of higher fat and protein content was associated with significant improvement in insulin resistance, fasting insulin levels and glucose control. 3, 4, 5
Processed food and prepared meals have become increasingly common because most of us are eating away from home. Fast food, in particular, has now become a major part of our lives resulting in alarming concern for various health conditions related to obesity. Our body composition has seen dramatic changes due to the dietary patterns across the globe. Also, technological advancement has reduced our energy expenditure at work even more. Easy transportation has resulted in more leisure time and reduced physical activity.
An NCBI paper 6 studied 229 hunter gatherer diets from around the world and found that they were higher in fat and protein and lower in carbohydrates. Protein contributed to 19–35% of the total energy and carbohydrates contributed 22–40% by whereas the fat contributed to 28–58%. Ancestral diets consisted majorly of fish and uncultivated plant based foods. Cereals and refined sugars were not a part of it. The carbohydrates consumed during the Palaeolithic Era were low glycemic, indicating a lower insulin response, just like fat and proteins. Our Nutrition saw some significant changes after the agricultural revolution about 10,000 years ago and the industrial revolution about 250 years ago. The western diets are dominated by high glycemic carbohydrates such as refined cereals and starchy food products. The glucose derived in huge amounts from these sources has become the most important source of energy for the human body and contributes to almost 40-75% of the energy intake. While human nutrition has changed post the industrial and agricultural revolution, the human genome has remained largely unchanged. Changes in diet and lifestyle occurred too fast for the human genome to adapt to; therefore, humans are still biologically adapted to the environment of their pre-agricultural ancestors. 7
Our physiology today is the result of overeating, frequent snacking and over consumption of high sucrose soft drinks. Sugar gets easily consumed in large quantities via beverages, sweets, addictive bakeries and ready to go meals. As a result, these high glucose meals contribute to an elevated insulin level throughout the day. Foods with a high insulin response are palatable, produce more appetite and are less satiating. Therefore, high-insulin producing Western Diets lead to increased food intake and overeating. In addition, the energy density of food has a major impact on the regulation of food intake and body weight. Calories from fluids are less satiating than those from solid foods and often lead to overconsumption. 8
Dietary Patterns Associated with Mental Illnesses
According to W.H.O, in Europe, sugar intake in adults ranges from about 7-8% of total energy to about 16-17% in countries like Spain and the United Kingdom. Intake is much higher among children, ranging from about 12% in countries like Denmark, Slovenia and Sweden, to nearly 25% in Portugal. Sugar intake also varies with geographic locations. Intake in rural communities in South Africa is 7.5% while that in urban communities is 10.3%.The latest sugar intake guidelines by WHO recommends adults and children to reduce their daily sugar intake to less than 10% of the total energy. Dr Francesco Branca, Director of WHO’s Department of Nutrition for Health and Development says, “We have solid evidence that keeping intake of free sugars to less than 10% of total energy intake reduces the risk of overweight, obesity and tooth decay. Making policy changes to support this will be important if countries are to live up to their commitments to reduce the burden of non-communicable diseases.”11
In fact a study published in BMC Public Health, found that compared to normal-weight individuals, overweight or obese individuals reported psychosocial problems and suicidal thoughts more often. 11 The human brain uses more energy than any other organ in the body and chooses glucose or Ketones as its primary source of fuel. Western diets expose the human brain to an excessive amount of sugar and high amounts of glucose, which is harmful to the brain. Along with worsening the regulation of insulin in our body, they also promote inflammation and oxidative stress. Number of studies suggests the prevailing correlation between high glucose diets with impaired brain function, diabetes and even worsening of mood disorders such as depression. According to Joseph C. Masdeu (MD, PhD, of the Houston Methodist Neurological Institute), “With diabetes, you have an increased risk of damage to blood vessels over time, including damage to the small blood vessels in the brain”. According to a recent study in neurology, if your blood sugar is on the high end of the normal range, diabetes isn’t the only risk. It also increases the risk of brain shrinkage in areas associated with memory and thinking. Past researches have also supported the link between type2 diabetes and brain shrinkage. 12
High glucose level in the blood is one of the predisposing factors of Alzheimer’s, which is known to cause mental dysfunctions. In fact, in recent years, Alzheimer’s is occasionally referred to as “type 3” diabetes. This is because both Alzheimer’s and “type 3” diabetes are caused due to abnormal levels of insulin. Alzheimer’s is another potential side effect of our widely adopted Western Diets. A study, published in the journal “Diabetologia”, followed 5,189 people over the course of 10 years and concluded that people with high blood sugar levels had a faster rate of cognitive decline than those with normal blood sugar levels.
Consistently having high blood sugar levels can cause diabetes which indirectly affects our brain. In fact, numerous researches have consistently highlighted the link between diabetes and dementia for decades. According to a review published in Experimental Gerontology, having diabetes doubles the risk of developing dementia and scientists are discovering that even slightly elevated levels of blood sugar can speed up cognitive decline. In a study conducted in 2012, about 1000 people were categorised into four groups based upon the proportion of carbohydrates in their diet. It was found that the group consuming the most amounts of carbohydrates, were 80% more prone to developing mild cognitive impairment (which is a pit stop on the way to dementia). High blood glucose levels can have other effects like Insomnia, sugar addiction and effects on mood.
