Abstract
Context:
Fine needle aspiration cytology (FNA) is increasingly replacing excisional lymph node biopsy in the assessment of various lymphoid lesions. Recent changes in the classification of non-Hodgkin’s lymphoma, namely the WHO (World Health Organization) Classification of Tumors of Haematopoietic and Lymphoid Tissues has considerably expanded its classification of lymphomas based on the molecular and cytogenetic profiling and immunophenotyping. FNA diagnosis includes varied cytomorphologic diagnostic categories; one of them is the atypical/suspicious.
Objective:
The atypical/suspicious category constitutes about 20 % of all cases studied by FNA cytology. The objective of this study is to determine the definition and the outcome of this unique category.
Design: A retrospective analysis of 34 fine needle aspirations with the diagnosis of atypical/suspicious cases were obtained during the period between 1995 –2000, and the histological and/or clinical follow-up was performed.
Results:
Flow cytometry was performed on all of the atypical/suspicious lesions. It was positive/diagnostic in 16 (47%) and negative in 18(53%) cases. Excisional follow-up biopsy was obtained in 30 cases. Of these 7(21%) confirmed to be negative, 17(50%) Non-Hodgkin’s lymphoma and 6 (18%) Hodgkin’s Lymphoma.
Conclusion:
The atypical/suspicious category by fine needle aspiration is a crucial diagnosis as it has proved to represent some type of lymphoma in about two third (68%) of cases.
Author Contributions
Academic Editor: Fernando Luiz Affonso Fonseca, Instituto de Ciências Químicas, Ambientais e Farmacêuticas, Universidade Federal de São Paulo, UNIFESP
Checked for plagiarism: Yes
Review by: Single-blind
Copyright © 2014 Emad Raddaoui,et al.
 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Competing interests
The authors have declared that no competing interests exist.
Citation:
Introduction
Fine needle aspiration (FNA) cytology is a widely used diagnostic method for the assessment of various benign and malignant lymphoid lesions. It is increasingly replacing excisional lymph node biopsy in the diagnosis of lymphomas. FNA is a safe, non-invasive, reliable, rapid and cost-effective procedure. It is routinely performed as the primary diagnostic work-up for patients with lymphadenopathy, documenting recurrent disease, for staging, and for obtaining material for ancillary studies.1, 2, 3, 4, 5
Recent changes in the classification of non-Hodgkin’s lymphoma namely the WHO (World Health Organization) Classification of Tumors of Haematopoietic and Lymphoid Tissues has considerably expanded its classification of lymphomas based on molecular and cytogenetic profiling and immunophenotyping.6
The atypical /suspicious diagnostic category is clinically very important. It is used whenever the cytomorphologic or other ancillary findings such as Flow cytometry are non-conclusive of for either positive or negative diagnosis.
Material and Methods
A retrospective analysis of 34 fine needle aspirations of lymphoid lesions diagnosed as atypical /suspicious with concurrent flow cytometry results conducted at Scott & White Hospital-Texas A&M College of Medicine, Temple, Texas, U.S.A., for the period January 1, 1995, to December 31, 2000. Additionally, correlation either histologically in case of follow-up tissue biopsy was available, or clinically by close monitoring the patient’s clinical records for at least five years in case of no follow-up tissue biopsy was obtained. FNA cases with no histologic or clinical follow-up were excluded from our study. All cases were diagnosed using the World Health Organization criteria.6
FNA diagnosing categories for lymphoid lesions included: Non diagnostic, Negative, Atypical/Suspicious, Positive for Non-Hodgkin’s Lymphoma (Figure 1), and Positive for Hodgkin’s lymphoma (Figure 2).
The atypical /suspicious diagnostic category is regarded to be crucial. It is used whenever the cytomorphologic or other ancillary findings such as Flow cytometry are non-conclusive for either positive or negative diagnosis of lymphoma.
Figure 1.Positive, Non-Hodgkin lymphoma (Papanicolaou stain 50x).
