Abstract
The objective of the study was to establish the role of helmet use on severity and pattern of maxillofacial injuries among motorcycle crash victims attending Mulago Hospital. This was descriptive cross sectional case series study using a questionnaire in form of an oral interview, clinical examination and review of medical records of the patients. The pattern of injuries was assessed based on the demarcated regions of the face. The severities of the injuries were scored using the Facial Injury Severity Scale. The data were analysed using SPSS version 17.0. There were 105 participants (male/female: 97/8) aged 15 to 63 years. Most participants (n= 74, 70.5%) were riders and the rest were passengers. There were no female riders. Most participants were from Kampala and surrounding districts. Overall, 35.2% of the participants had helmets: 50% of the riders and 0% of the passengers. About 73% o the participants used Three Quarter Shell helmet design. There was no significant difference in the pattern of injuries between the passengers and non helmeted riders (p=0.076). There was a higher frequency helmeted riders (n = 15, 40.5%) with pan-facial fractures compared to other participants. Non helmeted riders and passengers had significantly more injuries to the lower two thirds of the face compared to the helmeted riders. Passengers had less severe facial injuries compared to riders. We conclude that about a third of the participants who were riders used helmets, being particularly the Three Quarter Shell design. The helmeted riders had more severe maxillofacial injuries and of panfacial category as compared to other participants. The passengers had least severe injuries compared to riders. It is recommended to carry out further studies to elucidate on motorcycle related maxillofacial injuries especially in regard to the quality of helmets and their adequate use.
Author Contributions
Academic Editor: Rahul Tandon, Loma Linda University, School of Dentistry
Checked for plagiarism: Yes
Review by: Single-blind
Copyright © 2017 Joses O. Komakech, et.al
 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Competing interests
The authors have declared that no competing interests exist.
Citation:
Introduction
Motorcycles are a common means of transportation in low and middle income countries. Their use is associated with high prevalence of injuries; a major public health concern1. Previous studies2,3 indicated a direct relationship between the frequency of motorcycle usage and injuries in different countries. Injuries due to motorcycle crashes are highest in South East Asian countries compared to other countries1.
In Nigeria, maxillo-facial injuries due to motorcycle riding constituted 50.5% to 57% of the road traffic accidents4,5. In East Africa, the trend of fatalities due to motorcycle crashes is much lower and varies with countries: 16%, Rwanda; 7%, Uganda and Tanzania, and 1%, Kenya6. Overall, injuries due to motorcycle crashes in Kampala metropolitan is estimated at about 25%7 and those involving the head region constitute about 35.5%8.
Kampala metropolitan is congested with public service vehicles; estimated at 15,000 minibuses and 30,000 motorcycles9. Currently, more motorcycles are being imported into Uganda6,7, 8, 9, 10, particularly for public transportation because of their ability to circumvent traffic congestion, versatility in reaching remote places inaccessible to public passenger vehicles and provision of employment to youths. Galukande et al.8 estimated that riding motorcycles for public transport provides employment to about 100,000 youths in Uganda. The role of helmets in protection against maxillofacial injuries is still conflicting. Some studies11, 12, 13 have implicated helmets in exacerbating maxillofacial injuries (especially of the mandible), others14, 15 reported that helmets protect the face against severe injuries, while others16, 17 indicated that helmet use significantly reduced traumatic brain injuries. Although motorcycles provide quick public transport in Uganda, they are a risk to injury8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18. A few studies8, 18 on motorcycle crashes in Uganda reported general injuries of the body without specifying the maxillofacial injuries, while Kamulegeya et al.19 had a cursory information relating maxillofacial injuries and motorbikes/helmet use. The purpose of the present study was to investigate the role of helmet use in severity and pattern of maxillofacial injuries among motorcycle crash victims attending Mulago Hospital, Uganda
Material and Methods
Study Design
This was case series descriptive cross sectional study.
Study Setting
The study was carried out in Oral and Maxillofacial Surgery, Neurosurgery and Orthopaedics units of Mulago Hospital. Mulago Hospital is a national referral and teaching health facility located in Kampala, the capital city of Uganda. The hospital has a capacity of 1500 beds. The units are specialized in managing patients, particularly with trauma who are mainly referred from other health facilities in the country.