A recent study gathered data from 50,000 women in order to investigate whether high blood sugar levels lead to the development of Insomnia. The research concluded that individuals consuming diets with high levels of sugar and processed grains had a greater risk of developing insomnia. 12 Moreover, studies conducted on brain activity provide evidence that overeating alters the brain’s reward system which further drives overeating and thus forming a cyclic reaction. A study found that sweet foods can be more addictive than cocaine. Even though the research was performed on animals, they found that intense sweetness can surpass cocaine reward, even in drug-sensitized and addicted individuals.
Studies have reported that individuals with acute hyperglycemia (elevated blood sugar) have increased levels of negative emotions such as sadness and anxiety. A study conducted on dietary consumption and mood of 23,245 individuals found that higher rates of sugar consumption were associated with greater incidence of depression. A study published in 2017 in the journal Scientific Reports, found that those with the highest level of sugar consumption were 23% more likely to be diagnosed with a mental disorder than those with the lowest sugar intake.13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24
Unhealthy dietary patterns causing obesity has now become more common as compared to undernutrition 24. The obesity rates have skyrocketed by 185% in the last 50 years. According to the W.H.O, worldwide obesity has nearly tripled since 1975. In fact in 2016 more than 1.9 billion adults aged 18 and older were overweight and out of all these about 650 million were obese. According to a study conducted by the Global Burden of disease in 2017, obesity has accounted for a total of 4.72 million deaths worldwide. In 2017, globally 8% of the deaths were due to obesity. This has represented a 50% increase from the 1990s when obesity accounted for 4.5 million deaths. Across many middle income countries such as Eastern Europe, Central Asia, North Africa and Latin America, more than 15% of deaths in 2017 were due to high obesity. Aside from the prevalence of deaths due to overweight and obesity, deaths have also resulted due to poorer overall health. For high income countries, obesity related deaths fall in the range of 8% to 10%. Globally, the death rate from obesity in 2017 was around 60 per 100,000 people. The comparison of death rates and number of people with prevailing obesity conditions show that death rates tend to be high in countries where more people have obesity. According to W.H.O reports, the share of overweight or obese children and adolescents aged 5-19 has jumped from 4% in 1975 to around 18% in 2016, an alarming increase of 400%. 24 According to the Centres of Disease Control and Prevention, the estimated annual medical cost of obesity in the United States was $147 billion in 2008 US dollars; the annual medical cost for people who have obesity was $1,429 higher than healthy individuals. Obesity is a common and a costly disease that needs to be taken seriously. A significant raise in BMI has proven to be a major risk factor to the growth of diseases such as cardiovascular diseases. Globally in 2012, cardiovascular diseases were the leading causes of death. Amongst these were mainly heart diseases and strokes. A rise in BMI also leads to the growth of musculoskeletal disorders, especially osteoarthritis which is a high disabling disease of the joints. It also gives rise to various types of cancers such as endometrial, breast cancer, ovarian, prostate, liver, gallbladder, kidney, and colon. Talking about childhood obesity, the 2019 data from Work Health Organisation suggests that children under the age of 5 years were overweight or obese. Obesity used to be an issue of the high income countries but it has now skyrocketed in the low and middle income countries, especially in the urban areas. The number of obese children in Africa under the age of 5 has increased by nearly 24% since 2000. Almost half of the children under the age of 5 who were overweight or obese in 2019 lived in Asia. Obese children also experience breathing difficulties, increased risk of fractures, hypertension, and an early presence of cardiovascular diseases, insulin resistance and psychological effects. It is proved to be a significant risk contributor to the growth of mental illnesses. The co-existence of obesity and mental health can create a negative spiral effect for any individual. Issues such as depression and low self esteem have now been observed in obese individuals around the world even when there was no previous history of mental illnesses. Studies conducted at the Texas Health Science Centre and by the UK’s National Obesity Observatory (NOO) and many other such researches confirm that the obese are at greater risk of depression. 25
Lifestyle Factors
Alongside dietary patterns, a variety of lifestyle factors have contributed to disease development including smoking, alcohol overuse, drug abuse, physical inactivity and chronic stress. Cigarette smoking can cause or contribute to the development of a range of potentially fatal and disabling diseases and conditions including several types of cancer, cardiovascular diseases and chronic obstructive pulmonary disease. Intriguingly, smoking causes insulin resistance, activation of the Sympathetic Nervous System and low-grade inflammation, all of which have been implicated in the development of civilization diseases, as pointed out above.
Heavy alcohol consumption is a critical risk factor for various health challenges that eventually contribute to the global burden of disease. It can contribute to categories of illnesses like infectious diseases, cancer, diabetes, neuropsychiatric disorders (including alcohol use disorders) and cardiovascular diseases. According to a study by the Centre for Addiction and Mental Health, about 40% of the world’s adult population consumes alcohol, and the average consumption per drinker is 17.1 litres per year.
The Relationship Between Obesity and Covid-19
Affecting the globe’s most vulnerable population bit by bit, the COVID-19 pandemic has become a global crisis. Studies suggest that in many countries, the most vulnerable ones are also at a higher risk of obesity. Due to the current pandemic, the need for self isolation is making individuals rely more upon processed food choices and canned food products 26. This has resulted in an increase in weight over time. For individuals who are COVID-19 positive, there appears to be a strong relationship between overweight and obesity with the risks of hospitalisation. It has also been observed that adults under 60 who are obese are more likely to be hospitalised.