Figure 2.Positive, Hodgkin’s Lymphoma, Reed Sternberg cell, Center (Papanicolaou stain 50x).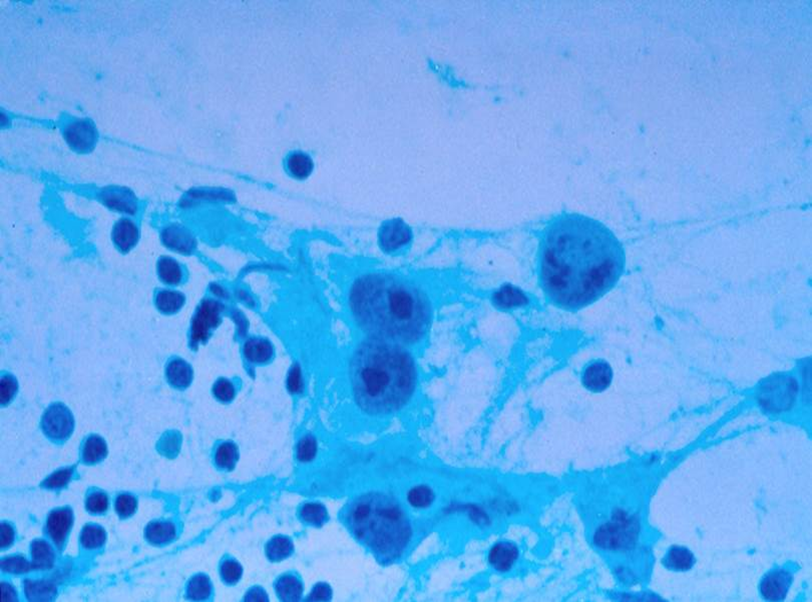
Flow Cytometry (FC) was performed in 18 out of 34 of the atypical/suspicious cases. FNA specimens received for FC are filtered and washed as required. A cytospin is prepared for each specimen, which is reviewed by a pathologist, prior to selecting the panel of antibodies for analyzing the cells from the FNA specimen. The above panel was tailored to the special requirements such as patient’s history and/or number of viable cells available in the specimen. The instrument used was the Becton Dickinson’s FACScan (BD Biosciences, San Jose, CA), 3 color staining/analysis. Approximately 0.5 million cells are allocated to each tube to which the appropriate antibodies are added. Prior to staining the kappa/lambda tubes with antibodies, these cells are washed 2-3 times with phosphate buffered saline (PBS) to remove any free floating kappa or lambda that may be present. The tubes are incubated for 15-30 minutes at room temperature and protected from light. After initial incubation, red blood cells are lysed in Becton Deckinson’s FACS Lysin Solution (BD Biosciences, San Jose, CA). After a 5-10 minute room temperature incubation to lyse red cells, each tube is centrifuged to pellet the cells. The lyse solution is decanted and the cells are washed with PBS. The PBS is decanted and the cells are fixed in 0.5 ml of a 0.5% formaldehyde fixative solution. The panel of tubes is then collected on the FACScan. Ten thousand events are collected from each tube, after a threshold is established to exclude debris. The data collected is then analyzed using Becton Dickson’s Cell-Quest software (BD Biosciences, San Jose, CA) The CD45 data is used to establish all populations in the specimen by gating from a CD45 fluorescein isothiocyanate conjugated (FITC) versus side scatter (SCC) dot plot. The data from the remaining tubes (excluding propidium iodine) is analyzed by gating CD45 prep versus SCC dot Plot. Analyzing at least ten thousand ungated events derives the viability.
Results
FNA diagnoses of all cases (175) are reported in as follows: Non diagnostic (n=3), negative (n=82), atypical (n=34), positive for Non-Hodgkin’s lymphoma (NHL), (n=53), and Hodgkin’s lymphoma (HL), (n=3).
The atypical /suspicious aspiration materials was obtained either from superficial locations in 25 of 34 cases (74%) or from deep locations with the guidance of image studies in in 9 cases (26%). An excisional follow-up biopsy was obtained in 30 of 34 cases (89%). Review of clinical follow-up treatment of all positive cases with FNA results with or without the follow-up biopsy was performed.
The patients ranged in age from 20 to 92 years of age (mean ± SD age of 64 ± 21 years). There was a 2: 1 female: male ratio (male: 11cases, female: 23 cases) .The primary site was nodal (n=29) and extra nodal (n=4). Among the (n=34) FNAs, a history of a previous diagnosis of a malignant lymphoma was available in (n=9) cases. FC was performed in 18 cases. All were reported to be negative.
Follow-up tissue biopsy was done in 30 of 34 (89%) of the cases, which revealed a positive diagnosis of malignant lymphoma in 23 of 30 cases (75%), 17 cases proved by follow up biopsy to be Non-Hodgkin’s lymphoma and 6 cases proved to be Hodgkin’s lymphoma. The atypical/suspicious category is a high risk diagnostic category and it was proved that there is a high probability of lymphoma diagnosis in the follow-up biopsies.
Discussion
Diagnosis and classification of malignant lymphoma into World Health Organization (WHO) categories are essential steps in the clinical management.6
Many studies have reported concordance rates between FNA studies and histologyof >80% (range: 76–97%).7, 8, 9
The initial diagnosis of lymphoma by FNA is challenging and, in the past it has been considered controversial.10 Some studies support its use for initial screening of patients with lymphadenopathy and suggest that the specimens obtained usually suffice for lymphoma diagnosis.11, 12, 13 Even others find that FNA specimens are mostly inadequate for diagnosis and classification of lymphoma.1 The combination of FNA and immunophenotyping by flow cytometry( FC) has been increasingly accepted as a method for primary diagnosis of NHL. It has been found to contribute to an improved classification of B-cell non-Hodgkin lymphomas (B-NHL) into WHO categories, especially for low-grade B cell lymphomas.15, 16, 17, 18
Few studies focused on the atypical/suspicious category in FNA cytology diagnosis. The latter include cases in which the final diagnosis includes the term atypical or suspicious for lymphoma, without giving a definitive diagnosis. There is no single explanation of this category. Generally, there is a lack of either cytopmorphologic criteria and/ or indefinite flow cytometry results. In one study 19of 11 cases of atypical cytology diagnosis the reasons for failing to determine a definitive diagnosis often were scant or insufficient material (5 cases) or extensive necrosis (2 cases). In 8 of the 11 cases, subsequent diagnoses of lymphoma were established by tissue biopsy, while 2 cases (1 showing reactive hyperplasia and the other granulomatous lymphadenitis) were benign.