Selection of Study Participants
The study participants (n=105) were patients aged 15 – 63 years with maxillofacial injuries following motorcycle crashes either as riders or passengers and attending Oral and Maxillofacial Surgery (n=77), Neurosurgery (n=22) and Orthopaedic unit (n=6) of Mulago Hospital. They were requested for consent/assent before recruitment into the study. Participants who were too ill to answer the questionnaire (n=3) and too young to wear a helmet (n=4) were excluded from the study.
Data Collection
A structured questionnaire was administered to the participants or their guardians in form of an oral interview by the Principal Investigator (JOK) to get background information. Information on the design of helmet into a computer and again double checked for errors and completeness. The injury severity scores based on FISSwere categorized: 1 = score 1-6 and 2 = score > 6. The data were analyzed using Statistical Package for Social Sciences Inc., (SPSS version 17.0 for windows, Chicago, Illinois, USA). Frequency distribution was used to summarize the data. Chi-square statistics was used to assess any significant differences in participants based on quantitative variables. Paired t test was used to assess the intra-examiner reliability in recording observations. The level of significance was set at p value <5%.
Reliability Test
Blind duplicate examination of mandibular fractures was conducted on 20 patients 4 days after the main survey. The agreement was substantial (Cohen’s κ = 0.70). Similarly, blind duplicate viewing of 50 radiographs, a week later gave an almost perfect agreement (Cohen’s κ = 0.84). There was neither evidence of systematic error in clinical examination nor in viewing of radiographs (paired t test, p>0.05).
Ethical Considerations
The study complied with a protocol approved by Makerere University School of Medicine Research and Ethics Committee (No. REC REF 2011-173). Permission to carry out the study was obtained from Mulago Hospital administration. Informed consent was obtained from the study participants /guardians of children below 18 years of age. In addition to the consent, the children were requested to assent to the study. The consent/assent form was translated from English into the local language (Luganda) for participants who did not understand English. The nature and purpose of the study were explained to the participants in accordance with Helsinki Declaration20. They were informed that they were at liberty to accept or refuse to participate in the study without being coerced and their refusal would not affect their relationship with investigators. No personal identifiers were used in recording the data and the final report on the findings is anonymous.
Results
The study sample constituted 105 participants (male/female: 97/8). Most participants (n= 74; 70.5%) were riders and none of them a female. They all rode the saddle motor cycles. Overall, the participants were aged 15 to 63 (mean, 29.01 ± 9.5) years with majority 62.9%, n=66) aged 21 to 30 years. The riders were aged 18 to 59 (mean, 28 ± 8.7) years while the passengers were 15 to 63 (mean, 29 ± 11.4) years. The helmeted riders were aged 18 to 59 years (mean, 30.4 ± 9.3) years and the non helmeted counterparts were 18 to 50 (mean, 27.1 ± 7.8) years. Based on the units of study, the helmeted riders were 22, 11 and 4 in Oral and maxillofacial, Neurosurgery and Orthopaedic Surgery unit, respectively.
Districts where Maxillofacial Injuries Occurred
The subjects with maxillofacial injuries came from 21 districts of Uganda. Kampala district had the majority of cases (46.7%, n = 49) followed by Wakiso district with 21.0% (n=22) and Mokono district had worn during crash was obtained from the participants with the help of pictures of helmets (Figure 1).
Figure 1.The pictures of different helmet designs used by the riders in the present study
Clinical examination for maxillofacial injuries was carried out while the patient was lying supine in the dental chair/couch with the help of artificial light by JOK. The pattern of maxillofacial bone fracture was assessed clinically and confirmed with radiological imaging.. The severity of the injuries was scored on Facial Injury Severity Scale (FISS) and recorded in a data recording form.
Data Management and Analysis
Data on completed forms were double checked for errors and completeness while the participant was still present in the clinic or ward. The data were inputted
((n=10, 9.5%; Figure 2).