The pandemic has occurred at a time when cases of obesity and overweight are increasing globally. 27 Comparing the obesity prevalence in the top 20 ranked countries of total deaths due to COVID-19, the data from global health services of the World Health Organization states that The United States of America is ranked first in terms of obesity prevalence (36.2%) and overweight prevalence (31.7%). Overall, most of the countries had prevalence between 20% and 30% (e.g., UK, Canada, Iran, Mexico, and Chile). 28 Analysing the correlation between obesity and total number of deaths due to COVID-19, it was observed that the total number of deaths significantly correlated with obesity existence. The number of deaths was directly proportional to the average obesity count of the population. Obesity-related conditions such as cardiovascular and metabolic effects, sleep apnea, vitamin D deficiency, and many others seemed to worsen the effect of COVID-19. 29
The Italian National Institute of Health (Instituto Superiore di Sanità) launched a surveillance system in order to collect data on Covid-19 positive individuals throughout the country. The system captured all Covid-19 cases data from 19 Italian regions and 2 autonomous provinces of Trento and Bozen 30. The report indicates that 99% of deaths occurred in patients with pre existing diseases, such as obesity, hypertension, type 2 diabetes mellitus, heart disease, kidney damage, and cancer 31. As of April 2020, 145 of the 12,250 (1.2%) COVID‐19–positive patients under the age of 50 have died. For 14 patients under the age of 40 years, no clinical information is available; the remaining 18 had serious pre existing pathologies, such as severe obesity and its comorbidities (cardiovascular, renal, diabetes mellitus, and psychiatric pathologies), and 3 had no major pathologies 32.
Why the High Risk for Obese Individuals?
An obese individual has numerous underlying risk factors for COVID‐19. It also increases the likelihood of obesity being the independent contributing factor to Covid-19. 33 Considering OSA (Obstructive sleep apnea), a sleep related disorder. It causes hypoxia (absence of enough oxygen in the tissues to sustain bodily functions) and apnea/ hypopnea. Obesity is a predominant risk factor for OSA and these patients may be vulnerable to COVID-19. 34
Sleep efficacy is considered as an important factor for the regulation and maintenance of the immune system. During sleep, the immune system releases certain proteins called cytokines which help in promoting sleep. Certain cytokines increase during an infection or inflammation, or when under stress. Sleep deprivation decreases the production of these protective cytokines, whereas damaged sleep efficacy is associated with decreased immune system activity. Another factor of Vitamin D deficiency which is very common in obese individuals has unfavourable impacts on several systems in our body. Vitamin D deficiency worsens obesity by enhancing lipogenesis (formation of fat) 35. Obesity-related conditions worsen the effect of COVID-19. The Centre for Disease Control and Prevention (CDC) reported that people with heart disease and diabetes are at higher risk of COVID-19 complications. 36
The negative influence of obesity isn’t limited to contributing to Covid-19 cases but similar infectious diseases in the future. A research looked at adults aged 18 to 64 and found that morbid obesity rates are positively correlated with COVID-19 case and death rates, and that morbid obesity rates can explain 9 percent of the variation in COVID-19 death rates. After overlaying the data geographically the researchers found that spatial clusters of high rates of morbid obesity are associated with spatial clusters of high rates of COVID-19 deaths.37 Therefore, fighting against Covid-19 on the basis of obesity should include approaches like weight loss programs, vitamin D supplementation, management of OSA being a few.
What Diet Works Best for Fat Loss and Neurodegenerative Disorders?
Various health care organisations have constantly bombarded the importance of weight control and adopting a healthy lifestyle. But this often fails due to a number of factors such as genetic predisposition of adipose along with having a sedentary lifestyle and high intake of processed high carbohydrate foods.38 In the past years, there have been many strategies that have focused solely upon reducing energy or calorie intakes by different diets, drugs and even bariatric surgery. 39 Even though there has been a general agreement regarding changing the calorie intake and physical activity levels, the process to achieve better dietary patterns and lifestyle has still been unclear. For many years, nutritional studies have been focused on reducing dietary fat. This not only had extremely small positive effects but also scared off the normal population of people habituated to consuming dietary fat over the years. In recent years, the ketogenic diet has received a lot of attention for treating obesity. In fact, many studies have also shown that this kind of nutritional approach has a solid physiological and biochemical basis and is able to induce effective weight loss along with improvement in several cardiovascular risk parameters. Ketogenic diets, consisting of very low intake of carbohydrates, started getting adopted as a weight loss strategy from 1972. 40 Our food consists of three macronutrients—carbohydrates (4 kcal/gm), fat (9 kcal/gm), and protein (4 kcal/gm). Analysing low carbohydrate diets, we can categorise them into low-carbohydrate (< 10% carbohydrates) or 20-50 gm/day, Low-carbohydrate (<26% carbohydrates) or less than < 130 gm/day, Moderate-carbohydrate (26%-44%), High-carbohydrate (45% or greater) 41
A study was conducted on 83 obese patients (39 men and 44 women) who had a BMI greater that 35 kg/m2in determined the effects of a very low carbohydrate diet consisting of 30gms per day, 1 g/kg body weight protein, 20% saturated fat, and 80% polyunsaturated and monounsaturated fat in obese patients. The individuals selected also suffered from high glucose and high cholesterol levels. The body weight, body mass index, total cholesterol, triglycerides, fasting blood sugar, urea and creatinine levels were determined before and after the administration of the ketogenic diet. Changes were monitored after 8, 16 and 24 weeks. The results showed a significant decrease in the weight and BMI of the obese patients. Their cholesterol levels also decreased in the duration of the study. HDL cholesterol levels significantly increased, whereas LDL cholesterol levels significantly decreased after treatment. The level of triglycerides decreased significantly following 24 weeks of treatment. The level of blood glucose significantly decreased. The initial weight of the subjects was around 101.03±2.33 kg and it was seen to drop significantly during the course of 24 weeks. The body weights at the 8th, 16th and 24th week were 91.10±2.76 kg, 89.39±3.4 kg and 86.67±3.70 kg, respectively (Figure 1). Similarly changes in BMI were observed from the initial BMI until the 24th week. The reduction noted in the 8th, 16th and 24th week was 37.77±0.79 kg/m2, 33.90±0.83 kg/m2, 33.24±1.00 kg/m2 and 32.06±1.13 kg/m2, respectively (Figure 2). 42, Figure 3, Figure 4.
