Abstract
Background:
Discharge disposition planning begins at admission and is frequently one of the first questions posed to healthcare providers by patients and families. We hypothesized that pre-injury functional status would predict discharge disposition.
Methods:
We linked prospective data from the Worcester, MA cohort of the Global Longitudinal Study of Osteoporosis (GLOW) study and the UMassMemorial Level 1 Trauma Center Registry to determine predictors of discharge disposition for female geriatric (over the age of 55) trauma patients using bivariate comparisons and multivariable modeling.
Results:
154 women of 5,091 in the Worcester GLOW cohort were evaluated for traumatic injury at UMassMemorial and were discharged alive either to their home (n=30) or to rehabilitation, skilled nursing, or nursing home facilities (n=124). The mean age was 79 years and the majority (99%) was white. There were no statistically significant differences in comorbidities or injury severity score between the groups. All women with femur fractures were discharged to a facility. The most common injury among women discharged home was traumatic brain injury. While univariate analysis revealed differences in pre-injury activity status, only age remained statistically different in a logistic regression model predicting discharge to facility (OR 2.61 per additional 10 years of age, 95% CI 1.62 to 4.19, p<0.0001).
Conclusions:
The majority of elderly women are not discharged home after injury. Pre-injury activity status was not associated with discharge disposition when accounting for other factors. It appears that physical function, which deteriorates with age, is a proxy for aging in older women at risk for osteoporosis.
Author Contributions
Academic Editor: Ian James Martins, Edith Cowan University
Checked for plagiarism: Yes
Review by: Single-blind
Copyright © 2017 Jon Dorfman, et al
 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Competing interests
The authors have declared that no competing interests exist.
Citation:
Introduction
With an aging population in the United States, trauma centers are experiencing an influx of geriatric patients. The injury mechanism is most commonly blunt trauma with falls being the most frequent (nearly 75%). Motor vehicle crashes account for remainder while penetrating trauma such as gunshot and stab wounds occur infrequently1 Simple trip and falls are not so simple in the elderly as the geriatric trauma patient has unique needs and outcomes. 2, 3 Older trauma patients have higher morbidity and twice the rate of death when compared to younger trauma patients with equivalent injuries4 These outcome differences are due a variety of factors including the physiologic changes with aging, comorbidities and medications4, 5, 6 Pre-existing conditions such as hepatic and kidney dysfunction as well as cancer have been shown to increase the risk of death5Medications including anticoagulants worsen outcomes from traumatic brain injury7
Discharge planning begins at admission. One of the first questions older patients and their families ask their trauma surgeon is whether they will be discharged home. Few studies have addressed the disposition to home, rehabilitation, skilled nursing facility or nursing home of geriatric trauma patients. Those studies that have examined disposition have not always included injury pattern and have used injury severity score as a surrogate. 8 Injury severity score may correlate better with mortality than the multiple factors that lead to a final disposition. Furthermore, the assessment tools used for the measurement of frailty have been labor intensive and unlikely to be applied clinically on a wide scale basis. 9, 10 The vast majority of patients have no pre-collected data on frailty or functional status prior to injury, leaving the trauma surgeon ill-equipped to counsel patients and families on expected discharge disposition.
We examined the discharge dispositions of a cohort of women over the age of 55 from the prospective Global Longitudinal Study of Osteoporosis (GLOW) study who also were evaluated for traumatic injury during the GLOW study period at the regional level 1 trauma center. Fifty five years of age is the cut off for trauma triage. 11 We hypothesized that pre-injury functional status would predict discharge to a facility.
Methods
The Global Longitudinal Study of Osteoporosis (GLOW) is an international study of osteoporosis administered out of the University of Massachusetts Medical School (Worcester, MA). This study included women over the age of 55 years (inclusion criteria have been previously published) 12. The Worcester GLOW cohort included 5,091 women from the local community for which the University of Massachusetts flagship teaching hospital, UMass Memorial, is the regional American College of Surgeons verified Level 1 trauma center. During the 7 year study period, a baseline survey of demographic, comorbidities, medications and Short Form -36 activity status 13 was performed followed by annual follow-up surveys. A prospective trauma registry is maintained by the trauma center.14 The University of Massachusetts Medical School Institutional Review Board approved this study.