Figure 2.The map of Uganda showing Kampala and some surrounding districts where participants came from to seek health care in Mulago Hospital following motorcycle crashes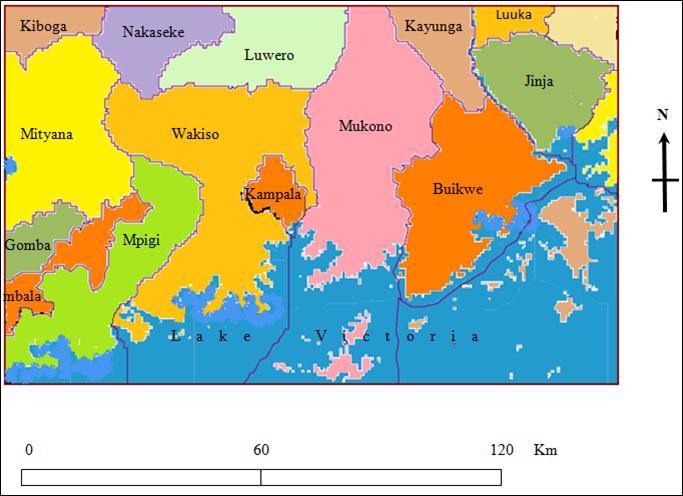
Helmet Design and Usage
Three different types of helmet design were used by the riders: the TQS (n=27, 73.0%), FF (n=8, 21.6%) and HS (n=2, 5.4%). Overall, 35.2% of the participants had helmets: 50% of the riders and 0% of the passengers (Table 1) Table 3.. Older riders were more likely to wear helmets as compared with the younger counterpart (Table 1).
Table 1. The frequency distribution of participants according to helmet usage by age groups (n=105)| Age Groups | Helmet usage, n (%) | |||
| Helmeted | Non-helmeted | Total | ||
| < 21 years | Passenger | 0 (0.0) | 4 (100) | 4 (100) |
| Rider | 2 (16.7) | 10 (83.3) | 12 (100) | |
| ≥21 years | Passenger | 0 (0.0) | 27 (100) | 27 (100) |
| Rider | 35 (56.5) | 27 (43.5) | 62 (100) | |
There was no significant difference in the pattern of injuries between the passengers and non helmeted riders (p=0.076). There was a higher frequency of helmeted riders (n = 15, 40.5%) with pan-facial fractures compared to 4 non helmeted riders and 1 passenger (Table 2). Non helmeted riders and passengers had significantly more injuries to the lower two thirds of the face compared to the helmeted riders (p = 0.020). Only 1 rider and with a helmet had injuries of the upper third of the face. The relationship between the pattern of maxillofacial injuries and helmet designs could not be assessed because of the skewed variability of helmet design.
Table 2. The frequency distribution of participants according to pattern of maxillofacial injuries and helmet use (n=105)| Helmet use | Injured part of the maxillofacial region, n (%) | |||||||
|---|---|---|---|---|---|---|---|---|
| UT | MT | LT | UTT | ULT | LTT | PF | ||
| Non helmeted | Passenger (n=31) | 0 (0.0) | 3 (9.7) | 14 (45.2) | 3 (9.7) | 0 (0.0) | 10 (32.3) | 1 (3.2) |
| Rider (n=37) | 0 (0.0) | 2 (5.4) | 17 (45.9) | 3 (8.1) | 3 (8.1) | 8 (21.6) | 4 (10.4) | |
| Helmeted | Rider (n=37) | 1 (2.7) | 4 (10.8) | 3 (8.1) | 4 (10.8) | 1 (2.7) | 9 (24.3) | 15 (40.5) |
Severity of Maxillofacial Injuries Based on FISS
The influence of gender on FISS score could not be assessed because the data were skewed towards males. The overall mean FISS was 7.0 (SD 5.3). Helmeted riders had more severe maxillofacial injuries, range 1 to 19 (mean, 10.1 ± 5.4) FISS as compared to their non helmeted counterparts (mean FISS, 6.59 ± 4.9). Passengers had the least severity of maxillofacial injuries (mean FISS, 4.0 ± 1.6; Table 3).