Figure 1.Reduction in body weight at 8, 16 and 24 weeks following the administration of the ketogenic diet in obese patients. 
Figure 2.Decrease in body mass index at eight, 16 and 24 weeks during the administration of a ketogenic diet in obese patients.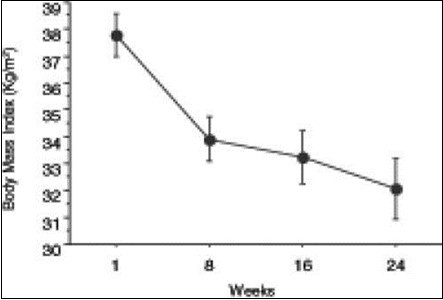
Figure 3.Global Health estimates 2016: Deaths by cause, age, sex by country and by region.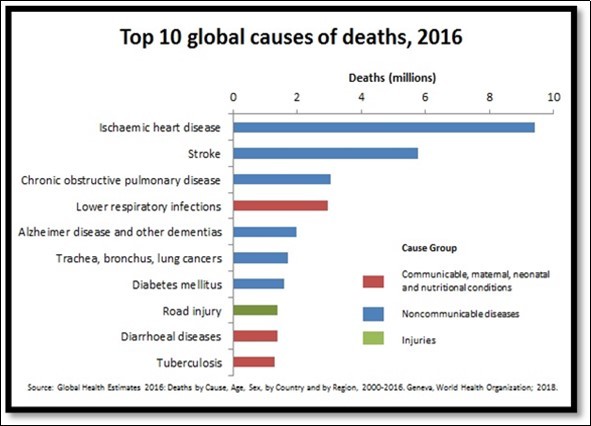
Figure 4.Increase in refined sugar consumption from 1970 to 2000.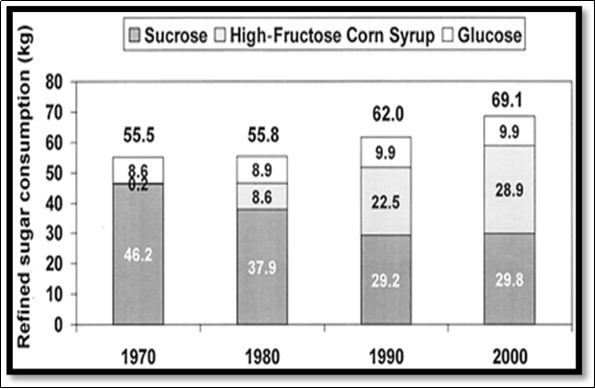
The entire study of low carbohydrate diets have been focused not just on weight loss for the obese and overweight but also for patients at risk of diseases such as type 2 diabetes and non-alcoholic fatty liver disease. They’re also used as treatment for seizure disorders as well as an alternative fuel for the athletes encouraging better performance and health. For patients with type 2 diabetes, before medications, controlling the carbohydrate intake has been essential in glycemic control for both type 1 and type 2 diabetes. Dietary carbohydrates increase insulin needs, and reduction of carbohydrate intake can improve glycemic control. 43 A recent study demonstrated a significant reduction of insulin and oral medications and hemoglobin A1C reduction with ketogenic approaches while demonstrating a high adherence to the intervention at 12 months.44 Approaches to nutritional lifestyle approaches to diabetes (medical nutrition therapy) have included low carbohydrate as an option in recent guidelines.45 Studies have demonstrated a consistent benefit in glycemic control, weight loss, and sustained medication reduction using a very low carbohydrate approach (< 14% of energy from carbohydrates).46 Current advancements in the nutritional research have accounted to public awareness about the positive effects of the low carbohydrate and high fat diet. In humans, ketone bodies are the only additional source of brain energy after glucose and the generation of ketone bodies during fasting is essential to prevent the destruction of muscle from glucose synthesis. 47, 48 It was shown that a ketogenic diet could act as a mood stabilizer in bipolar illness 49. Beneficial changes in the brain energy profile have been observed in subjects who are on a ketogenic diet 50. This is a significant observation because cerebral hypometabolism is a characteristic feature of those who suffer from depression or mania 51. In another study 52, it was shown that a ketogenic diet induced gene expression in the brain. These studies provide evidence to explain the actions of a ketogenic diet in the brain. The treatment of epilepsy by using a ketogenic approach may be related to increased availability of beta-hydroxybutyrate, a ketone body readily transported through the blood-brain barrier. 53.