The GLOW database (5,091 women) and the UMass Memorial Trauma Registry during the GLOW study period from January 1, 2006 to January 31, 2013 (3,326 women over the age of 55) were cross referenced by name and date of birth. From the GLOW database, we obtained age, comorbidities, recent hospitalizations in the prior year, number of outpatient visits in the prior year, number of falls in previous year and Short Form-36 activity data. Short Form-36 (SF36) activity data is a self-reported validated survey of exercise activity and activities of daily living. Response categories include “not limited”, “limited a little” or “limited a lot”. Due to the smaller sample size, we combined the categorical responses of “limited a little” or “limited a lot”; our comparison groups were therefore women who reported “not limited” versus any limitation of the queried activity. The UMass Memorial trauma registry provided mechanism, initial vital signs, types of injuries, injury severity score and discharge location. One hundred and sixty three women from the GLOW database were identified as trauma patients presenting to UMass Memorial for injury between 2006 and 2013; the traumatic injury occurred after their baseline GLOW survey. The Trauma registry was queried for demographic information, admission physiology, injury patterns, injury severity score, length of hospital stay and disposition. This inpatient hospital information was linked with the GLOW survey data and then de-identified.
The linked data were then analyzed for patient functional, demographic, and injury-related factors and discharge disposition (home vs. facility: rehabilitation, skilled nursing, or nursing home facilities). Data analysis was performed as follows. Continuous variables are shown as medians with 25th and 75th percentiles; the Mann-Whitney U test was used to test for differences between groups. Categorical variables are shown as frequency and proportion, with Fisher’s exact test or the chi square test used to test for differences. A logistic regression model predicting discharge to facility versus home was fit using backwards selection, beginning with all variables that were significant (p<0.20) on the univariate level. Variables that were significant (p<0.05) were retained in the final model. All analyses were performed in SAS version 9.2.
Results
Five thousand ninety one women between the ages of 56 and 96 who resided locally were enrolled in the Global Longitudinal Study of Osteoporosis (GLOW). One hundred sixty three of the 5,091 were evaluated at our trauma center for injury from 2006 to 2013. Of those, five died in hospital, two had missing discharge disposition information, and two were discharged to a location other than home or a facility (one was discharged to a psychiatric unit and excluded; one was excluded as injury occurred at a facility and was transferred back to that facility). The remaining 154 women were discharged either home or to a facility and comprise the study population. Their median age was 79 years (IQR 71 - 84) and their median Injury Severity Score (ISS) was 9.0 (IQR 9 - 10). Falls were the most common mechanism (n = 133, 86%) with fall on same level from slipping, tripping or stumbling the most common (n = 81, 53%), followed by fall on or from stairs or steps (n = 21, 14%). Motor vehicle crashes were the next most frequent mechanism (n= 14, 9.1%).
Thirty women were discharged home and 124 women were discharged elsewhere, either to a nursing home, skilled nursing facility (n=72, 47%) or rehabilitation center (n=52, 34%). The median SF-36 Physical Function Index Score was 80 versus 60 (p value 0.02) for patients discharged home versus a facility. Figure 1 shows discharge disposition by response to SF-36 domains where activity limitation was dichotomized to none versus any limitation. Women discharged home were less likely to report any limitation of lifting/carrying groceries, walking one hundred yards, walking several hundred yards or walking more than a mile (Figure 1).