Table 3. The frequency distribution of participants according to severity of maxillofacial injury based on Facial Injury Severity Scale and helmet use (n=105)| Helmet use | FISS score, n (%) | ||
|---|---|---|---|
| 01-Jun | >6 | ||
| Non helmeted | Passenger (n=31) | 30 (96.8%) | 1 (3.2%) |
| Rider (n=37) | 24 (64.9%) | 13 (35.1%) | |
| Helmeted | Rider (n=37) | 12 (32.4%) | 25 (67.6%) |
Helmeted riders had significantly more severe maxillofacial injuries as compared to the non helmeted counterparts (p=0.004) and overall, the riders sustained significantly more severe maxillofacial injuries as compared to the passengers (p=0.001). Three of the participants lost an eye each: 2 helmeted riders (5.4%) and a female passenger (3.2%, Figure 3), particularly who were ejected some distance from the motorcycle to tarmac.
Figure 3.The picture of a passenger who sustained severe injuries involving loss of a left eye
Discussion
There are several scoring systems, but with challenges related to their use as previously discussed21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32 though without reaching a consensus. In the present study, FISS was used to record severity of maxillofacial injury because of its reliability21 and easy to compute22.
We observed most of the participants were from Kampala and the neighboring districts probably because the study site (Mulago Hospital) is within Kampala and in proximity of the surrounding districts. Furthermore, Kampala metropolitan has more motorcycles compared to other regions9, hence the high frequency of the injured. Additionally, although Mulago Hospital is a national referral health facility, some of the trauma patients from distant districts may have been managed in regional referral health facilities33.
In the present study, the motorcycle riders were aged 18 to 59 (mean, 28 ± 8.7) years, which is consistent with other studies elsewhere4,5,8,16,34, but higher than reported in Indianapolis, United States of America35. The lowest age permissible for acquiring a motorcycle riding license varies in different countries because of varying socio-economic, political and cultural backgrounds. In Uganda, motorcycles are mainly used for public transport, a business mainly involving youths8, while in other countries they are used so much in sports, leisure and children (as young as 14 years) commuting to school36,37.
We observed all the riders were males, who coincidentally, are the ones mostly involved in riding motorcycles for public transport in Uganda. This finding is similar to previous studies5,8,38 in Africa. Elsewhere in the world, there are variable proportions of female riders: 2.2% in Mersey and North Wales, UK34; 24.6% in Athens, Greece39; 30% in Indianapolis, USA35; 11.9% in Hyderabad, India40 and 24% in Kerala, India15.
The absence of female motorcycle riders in the present study and elsewhere in Africa may probably be due to the type of motorcycles on the market, the straddle type which do not favor mounting by female and child riders unlike the scooters, which are more appealing and commonly used in recreational and sporting activities41.
In the present study, 50% of the riders used helmet (Table 1 and Table 2) which was higher than the 17.7%8 and 29%33 earlier reported among patients attending Mulago Hospital. The older participants were more likely to put on helmet compared to the younger age group (Table 1) and this was similar to observation in Vietnam42. However, this was self motivated usage of helmet because although there is a law43 on mandatory use, it is not adequately enforced in Uganda similar to observation in Nigeria4, and contrary to the United Kingdom where the law is enforced and usage rate is 93.1%34.
Other reasons for not willing to wear helmet include: discomfort, obscuring of vision, disturbance of hearing, ruffling up hair style, cost or thefts of helmets while others said helmets are responsible for crashes39. However, in the present study, we were not able to interview the participants on the opinion about helmet use.
In the present study, about three quarters (27/37) of the riders wore helmets of Three Quarter Shell design and because of the limited variability, the relationship between helmet design and type of maxillofacial injuries could not be assessed. However, amongst the non helmeted participants, the injuries were predominantly mandibular fractures and the associated soft tissue injuries while the helmeted group had panfacial fractures in addition to mandibular fractures. Overall, most participants had injuries of the lower two thirds of the face irrespective of helmet use (Table 2). Furthermore, it may also be assumed that the Three Quarter Shell helmets predominantly used by the study participants lack the chin bar, which leaves the lower two third of the face exposed to injury. However, Yates and colleagues12 reported higher incidence of mandibular fractures amongst the riders wearing Full Face type of helmet (with chin bar) as compared to non helmeted counterparts.