It has been found that a sugary diet is the root cause of various chronic diseases of the body. A recent study 54 showed that sugar can accelerate aging. Several recent studies 55,56 have pointed to the fact that a diet with a high glycemic load is independently associated with the development of cardiovascular diseases, type II diabetes and certain forms of cancer. Glycemic load refers to a diet of different foods that have a high glycemic index. Glycemic index is a measure of the elevation of glucose levels following the ingestion of a carbohydrate. The classification of a carbohydrate based on its glycemic index provided a better predictor of risk for coronary artery diseases than the traditional method of classification of carbohydrate into simple or complex forms 57. It has also been found that sugary drinks decreased blood levels of vitamin E, thus reducing the amount of antioxidants in the body. It has been proven, beyond a doubt, that disrupting the oxidant-antioxidant status of the cell will lead to various diseases of the body 58.Studies have suggested that very low fat diets are considered to be low in calcium content. Women on low fat diets excrete most of the calcium they consume; therefore, they are more prone to osteoporosis. However, a high fat diet can rectify this situation 59.
Several studies 60,61 with appropriate control groups that compared the effect of a low fat diet with a low carbohydrate ketogenic diet 62 showed that obese women on a low carbohydrate ketogenic diet lost 8.5 kg in six months as compared to 4.2 kg lost by those in the low fat diet group. Twenty-two subjects from the low carbohydrate ketogenic diet and 20 subjects from the low fat diet completed the study, with both groups reducing their energy intake by approximately 450 kcal from the baseline level. In another study performed in 132 severely obese subjects for six months 63, there was greater weight loss in the low carbohydrate ketogenic diet group than in the low fat diet group (5.8 kg versus 1.9 kg).
Effects of Kd on Mental Disorders
15 studies were conducted in order to test the effect of the ketogenic diet on mental disorders such as anxiety, depression, bipolar disorder, schizophrenia, autism spectrum disorder (ASD), and attention deficit hyperactivity disorder (ADHD). Anxiety in humans is associated with the activation in the ventromedial prefrontal cortex and hippocampal regions of the brain 64. Symptoms of anxiety and disorders are more frequent in patients with epilepsy with one recent study reporting a lifetime incidence of 22.8% as opposed to 11.2% in people without epilepsy 65. The study conducted for anxiety on male rats consisted of administering exogenous ketone supplement which led to significantly elevated levels of beta-hydroxybutyrate indicating ketosis. The treatment conditions resulted in reduced anxiety that was assessed by behaviour.
Studies have suggested the association between depression and epilepsy 66. After examining the antidepressant properties of KD on 20 rats, they found out that the rats on HFLC (High fat low carbohydrate) diets spent less time immobile than control rats that were fed a standard diet. This provided some evidence stating the potential antidepressant effects of the diet. The diet duration was 7 days, and levels of beta-hydroxybutyrate were measured. 67
A study of nutrition and exercise behaviour conducted on patients with schizophrenia andbipolar disorders found that the latter reported risk factors related to poor nutrition 68. A study conducted on two women with bipolar disease type II maintained a KD diet for 2 and 3 years respectively and they reported mood stabilization which exceeded that of medication as well as an overall improvement in their condition. 70. The ratio of KD was estimated to be around 70% fat, 22% protein, and 8% carbohydrates. Considering the case of Schizophrenia which is associated with high levels of morbidity, a drug induced study was conducted on mice which demonstrated that 3 weeks of KD (77.6% fat) normalised pathological behaviours 71. These included psychomotor hyperactivity, stereotyped behavior, social withdrawal, and working memory deficits, which reflect the positive, negative, and cognitive symptoms of the disorder. Weight loss was an observed side effect. Elevated levels of the ketone beta-hydroxybutyrate and decreased glucose levels indicated that metabolic adaptation had occurred. 72
Patients with ASD (Autism Spectrum Disorder) have compromised social interaction and communication 73. It has also been studied that between 5 and 40% of patients with autism will develop epilepsy 74 Effects of KD were examined on mice and the other group was fed a standard diet. After 70 days on KD, a statistically significant result was found in mice with behaviours such as social deficits and stereotypes that are common behaviours in those with ASD 75. It is also believed that mitochondrial dysfunction may play a role in the onset of ASD 76, 77 It was aimed to determine if KD could reverse the social deficits and mitochondrial dysfunction seen in an animal model of autism using rats. On day 21, rats were placed on either KD (6:1 lipid:non-lipid ratio) or standard diet for 10–14 days. Beta-hydroxybutyrate was measured. KD had a significant effect and was able to modify complex social behaviours in VPA and control rats and mitochondrial respiration 78. The role of KD in ASD has been examined in a pilot study of 30 children 79. The diet (30% of energy as MCT oil, 30% fresh cream, 11% as saturated fat, 19% carbohydrates, and 10% as protein) was administered for 6 months with intervals of 4 weeks with 2 diet-free weeks. Of the total sample, 40% did not comply or did not tolerate the diet. Urinary ketones were measured. In the remaining sample, two children showed significant improvements on the Childhood Autism Rating Scale, while the rest showed mild-to-moderate improvements. As observed in patients with epilepsy, after the termination of KD the benefits persisted, which raise intriguing questions regarding the effects of plasticity. The suggested mechanisms of action of KD in ASD include that it may reduce pain sensitivity through the reduction of glucose and may have anti-inflammatory properties as it reduces swelling and plasma extravasation 80. In a systematic review of KD in ASD it was concluded that the limited number of reports of improvements after treatment with the diet is not sufficient to attest to the practicability of KD as a treatment for the disorder 81. Attention deficit hyperactivity disorder is characterized by a lack of behavioural inhibition and by neuropsychological deficits in four areas, including working memory, self-regulation of affect–motivation–arousal, internalization of speech, and behavioral analysis and synthesis 82. ADHD is the most commonly occurring mental disorder in children and adolescents with epilepsy occurring in 16 (29.1%) of 78 patients 83. Children with ADHD have a high frequency of epileptiform discharges as observed by EEG 84. In a prospective study of children with epilepsy (n = 34) on KD it was found that after 1 year on the diet there was a statistically significant improvement of attention and social functioning 85.