Figure 1.Preinjury activity status by discharge status. Univariate analysis of Short Form 36 self-reported “no limitation” of the activity on the GLOW baseline survey as compared with the disposition outcome. (*denotes p-value ≤0.05 )
Women discharged home were younger with a median age of 70 years old (IQR 64, 76) as compared to women discharged to facility, median age 81 years old (IQR 74, 85), p value <0.0001. No statistically significant differences were noted in pre-existing cardiopulmonary disease or other comorbidities (Figure 2). When comparing the number of recent inpatient hospitalizations in the year prior to the GLOW baseline survey, there were no differences between the two groups. No statistical differences were found in the number of outpatient doctor’s visits (Table 1) or self-reported falls between the two groups (Table 2).
Figure 2.Co-morbidities of women compared by discharge status. Comparison of comorbidities of the injured GLOW study participants between those women discharged home and those women discharged to rehabilitation, skilled nursing facility or nursing home. (*Fisher’s exact test used due to small cell values)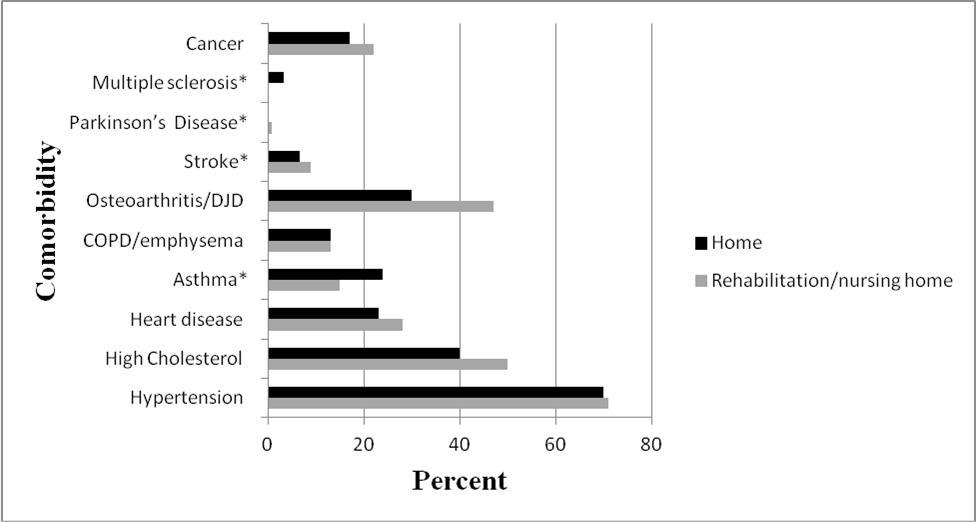
| Discharged to facility (n=124) | Discharged home (n=30) | p-value | ||
| Outpatient | 0.56* | |||
| None | 4 (3.3) | 2 (6.7) | ||
| 1 to 2 | 36 (29) | 7 (23) | ||
| 3 to 5 | 43 (35) | 13 (43) | ||
| 6 or more | 40 (33) | 8 (27) | ||
| Inpatient | 0.40* | |||
| None | 94 (76) | 27 (90) | ||
| 1 | 19 (15) | 2 (6.7) | ||
| 2 | 4 (3.3) | 1 (3.3) | ||
| 3 or more | 6 (4.9) | 0 (0.0) |
| Discharged to rehab (n=124) | Discharged home (n=30) | p-value | |
| None | 59 (48) | 13 (45) | 0.29 |
| Once | 30 (24) | 4 (14) | |
| 2 or more | 35 (28) | 12 (41) |
Admission vital signs during the trauma hospitalization were not statistically different between groups. Median admission systolic blood pressure was 146 mmHg versus 148 mmHg respectively. Two of the patients discharged to a facility were intubated versus none of the patients discharged to home. This difference was not statistically significant.