We found significantly more helmeted riders had severe maxillofacial injuries (with 2 of them losing an eye each) as compared to the non helmeted counterparts (Table 3), in support of Gopalakirshna et al.11 Gopirikan et al.14 and Jayadevan et al.15, but contrary to findings from Yates et al.12. Earlier on, Brian et al.13 revealed no significant difference in severe injuries between the helmeted and nonhelmeted groups. Our finding could be due to poor quality44 or improper use of helmets like the size and fastening of the straps. However, we were neither able to assess the quality of the helmets nor the adequacy of their use.
Overall, we found the riders had sustained significantly more severe maxillofacial injuries as compared to the passengers contrary to previous workers45 who found no significant difference between the riders and passengers. Additionally, the passengers had the least severe maxillofacial injuries compared to the riders (Table 3). It could be postulated that the bodies of the riders could have shielded the passengers who ordinarily sit behind the riders. However, one female passenger lost an eye (Figure 3) and it was an isolated case where she was ejected from the motorcycle to some distance on the tarmac. This is consistent with Gopalakrishna et al.11 report that participants with maxillofacial injuries were those who were ejected from the motorcycle to some distance during the crash.
One previous study46 that used FISS as a scoring system recorded the most severely injured subject with FISS score of 11, which was much lower than 19 seen in the present study, The difference may probably be due to factors like differences in quality of the roads and motorcycle overloading. We could not assess the influence of gender on FISS score because of skewed gender distribution among the study participants.
Conclusion
About a third of the participants and only riders used helmets particularly of the Three Quarter Shell design at the time of injury. None of the passengers had a helmet. Generally, helmeted riders had severe maxillofacial injuries and of panfacial category as compared to other participants.
Recommendation
Although the present study generated baseline data, it was daunted with various limitations indicative of further studies to elucidate on factors such as the quality of helmets and their adequate use as well as mechanism of maxillofacial injuries during motorcycle crashes.
Acknowledgements
The authors are grateful to the participants for their cooperation during the study. The staff members in the study units of Mulago Hospital were instrumental in mobilizing the study participants.
References
- 1. (2004) World Health Organisation. World report on road traffic prevention, Accessed on 20.6.2016 from {http://apps.who.int/iris/bitstream/10665/42871/1/9241562609.pdf}.
- 2.Dubois L, Leijdesdorff H A, Goslings J C, Lam P H, Bui H L. (2009) Motorcycle related maxillofacial trauma in southern Vietnam: need for preventive measurements. , Intern J Oral Maxillofac Surg; 38(5), 579-84.
- 3.Maitree S. (2007) Road accidents: A common persistent problem. Keynote address on scientific conference on Road Safety On Four Continents. , Bankok, Thailand
- 4.Oginni F O, Ugboko Ogundipe O, Adegbeingbe B O. (2006) Motorcycle-related maxillofacial injuries among Nigerian intracity road users. , J Oral Maxillofac Surg; 64, 56-62.
- 5.Solagberu B A, CKP Ofoegbu, Nasir A A, Ogundipe O K, Adekanye A O. (2006) Motorcycle injuries in a developing country and the vulnerability of riders, passengers, and pedestrians. , Injury Prev; 12, 266-8.
- 6.Odero W. (2009) Motorcycle Injuries In: East Africa: Risk factors and prevention. Paper presented at the scientific meeting of the RTIRN regional workshop. , Accra, Ghana
- 7.Naddumba E K. (2007) A cross-sectional retrospective study of boda boda injuries at Mulago Hospital in Kampala-Uganda. Makerere University.
- 8.Galukande M, Jombwe J, Fualal J, Gakwaya A. (2009) Boda-boda injuries a health problem and a burden of disease in Uganda: a tertiary hospital survey. East Centr AfrJSurg. 14(2), 33-7.