Additionally, atypical FNA results of lymphoid lesions, as in all body sites, should be interpreted in correlation with the clinical and radiological findings. All these cases should undergo surgical biopsy followed by histological examination along with the flow cytometry; for confirmation and further classification of these haematopoietic malignancies.
Conclusion
Our study highlights the high risk potential of the atypical category diagnosis in the evaluation of FNA results of lymphoid lesions. There is a high probability of malignancy in these cases and we highly recommend a follow-up surgical biopsy followed by histological examination in conjunction with flow cytometry for confirmation and further categorization.
References
- 1.Harris N L, Jaffe E S, Stein H. (1994) A revised European-American Classification of lymphoid neoplasms: a proposal from the International Lymphoma Study Group. , Blood 84, 1361-92.
- 2.Zeppa P, Marino G, Troncone G. (2004) Fine-needle cytology and flow cytometry immunophenotyping and subclassification of non-Hodgkin lymphoma: a critical review of 307 cases with technical suggestions. , Cancer 102, 55-65.
- 3.Landgren O, Porwit M A, Tani E. (2004) Prospective comparison of fine needle aspiration cytology and histopathology in the diagnosis and classification of lymphoma. , Hematol J 5(1), 69-76.
- 4.Hehn S T, Grogan T M, Miller T P.Utility of fine needle aspiration as a diagnostic technique in lymphoma. , J Clin Oncol.2004 Aug 1, 22(15), 3046-52.
- 5.Siebert J D, Weeks L M, List L W. (2000) Utility of flow cytometry immunophenotyping for the diagnosis and subclassification of lymphoma in community hospital clinical needle aspiration/biopsies. Arch Pathol Lab Med. 124, 1792-1799.
- 6.Swerdlow S H, Campo E, Harris N L. (2008) WHO Classification of Tumours of Haematopoietic and Lymphoid Tissues.
- 7.Roha J L, Lee Y W, Kim J M. (2008) Clinical utility of fine-needle aspiration for diagnosis of head and neck lymphoma. , EJSO 34, 817-821.
- 8.Khillan Ratesh, Sidhu Gurinder, Abiotic Constantine, Albert S Braverman. (2012) Fine needle aspiration (FNA) cytology for diagnosis of cervical lymphadenopathy. , Int J Hematol 95, 282-284.
- 9.J F Nasuti, G Y U, A B oudousquie, Gupta P. (2000) Diagnostic value of lymph node fine needle aspiration cytology: an institutional experience of 387 case sobserved over a 5-year period. Cytopathology. 11, 18-31.
- 10.Wakely PE Jr. (2000) Fine-needle aspiration cytopathology in diagnosis and classification of malignant lymphoma: accurate and reliable?. , Diagn Cytopathol 22, 120-125.
- 11.Young N A, Al-Saleem T I, Ehya H, Smith M R. (1998) Utilization of fine needle aspiration cytology and flow cytometry in the diagnosis and subclassification of primary and recurrent lymphoma. , Cancer Cytopathol 84, 252-61.
- 13.Lowe S M, Kocjan G I, Edwards S G, Miller R F. (2008) Diagnostic yield of fine-needle aspiration cytology in HIV-infected patient with lymphadenopathy in the era of HAART. Int JSTDAIDS. 19, 553-6.
- 14.Hehn S T, GroganTM. (2004) MillerTP utility of fine-needle aspiration as a diagnostic technique in lymphoma. , J ClinOncol 22, 3046-52.
- 15.Bangerter M, Brudler O, Heinrich B, Griesshamnuer M. (2007) Fine needle aspiration cytology and flow cytometry in the diagnosis and subclassification of non-Hodgkin’s lymphoma based on the World Health Organization classification. Acta Cytol. 51, 390-398.
- 16.Swart G J, Wright C, Brundyn K. (2007) Fine needle aspiration biopsy and flow cytometry in the diagnosis of lymphoma. , Transfus. Apher. Sci 37, 71-79.
- 17.Barroca H, Marques C, Candeias J. (2008) Fine needle aspiration cytology diagnosis, flow cytometry immunophenotyping and histology in clinically suspected lymphoproliferative disorder: A comparative study. Acta Cytol. 52, 124-132.