Examining the women’s injury patterns, median ISS did not differ by discharge group. Overall, head and extremity injuries were the most common. Femur fractures were the most common injury in patients discharged to a facility. No woman with a femur fracture was discharged home. Concussions and subdural hematomas were the most common injuries among women discharged home. (Table 3)
Table 3. Most frequent diagnosis based on disposition.| Discharged to rehab (n=124) | Discharged home (n=30) | |||
| n | % | n | % | |
| Femur fracture (intertrochanteric) | 33 | 31 | 0 | 0 |
| Concussion | 10 | 9.3 | 8 | 33 |
| Subdural hematoma | 3 | 2.8 | 3 | 13 |
In a logistic regression model predicting discharge to a facility, age was the only statistically significant variable. Every 10 year increase in age increased the odds of being discharged to a facility versus home, by 2.6 (95% CI 1.62 – 4.19). In the model fitting process the SF-36 physical function index score was the next most significant variable, with a p-value of 0.09; it might have been statistically significant with a larger sample size. An interaction between age and physical function was not statistically significant
(p = 0.33).
Discussion
This study links self-reported health and functional status of older women prior to sustaining an injury severe enough to warrant trauma center evaluation with injury related factors and post-injury discharge disposition. Contrary to our hypothesis, we found that pre-injury functional status did not predict discharge disposition. Age was the only independent predictor of discharge disposition. Our findings have implications for surgeons who are asked by families to predict potential discharge location soon after injury given that many of these conversations focus on pre-injury functional status and quality of life and desire to return to a level similar to baseline.
Falls were by far the most common mechanism of injury in our cohort; and, head and extremity injuries were the most common injury patterns sustained by women in our study. These injury mechanisms and patterns of injury are similar to previously published geriatric trauma studies15. With the aging of the US population 16, trauma centers will be seeing increasing numbers of geriatric falls patients. Therefore, understanding the key factors in discharge planning for this vulnerable group is important.
We found that neither injury severity nor physiology on presentation predicted discharge disposition. Previous studies have not found that ISS and RTS predict discharge disposition in multivariate models 17. These risk adjustment markers have been validated only in mortality studies.
Previous studies have found walking speed, grip strength and weight to be predictors of discharge location in surgical patients18. The surgical patient population in these studies benefitted from preoperative assessment for elective procedures. Clearly, traumatic injury is not predictable and pre-trauma assessment is not feasible; however, in our study we have access to activity assessment prior to the traumatic injury, albeit at varying lengths of time prior to the traumatic injury. In our patient population we found that such detailed knowledge of physical functioning is not as important as age itself in determining discharge disposition. However, a prospective study of geriatric trauma patients, which utilized a still more detailed 50 question frailty index found the index to be best predictor of discharge location with age being insignificant when controlling for this index 17 Ultimately, this method works well as a research tool but would be difficult to implement in clinical practice. Our findings emphasize need for surgeons to consider the implications of age even with patients who are reportedly very high functioning since these familial assessments of pre-injury functions are unlikely to be as precise as this tool.
The univariate analysis of activity data revealed significantly decreased activity restrictions in the women discharged home versus those discharged to a facility. The activity difference was not noted for all queried activities but found in walking and lifting groceries. Women discharged home had a greater Physical Function Index Score than women discharged to a facility. This finding suggests that pre-injury activity may matter in the ultimate discharge disposition. Given our sample size, we were restricted in the number of variables we could incorporate into our prediction model. In logistic regression analysis these activity restrictions were no longer independently statistically significant and only age remained a large and significant predictor of discharge disposition. Increasing age was a very strong predictor of discharge to facility, with an odds ratio of 2.61 for each 10 year increase. The extent of this association and the loss of activity status as a predictor indicate a strong correlation between aging and activity. 19, 20 This finding is important in an era where there is a focus on discharge. Tools such as the SF-36 may not be applicable for discharge disposition.