- 9.Wandera G O. (2010) Urban traffic congestion in African cities – An over view of Kampala. , Kampala: Government
- 10.Sserwaniko F. (2009) Indian bikes topple Japanese. Accessed on 15.6.2016 from {http://www.newvision.co.ug/D/8220/672752}
- 11.Gopalakrishna G, Peek-Asa C, Kraus J F. (1998) Epidemiologic features of facial injuries among motorcyclists. , Ann Emerg Med; 32, 425-30.
- 12.Yates J M, Dickenson A J. (2002) Helmet use and maxillofacial injuries sustained following low speed motorcycle accidents. , Injury; 33, 479-83.
- 13.Brian M W, Bobek S, Dierks E J, Bell R B, Potter J.Comparison of helmeted and un-helmeted motorcyclists and evaluation of maxillofacial injuries. , J Oral Maxillofac Surg.2006);64(9Suppl): 33-4.
- 14.Thota G.Review of Motorcycle Related Facial Injuries Pre-and Post-2003 Pennsylvania Helmet Law Modification From 1/1998 to 8/2008 at Allegheny General Hospital,Pittsburgh,PA.JOralMaxillofac Surg.2009Sep30;67(9):. 62-7.
- 15.Jayadevan S, Jayakumary M, Binoo D, Jeesha C H. (2010) Determinants of safety helmet use among motorcyclists in Kerala. , India. J Injury Viol Res; 2(1), 49-4.
- 16.Ankarath S, Giannoudis P V, Barlow I, Bellamy M C, S J Matthews. (2002) Injury patterns associated with mortality following motorcycle crashes. , Injury; 33, 473-7.
- 17.Servadei F, Begliomini C, Gardini E. (2003) Effect of Italy’s motorcycle helmet law on traumatic brain injuries. , Injury Prev; 9, 257-60.
- 18.Naddumba E K. (2004) A Cross sectional retrospective study of Boda Boda injuries at Mulago Hospital inKampala,Uganda. , East Centr Afr J 19(1), 44-7.
- 19.Kamulegeya A, Lakor F, Kabenge K. (2009) Oral maxillofacial fractures seen at a Ugandan tertiary hospital: a six-month prospective study. Clinics. 64(9), 843-8.
- 20. (2013) World Medical Association. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. , J Am Med Assoc.2013Nov27; 310(20), 2191-4.
- 21.Chawda M N, Hildebrand F, Pape H C, Giannoudis P V. (2004) Predicting outcome after multiple trauma: which scoring system?. , Injury; 35, 347-58.
- 22.Bagheri S C, Dierks E J, Kademani D, Holmgren E, Bell R B. (2006) Application of a Facial Injury Severity Scale in Craniomaxillofacial Trauma. , J Oral Maxillofac Surg; 64, 408-14.
- 23.Kirkpatrick J R, Youmans R L. (1971) TRAUMA INDEX: an aide in the evaluation of injured victims. , JTraumaAcuteCareSurg; 11(8), 711-4.
- 24.Baker S P, O’Neill B, Haddon Jr W, Long W B. (1974) The injury severity score:a method for describing patients with multiple injuries and evaluating emergency care. , J Trauma Acute Care Surg; 14(3), 187-96.
- 25.Baker S P, O’Neill B. (1976) Injury severity score: an update. , J Trauma Acute Care Surg.1976Nov1; 16(11), 882-5.
- 26.Champion H R, Sacco W J, Lepper R L. (1980) An anatomic index of injury severity. , J Trauma Acute Care Surg.1980Mar1; 20(3), 197-202.
- 27.Knaus W A, Draper E A, Wagner D P, Zimmerman J E. (1985) APACHE II: a severity of disease classification system. , Critical Care Med; 13, 818-29.
- 28.Baxt W G, Moody P. (1987) The differential survival of trauma patients. , J Trauma Acute Care Surgery.1987Jun1; 27(6), 602-6.
- 29.Champion H R, Copes W S, Sacco W J. (1990) A new characterization of injury severity. , J Trauma; 30(5), 539-45.