Conclusion
Evidence shows the significant relation between our dietary patterns and the resulting rates of obesity that give rise to a plethora of diseases. Since the adoption of Western high carbohydrate, we have seen a tremendous rise in diseases of civilization. In the years to come, the situation can get worse if not addressed properly. Weight loss programs should be taken seriously in order to maintain mental and physical health. While addressing we know that nutritional studies in the past have avoided dietary fat. But evidence proves the benefits of a High Fat Ketogenic diet for fat loss and treating Neurodegenerative disorders and its long term benefits in Psychiatry. In short, this paper highlights the importance of treating fat loss and mental health issues in the most beneficial way.
Declarations
Ethics approval and consent to participate: Not Applicable as this is a review paper based on other published Researches.
Consent for Publication
Not Applicable as this is a review paper based on other published Researches.
Availability of data and Materials
The data generated and analysed during the current study are available in the section of references. All data generated or analysed during this study are included in this published article (and its supplementary information files).
Funding
Not Applicable as this is a review paper based on other published Researches.
Authors' Contributions
All authors contributed towards the analysis of the various research papers. All authors read and approved the final manuscript.
Authors' Information
Vaishnavi Nashte
Sports Nutrition at K11 Academy of Fitness Sciences
3rd Year, BAJMC at MITWPU
Phone Number: +91 8689508948
Email Id: [email protected]
Rutuja Shinde
2nd Year, Physiotherapy at Modern College of Physiotherapy
Phone Number: +91 7040212741
Email Id: [email protected]
Acknowledgements
Sumedha Nashte and Vivek Singh for reviewing and revising the paper.
References
- 3.Cordain Loren, S Boyd Eaton, Sebastian Anthony, Mann Neil.Staffan Lindeberg, Bruce A Watkins, James H O’Keefe, Janette Brand-Miller (2005),The American Journal of ClinicalNutrition,Origins and evolution of the Western diet: health implications for the 21st century.
- 4.Lindeberg S, Eliasson M, Lindahl B, B.Ahrén(1999), National Library of Medicine, Low serum insulin in traditional Pacific Islanders--the Kitava Study.
- 5.S B Eaton, Konner M, Shostak M. (1988) National Library of Medicine, Stone agers in the fast lane: chronic degenerative diseases in evolutionary perspective.
- 6.Ströhle Alexander.Andreas Hahn (2011), National Library of Medicine, Diets of modern hunter-gatherers vary substantially in their carbohydrate content depending on ecoenvironments: results from an ethnographic analysis.
- 7.Luca F, G H Perry, A Di Rienzo. US National Library of Medicine National Institutes of Health,Evolutionary Adaptationsto Dietary Changes (2014) .
- 8.Wolfgang Kopp.(2019).US National Library of Medicine National Institutes of Health, How Western Diet And Lifestyle Drive The Pandemic Of Obesity And Civilization Diseases.
- 10.Vuuren C L van, G, Veenstra R. (2019) Associations between overweight and mental health problems among adolescents, and the mediating role of victimization. , BMC Public Health 19, 612.
- 11.Vuuren C L van, G, Veenstra R. (2019) Associations between overweight and mental health problems among adolescents, and the mediating role of victimization. , BMC Public Health 19, 612.
- 12.Even in normal range, high blood sugar linked to brain shrinkage, (2012), Science Daily, People whose blood sugar is on the high end of the normal range may be at greater risk of brain shrinkage that occurs with aging and diseases such as dementia, according to new research.
- 13.Rosebud O Roberts. (2013) US National Library of MedicineNational Institutes of Health, Relative Intake of Macronutrients Impacts Risk of Mild Cognitive Impairment or dementia.
- 16.W H O.Press release (2015) WHO calls on countries to reduce sugars intake among adults and children.
- 17.Daily Science. (2019) Refined carbs may trigger insomnia, finds study, Women who consumed a diet high in added sugars and refined carbohydrates had a greater risk of developing insomnia, a new study has found.
- 18.KHAZAN OLGA.(2018),The Atlantic The Startling Link Between Sugar and Alzheimer's A high-carb diet, and the attendant high blood sugar, are associated with cognitive decline.
- 19.Clara R Freeman1. (2018) Amna Zehra1, Veronica Ramirez1, Corinde E Wiers1, Nora D Volkow1,2, Gene-Jack Wang.
- 20.Barry M Popkin, Linda S Adair, Shu Wen Ng. (2013) . US National Library of Medicine National Institutes of Health, NOW AND THEN: The Global Nutrition Transition:The Pandemic of Obesity in Developing Countries .