There are some limitations to our research. This was a retrospective study linking prospective data on bone health with trauma registry data. For GLOW, functional status data was not measured for the purposes of measuring injury incidence therefore we were limited to questions about activity restriction and the extent of restriction of particular activities. Importantly, we lacked data on baseline cognitive status, nutritional status, and mental health issues which may impact discharge disposition after injury. While we are the only Level 1 trauma center in our region, we may have missed women who moved or went to other local hospitals for less severe injuries. Due to our small sample size, restricted as the data was previously collected for other purposes, we collapsed discharge disposition to home versus not home; however, clinically there may be differences between those who go to a skilled nursing facility as compared to a rehabilitation center that we have not explored. Finally, while we accounted for comorbidities, we may be missing other aspects of discharge disposition not related to injury patterns or functional status such as social networks, insurance restrictions and facility location. Prior
Studies21, 22 have shown that insurance or the lack thereof plays an important role in disposition and post-hospital services. Even in Massachusetts which passed health reform in 2006, trauma patients were more likely to be uninsured and more likely to be discharged home without services.23. Furthermore, insurance companies can also restrict access due to cost containment measures. These influences are difficult to account for and therefore could confound our results.
Strengths include that, to our knowledge, this is one of few studies in the literature measuring wellness and functional status data prior to any traumatic injury. The questionnaire was collected during a stress free time period and therefore may have less recall bias. Secondly, head injury was common within our cohort and is one of the most common injuries in the elderly. Memory and recall of activity status would therefore not be impacted as it could be if the SF-36 data were collected in the acute injury period.24 Furthermore, activity status was collected from the patient and not a surrogate as has occurred in prior studies 6 when the patient could not answer for themselves. A surrogate could potentially have inaccurate or incorrect perception of a patient’s activity status.25, 26
Conclusion
Our results suggest that age and age associated changes in wellness and functional status are the strong predictors of discharge location. Future studies with larger sample sizes may be able to refine which specific activity limitations and what extent of limitation are the most helpful factors and clinically useful to ultimately predict discharge location.
Disclosure :
The authors report no proprietary or commercial interest in any product mentioned or concept discussed in this article.
Funding statement: This work was partially supported by grants from NIH (8KL2TR000160-03), AHRQ (R01HS22694), and PCORI (ME-1310-07682) to HPS.
Author Contributions
JD- study design, data management, interpretation of results, manuscript review
AW-data analysis, data management, manuscript review
GF-study design, interpretation of results
BC- data management, manuscript review
TE-manuscript review
FA- manuscript review, PI of GLOW study, obtained funding for GLOW study
HS-study design, interpretation of results, manuscript review
References
- 1.Bonne S, DJE Schuerer. (2013) Trauma in the Older Adult: Epidemiology and Evolving Geriatric Trauma Principles. Clin Geriatric Med. 29(1), 137-150.
- 2.MacKenzie E J, Rivara F P, Jurkovich G J, Nathens A B, Frey K P.. , Egleston BL et al.(2006) A National Evaluation of the effect of Trauma-center Care on Mortality. N Engl J of 354(4), 366-78.
- 3.Sasser S M, Hunt R C, Faul M, Sugerman D, Pearson W S et al. (2011) Guidelines for field triage of injured patients: recommendations of the National Expert Panel on Field Triage. , MMWR Recomm Rep 61(1), 1-23.
- 4.Perdue P W, Watts D D, Kaufmann C R, Trask A L. (1998) Differences in mortality between elderly and younger adult trauma patients: geriatric status increases risk of delayed death. , J Trauma 45(4), 805-810.
- 5.Grossman M D, Miller D, Scaff D W, Arcona S. (2002) When Is an Elder Old? Effect of Preexisting Conditions on Mortality in Geriatric Trauma. , J of Trauma 52(2), 242-246.
- 6.Zafar S N, Obirieze A, Schneider E B, Hashmi Z G, Scott V K et al. (2015) Outcomes of trauma care at centers treating a higher proportion of older patients: The case for geriatric trauma centers. , J Trauma 78(4), 852-859.
- 7.Pieraccci F M, Eachempati S R, Shou J, Hydo L, Barie P S. (2007) Degree of Anticoagulation, but not Warfarin Use Itself, Predicts Adverse Outcomes After Traumatic Brain Injury in Elderly Trauma Patients. , J of Trauma 63(3), 525-530.
