Abstract
Objective:
Skipping breakfast has been associated with an increased risk of obesity. This randomized controlled pilot study tested whether emphasizing breakfast consumption, in conjunction with nutrition counseling, would improve weight status and dietary quality in children.
Design and Methods:
Twenty children were recruited and randomized to a breakfast (BF, n=11) or control (n=9) intervention. Both groups received weekly group nutrition counseling for 12 wk but breakfast consumption was emphasized, and ready-to-eat (RTE) cereal provided, to BF only. Anthropometric measurements were taken weekly. Three-day food records were taken at baseline and endpoint.
Results:
Weight status did not change significantly, however, children in BF displayed an overall decrease in BMI (-1.0±5.1%) whereas children in the control group had an overall increase (1.1±7.2%) from baseline (P=0.52). Three-day food records (BF, n=6; control, n=5) revealed group x time interactions on total sugars (P=0.007), folate (P=0.05), vitamin B12 (P=0.03), sodium (P=0.05), niacin (P=0.009), and vitamin B6 (P=0.023). Except for sodium, BF had improvements in these nutrients relative to the control group.
Conclusions:
Preliminary data from this study show that the provision of RTE cereal with weekly nutrition counseling may positively affect intake of essential nutrients. The effects of breakfast consumption on weight status are still uncertain.
Author Contributions
Academic Editor: Marcello Iriti, Milan State University
Checked for plagiarism: Yes
Review by: Single-blind
Copyright © 2015 Amanda Unanski Enright, et al.
 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Competing interests
The authors have declared that no competing interests exist.
Citation:
Introduction
Obesity is the primary nutritional disorder affecting children in the United States.1 The prevalence of obesity among children remains alarmingly high, particularly among minority and underserved populations.2 Recent population surveys show that 18% of children are obese, but these numbers can be as high as 1 in 3 in some ethnic groups.2 Being obese during childhood is associated with more severe and costly lifetime health burden.3 For this reason, identifying dietary interventions to prevent future weight gain is a public health and research priority.
Breakfast consumption is one possible intervention target. Participation in school breakfast programs is inversely related with childhood obesity, suggesting that infrequent breakfast consumption could be a risk factor for developing obesity.4 School children who consumed breakfast everyday had a significantly lower BMI† than children who did not consume breakfast regularly.5 Moreover, breakfast skipping was associated with increased intra-abdominal adiposity in Latino youths.6
Breakfast skipping in childhood may also be associated with poor adult health outcomes. A longitudinal study of Australian youth revealed that children who reported more frequent breakfast skipping were more likely to develop metabolic complications during adulthood.7 Thus, breakfast consumption may be an important area to target to improve both current and future health.
Unfortunately, breakfast skipping is not uncommon. A national survey found that 20% of American children and 31.5% of adolescents are breakfast skippers.8 This study also found that there are particular benefits, including lower total fat and cholesterol intakes, higher dietary fiber and micronutrient intakes, for children and adolescents who consume RTE‡ cereal for breakfast. A study of low-income, minority children from Texas also found improved nutritional intake and lower BMI in children who regularly consumed RTE cereal over a 3-year period.9 Breakfast skipping may be a frequent yet preventable behavioral target for obesity prevention. Additionally, encouraging RTE cereal as a form of breakfast may help improve nutritional intake.
A randomized controlled trial testing the effects of RTE cereal consumption on weight status found that only children who received combined RTE cereal and nutrition education improved their weight status; children in groups receiving just RTE cereal for breakfast, RTE cereal for breakfast and dinner, and control did not have improvements in weight.10 However, it is presently not known whether promoting breakfast consumption, specifically RTE cereal consumption, among non- or infrequent breakfast consumers will improve weight status and nutritional intake.
The purpose of the present study was to test the impact of breakfast consumption, as part of a healthy eating counseling program, on body weight and diet quality in obese school-age children from New York City. We hypothesized that children receiving nutrition counseling with an emphasis on breakfast consumption (BF)* would have improved weight status, reduced intakes of fat and increased intakes of calcium and fiber relative to children who received the same nutrition counseling without an emphasis on breakfast (control). The findings from this study would directly support clinical recommendations for children to eat breakfast daily, specifically RTE cereal, and would underline the importance of school breakfast programs as a means of achieving a healthy weight and healthy diet.
Materials and Methods
Subject Selection and Screening
Children were recruited via online advertisements and flyers posted around the community and at New York City public schools. Parents who responded to our advertisements were initially screened by phone about the health status of their child. Only overweight and obese children between the ages of 7 and 9 years who regularly skipped breakfast were eligible for participation. Children were eligible if they had a BMI ≥95th percentile for their sex/age or a BMI ≥85th percentile and one obese parent. Regular breakfast skipping was defined as having a parentally reported breakfast intake of <5 times/wk. Children were excluded if they had any diagnosed health or behavioral condition, or if they reported use of prescription medication. Children were also excluded if they had a T-score >70 on the Child Behavior Checklist.11 The study was approved by the St. Luke’s/Roosevelt Hospital Institutional Review Board. Parents provided consent and children provided written assent prior to their enrollment into the study.