- 24.Vuuren C L van, G, Veenstra R. (2019) Associations between overweight and mental health problems among adolescents, and the mediating role of victimization. , BMC Public Health 19, 612.
- 26.Obesity World.Prevalance of obesity, The epidemic of obesity is now recognised as one of the most important public health problems facing the world today. Adult obesity is more common globally than under-nutrition.
- 29.Obesity World.Corona Virus (Covid-19) and obesity, Obesity-related conditions seem to worsen the effect of COVID-19; indeed, the Centers for Disease Control and Prevention (CDC) reported that people with heart disease and diabetes are at higher risk of COVID-19 complications.
- 30.Popkin B M, Du S, Green W D. (2020) Individuals with obesity and COVID‐19: A global perspective on the epidemiology and biological relationships. Obesity Reviews. 1-17.
- 31.W H O.Coronavirus disease (COVID-19) Weekly Epidemiological Update and Weekly Operational Update.
- 32.Ekiz Timur. (2020) and Ahmet Cemal Pazarlı. Relationship between COVID-19 and obesity.” Diabetes & metabolic syndrome 14, 761-763.
- 33.A E Malavazos, Romanelli Corsi, M, F, Iacobellis G. (2020) Targeting the Adipose Tissue in COVID‐19. , Obesity 28, 1178-1179.
- 34.A E Malavazos, Romanelli Corsi, M, F, Iacobellis G. (2020) Targeting the Adipose Tissue in COVID‐19. , Obesity 28, 1178-1179.
- 35.Popkin B M, Du S, Green W D. (2020) Individuals with obesity and COVID‐19: A global perspective on the epidemiology and biological relationships. Obesity Reviews. 1-17.
- 36.Romero-Corral Abel. (2010) Interactions between obesity and obstructive sleep apnea: implications for treatment. , Chest 137(3), 711-9.
- 37.Ekiz Timur.Ahmet Cemal Pazarlı,Relationship between. COVID-19 and obesity,Diabetes & Metabolic Syndrome: Clinical Research & Reviews,Volume 14, Issue 5-2020.
- 38.Obesity World.Coronavirus (COVID-19) & Obesity, Obesity-related conditions seem to worsen the effect of COVID-19; indeed, the Centers for Disease Control and Prevention (CDC) reported that people with heart disease and diabetes are at higher risk of COVID-19 complications.
- 39.Daily Science. (2020) Relationship between COVID-19 deaths and morbid obesity, The prevalence of morbid obesity in a population is associated with negative outcomes from COVID-19, according to a new analysis of morbid obesity data and reported COVID-19 deaths in the United States.
- 40.Paoli Antonio. (2014) Ketogenic diet for obesity: friend or foe?.” International journal of environmental research and public health vol. 11, 2092-107.
- 41.Paoli Antonio. (2014) Ketogenic diet for obesity: friend or foe?.” International journal of environmental research and public health. 11(2), 2092-107.
- 42.Oh R, Gilani B, Uppaluri K R. (2020) Low Carbohydrate Diet. In: StatPearls [Internet]. Treasure Island (FL):StatPearlsPublishing.
- 43.Hussein M Dashti. (2004) Long-term effects of a ketogenic diet in obese patients.” Experimental and clinical cardiology vol. 9(3), 200-205.
- 44.Oh R, Gilani B, Uppaluri K R. (2020) Low Carbohydrate Diet. [Updated. Available from: https://www.ncbi.nlm.nih.gov/books/NBK537084/
- 45.Hussein M Dashti. (2004) Long-term effects of a ketogenic diet in obese patients.” Experimental and clinical cardiology vol. 9(3), 200-205.
- 46.Hussein M Dashti. (2004) Long-term effects of a ketogenic diet in obese patients.” Experimental and clinical cardiology vol. 9(3), 200-205.
- 47.Bostock Emmanuelle C S. (2017) . The Current Status of the Ketogenic Diet in Psychiatry.” Frontiers in psychiatry 8, 43-20.
- 48. (1999) Essential fatty acids are mediators of brain biochemistry and cognitive functions.Yehuda S. , Rabinovitz S, Mostofsky DI J Neurosci Res 56(6), 565-70.
- 49. (2001) The ketogenic diet may have mood-stabilizing properties. El-Mallakh RS, Paskitti ME Med Hypotheses. 57(6), 724-6.
- 50. (2001) The ketogenic diet may have mood-stabilizing properties. El-Mallakh RS, Paskitti ME Med Hypotheses. 57(6), 724-6.
- 51. (2001) The ketogenic diet may have mood-stabilizing properties. El-Mallakh RS, Paskitti ME Med Hypotheses. 57(6), 724-6.
- 52.DA Sato H Epilepsy Res. (2002) The ketogenic diet upregulates expression of the gene encoding the key ketogenic enzyme mitochondrial 3-hydroxy-3-methylglutaryl-CoA synthase in rat brain. Cullingford TE,Eagles. 49(2), 99-107.
- 53.barrier Blood-brain. (1999) ion homeostatis and epilepsy: possible implications towards the understanding of ketogenic diet mechanisms. Janigro D. Epilepsy Res. 37(3), 223-32.
- 54.Petersen K F, Befroy D, Dufour S, Dziura J, Ariyan C et al. (2003) Mitochondrial dysfunction in the elderly: possible role in insulin resistance. , Science. May 300(5622), 1140-2.