- 30.G J Bazzoli, Madura K J, Cooper G F. (1995) Progress in the development of trauma systems. , I. United States. J Am Med Assoc; 273, 395-401.
- 31.Brenneman F D, Boulanger B R, McLellan B A, Redelmeier D A. (1998) Measuring injury severity: time for a change? J Trauma Acute Care Surg.1998Apr1;. 44(4), 580-2.
- 32.Al West T, Rivara F P, Cummings P, Jurkovich G J, Maier R V. (2000) Harborview assessment for risk of mortality: an improved measure of injury severity on the basis of ICD-9-CM. , J Trauma Acute Care Surg.2000Sep1; 49(3), 530-41.
- 33.Naddumba E K. (2008) Musculoskeletal Trauma Services in Uganda. Clin Orthopaedic Rel Res;. 466, 2317-22.
- 34.Sinha A K, Boot D A, Gorman D F, Teanby D N. (1995) Severe motorcycle injury in Mersey region and North Wales. , Injury.1995Oct31; 26(8), 543-5.
- 35.Mangus R S, Simons C J, Jacobson L E. (2004) Current helmet and protective equipment usage among previously injured ATV and motorcycle riders. Injury Prev;. 1056-8.
- 36.Maw-Chang L, Wen-Ta C, Li-Tung C, Liu S C, Lin S H. (1995) Craniofacial injuries in unhelmeted riders of motorbikes. , Injury; 26(7), 467-70.
- 37.Segui-Gomez M, Lopez-Valdes F J.Recognizing the importance of injury in other policy forums: the case of motorcycle licensing policy in Spain. Injury. Prev.2007;13: 429-30.
- 38.Andrew A. (2010) Motorcycle related trauma in South Sudan: a cross sectional observational study. South Sud Med J2010;. 2(4), 7-9.
- 39.Skalkidou A, Petridou E, Papadopoulos F C. (1999) Factors affecting motorcycle helmet use in the population of Greater Athens. , Greece. Injury Prev; 5, 264-7.
- 40.Michael C H, Barry L E, Davi W T, Stephen E B. (2003) Etiology and prevention of craniomaxillofacial trauma. In Peter Ward Booth, Barry L Eppley and Rainer Schmelzeisen (Eds.), Maxillofacial trauma and esthetic facial reconstruction.Philadelphia, PA:Elsevier Science,(pp. 3-19.
- 41.Zalavras C, Nikolopoulou G, Essin D, Manjra N, Lewis E. (2005) Pediatric Fractures During Skateboarding, Roller Skating, and Scooter Riding. , Am J Sports Med; 33(4), 568-73.
- 42.Hung D V, Stevenson M R, Ivers R Q. (2003) Prevalence of helmet use among motorcycle riders in Vietnam. , Injury Prev; 12, 409-13.
- 44.Mau-Roung L, Kraus J F. (2009) A review of risk factors and patterns of motorcycle injuries. Accid Analy Prev2009;. 41, 710-22.
Cited by (3)
- 1.Adebayo Ezekiel Taiwo, Fomete Benjamin, Adelusi Emmanuel Adetolu, Ahaji Lilian Ejije, Nnawuhie Ukachi Chiwendu, 2023, Maxillofacial injuries due to motorcycle accidents from suburban Nigeria, Journal of Oral and Maxillofacial Surgery, Medicine, and Pathology, 35(1), 30, 10.1016/j.ajoms.2022.07.014
- 2.Kalanzi Joseph, Wallis Lee, Nabukenya Mary, Okello Erasmus, Okong Doreen, et al, 2023, Injury patterns in patients with severe traumatic brain injuries from motor crashes admitted to Mulago hospital accidents & emergency unit, African Journal of Emergency Medicine, 13(2), 94, 10.1016/j.afjem.2023.03.003
- 3.Chalathadka Mahabaleshwara, Dengody Prasanna Kumar, Ram Bhargav, Pasha Aysha Kaleem, Madala Gayathri, et al, 2022, Patterns of maxillofacial trauma in helmet vs. non helmet wearing two wheeler drivers in a tertiary care center, Dental Traumatology, 38(4), 314, 10.1111/edt.12752