- 8.Joseph B, Pandit V, Rhee P, Aziz H, Sadoun M et al. (2014) Predicting hospital discharge disposition in geriatric trauma patients: Is frailty the answer?. , J of Trauma 76(1), 196-200.
- 9.Min L, Ubhayakar N, Saliba D, Kelley‐Quon L, Morley E et al. (2011) . The Vulnerable Elders Survey-13 Predicts Hospital Complications and Mortality in Older Adults with Traumatic Injury: A Pilot Study. J of the Am Ger Soc 59(8), 1471-1476.
- 10.Gabbe B J, Cameron P A, Wolfe R, Simpson P, Smith K L et al. (2005) Predictors of Mortality. , Length of Stay and Discharge Destination in Blunt Trauma. ANZ J Surg 75(8), 650-656.
- 11.Scott M Sasser. (2012) Guidelines for field triage of injured patients: recommendations of the. National Expert Panel on Field Triage,2011.Morbidity and Mortality Weekly Report:Recommendations and Reports 61(1), 1-20.
- 12.Hooven F H, Adachi J D, Adami S, Boonen S, Compston J et al. (2009) The Global Longitudinal Study of Osteoporosis in Women (GLOW): rationale and study design. , Osteoporosis Int 20(7), 1107-1116.
- 13.Ware J E, Kosinski M, Dewey J E. (2000) How to score version 2 of the SF-36 health survey (standard & acute forms). Quality Metric Incorporated.
- 14.Rotondo M F, Cribari C, Smith RS ed. (2014) Resources for the optimal care of the injured patient 6th edition.American College of Surgeons.
- 15.Richmond T S, Kauder D, Strumpf N, Meredith T. (2002) Characteristics and outcomes of serious traumatic injury in older adults. , J Am Geriatr Soc 50(2), 215-222.
- 16.Colby S L, Ortman J M.. (2014).Projections of the Size and Composition of the U.S. Population: 2014to 2060,Current Population Reports,P25-1143,U.S.Census Bureau,Washington,DC .
- 17.Joseph B, Pandit V, Zangbar B, Kulvatunyou N, Hashmi A et al. (2014) Superiority of Frailty Over Age in Predicting Outcomes Among Geriatric Trauma Patients A Prospective Analysis. , JAMA Surg 149(8), 766-772.
- 18.Makary M A, Segev D L, Pronovost P J, Syin D, Bandeen-Roche K et al. (2010) Frailty as Predictor of Surgical Outcomes in Older Patients. , J Am Coll Surg.210(6): 210, 901-908.
- 19.Lauretani F, Russo C S, Bandinelli S, Bartali B, Cavazzini C et al. (2003) Age-associated Changes in Skeletal Muscles and their Effect on Mobility: an Operational Diagnosis of Sarcopenia. , J Appl Physiology 95(5), 1851-1860.
- 20.Hunter S K, Thompson M W, Adams R D. (2000) Relationship Among Age-Associated Strength Changes and Physical Activity level, Limb Dominance, and Muscle Group in Women. , J of Geront.55(6):B264-B273
- 21.Nirula R, Nirula G, Gentilello L M. (2009) Inequity of Rehabilitation Services after Traumatic Injury. , J Trauma 66(1), 255-259.
- 22.Sacks G D, Hill C, Rogers S O. (2011) Insurance Status and Hospital Discharge Disposition after Trauma: Inequities in Access to Postacute Care. , J Trauma 71(4), 1011-1015.
- 23.Santry H P, Collins C E, Wiseman J T, Psoinos C M, Flahive J M et al. (2014) Rates of insurance for injured patients before and after health care reform in Massachusetts: a possible case of double jeopardy. , Am J Public Health 104(6), 1066-1072.
- 24.Belanger H G, Curtiss G, Demery J A, Lebowitz B K, Vanderploeg R D. (2005) Factors Moderating Neuropsychological Outcomes Following Mild Traumatic Brain Injury: A Metanalysis. , J of Int Neuropsychol Soc 11, 215-227.