- 55.Holt SH K, Brand-Miller J C, Nutr Am J Clin. (2002) International table of glycemic index and glycemic load values:. Foster-Powell 76(1), 5-56.
- 57.Liu S, Willett W C, Stampfer M J, Hu F B, Franz M et al. (2000) A prospective study of dietary glycemic load, carbohydrate intake, and risk of coronary heart disease in. 71(6), 1455-61.
- 58.W P Hamouda, Garg R, Aljada A, Ghanim H, P J Dandona. (2000) Glucose challenge stimulates reactive oxygen species (ROS) generation by leucocytes. Mohanty. 85(8), 2970-3.
- 59.Cauley J A, Baker C E, Ferrell R E, Charron M, Caggiula A W et al. (2000) Factors associated with calcium absorption efficiency in pre- and perimenopausal women. Wolf RL. , Am J Clin Nutr. Aug; 72(2), 466-71.
- 60.Brehm B J, Seeley R J, Daniels S R, D'Alessio DA J. (2003) A randomized trial comparing a very low carbohydrate diet and a calorie-restricted low fat diet on body weight and cardiovascular risk factors in healthy. 88(4), 1617-23.
- 61.Iqbal N FF, Seshadri P, Chicano K L, Daily D A, McGrory J et al. (2003) A low-carbohydrate as compared with a low-fat diet in severe obesity. Samaha. 348(21), 2074-81.
- 63.Iqbal N FF, Seshadri P, Chicano K L, Daily D A, McGrory J et al. (2003) A low-carbohydrate as compared with a low-fat diet in severe obesity. Samaha. 348(21), 2074-81.
- 64.Rigoli F, Ewbank M, Dalgleish T, Lett Calder A Neurosci. (2016) Threat visibility modulates the defensive brain circuit underlying fear and. 26, 7-13.
- 67.P B Branski, Palucha A, Pilc A, Bull Nowak G Brain Res. (2001) Antidepressant-like properties of zinc in rodent forced swim test. Kroczka. 55(2), 297-300.
- 68.Kilbourne A M, Rofey D L, McCarthy J F, Post E P, Welsh D et al. (2007) Nutrition and exercise behavior among patients with bipolar disorder. , Bipolar Disord. Aug; 9(5), 443-52.
- 69.Kilbourne A M, Rofey D L, McCarthy J F, Post E P, Welsh D et al. (2007) Nutrition and exercise behavior among patients with bipolar disorder. , Bipolar Disord. Aug; 9(5), 443-52.
- 70.Phelps J R, Siemers S V, El-Mallakh R S. (2013) The ketogenic diet for type II bipolar disorder. Neurocase. 19(5), 423-6.
- 71.Phelps J R, Siemers S V, El-Mallakh R S. (2013) The ketogenic diet for type II bipolar disorder. Neurocase. 19(5), 423-6.
- 72.Phelps J R, Siemers S V, El-Mallakh R S. (2013) The ketogenic diet for type II bipolar disorder. Neurocase. 19(5), 423-6.
- 73.S De Rubeis, He X, Goldberg A P, Poultney C S, Samocha K et al.Homozygosity Mapping Collaborative for Autism., UK10K Consortium., Synaptic, transcriptional and chromatin genes disrupted in autism. , Nov 515(7526), 209-15.
- 74. (2016) Autism spectrum disorder and epilepsy: the role of ketogenic diet .Garcia-Penas JJ Rev Neurol. 62(1), 73-8.
- 75.Castro K, Baronio D, Perry I S, RDS Riesgo, Gottfried C. (2016) The effect of ketogenic diet in an animal model of autism induced by prenatal exposure to valproic acid. Nutr Neurosci. 19, 1-8.
- 76.Psychiatry Mol. (2012) Mitochondrial dysfunction in autism spectrum disorders: a systematic review and meta-analysis. 17(3), 290-314.
- 77.Psychiatry Mol. (2012) Mitochondrial dysfunction in autism spectrum disorders: a systematic review and meta-analysis. 17(3), 290-314.
- 78.Ahn Y, Narous M, Tobias R, Rho J M, Mychasiuk R. (2014) The ketogenic diet modifies social and metabolic alterations identified in the prenatal valproic acid model of autism spectrum disorder. Dev Neurosci. 36(5), 371-80.
- 79.Evangeliou A, Vlachonikolis I, Mihailidou H, Spilioti M, Skarpalezou A et al. (2003) Application of a ketogenic diet in children with autistic behavior: pilot study. , J Child Neurol 18(2), 113-8.
- 80.Castro K, Baronio D, Perry I S, RDS Riesgo, Gottfried C. (2016) The effect of ketogenic diet in an animal model of autism induced by prenatal exposure to valproic acid. Nutr Neurosci. 19, 1-8.
- 81.Castro K, Faccioli L S, Baronio D, Gottfried C, Perry I S et al. (2015) Effect of a ketogenic diet on autism spectrum disorder: a systematic review. , Res Autism Spectr Disord 20, 31-38.
- 82.inhibition Behavioral. (1997) sustained attention, and executive functions: constructing a unifying theory of ADHD. Barkley RA. Psychol Bull. 121(1), 65-94.
- 83.Thome-Souza S, Kuczynski E, Assumpção F Jr, Rzezak P, Fuentes D et al. (2004) Which factors may play a pivotal role on determining the type of psychiatric disorder in children and adolescents with epilepsy? Epilepsy Behav. 5(6), 988-94.