During the phone screening, parents were given an overview of the study requirements and questioned about their child’s weight and health status. If parents reported a BMI and breakfast consumption pattern for their children that were consistent with the inclusion criteria, an in-person screening was scheduled. At the in-person screening, eligibility was confirmed and information was collected about the child’s sleep, physical activity, and dietary patterns. Physical activity was defined as any bout of vigorous activity involving physical effort that would cause one to breathe much harder than normal for at least 10 min over the past week. Also, information was gathered about the family’s socio-demographic status, the parent’s breakfast consumption, the parent’s general dietary habits, and the family’s history of obesity. Information about the child’s eating behavior was reported by parents with the Children’s Eating Behavior Questionnaire.12
At the end of the screening session, parents were given a 3-d food diary to complete prior to the first counseling session. They received the same 3-d food diary at wk 11 to complete for wk 12. Parents were told to provide information on all foods consumed, including method of preparation and brand names or specifics related to the food, such as low-fat or non-fat, sugar-free, etc., for 2 weekdays and 1 weekend day. Food records were reviewed with the investigator at the following session and questions were asked to gather any necessary additional information. In addition to completing 3-d food diaries at wk 0 and 12, parents were instructed to keep weekly records of their child’s breakfast consumption and screen time.
Nutrition Counseling Sessions
Participants were randomized, with the use of a random digit table, to one of two groups: BF and control. The BF group received nutrition counseling with an emphasis on breakfast consumption and also received a weekly supply of RTE cereal (Post Foods, Battle Creek, MI) at every counseling session. Children could choose from 4 different kinds of cereals selected for this study based on criteria for inclusion in the Women, Infants, and Children program. Specifically, cereals had to contain <21g of sugar per 100 g. At the first counseling session, participants in the BF group received 2 boxes of cereal; they received one box at each subsequent session. This system provided each child with enough cereal for daily breakfast consumption, and children had an extra box if a session was missed. Children were told how much of each cereal they should eat on a daily basis based on the serving size listed on the nutrition facts panel. Each box provided 9 servings of cereal; parents were told that one box should be consumed each week, providing approximately 1.25 servings/d. Children in the control group received the same counseling, without the emphasis on breakfast, and did not receive cereal. All counseling sessions were held at the New York Obesity Nutrition Research Center and lasted approximately 30 min.
The lessons were developed based on the Stoplight Diet.13 This approach categorizes foods as red, yellow, or green, based on the food’s recommended frequency and amount of consumption. Red foods were high-energy dense foods (e.g. candy, fried foods, pastries) that were limited in consumption to 7/wk. Yellow foods (e.g. low-fat dairy, whole wheat breads, and starchy vegetables) could be consumed, but children were urged to adhere to pre-determined serving sizes. Green foods (e.g. most fruits and vegetables and non-caloric condiments) were “anytime” foods. In the BF group, each session included a reminder to eat breakfast daily, and breakfast was always used as an example when describing how to make healthier meals or choices. For the control group, a meal other than breakfast was used for examples during sessions, and the participants were not reminded to eat breakfast daily. In addition to the Stoplight Diet approach, weekly lessons for both groups also focused on healthful lifestyle changes, including healthy snacking, beverages, activity, and energy balance. Lessons were designed specifically for this study and were targeted at the child (Online Supplemental Material).
Anthropometric Measures
Children’s weight, height, waist and hip circumference were measured at baseline (wk 0) and wk 12. In addition, weight, waist and hip circumference were measured at each weekly session. Weight was measured without shoes, on a Tanita digital scale (BWB-800AS, Arlington Heights, Illinois). Height was measured without shoes using a stadiometer. Waist and hip circumferences were each taken twice, using a non-stretch measuring tape, and the mean of each measurement was calculated.
Dietary Intake Measures
Dietary intake was assessed from parent-reported 3-d food records at baseline and wk 12. The University of Minnesota Nutrition Data System for Research software (2011, Minneapolis, Minnesota) was used to analyze the data. Nutrient values from each dietary record were averaged to estimate daily intakes for wk 0 and wk 12.
Statistical Analysis
The main outcome measures were changes in body weight, BMI, BMI z-score, and waist circumference, from baseline to wk 12. Only completers were included in the analysis. Completers were classified as those children who attended counseling sessions through wk 10. Week 10 and 11 measurements were carried forward for those who did not show up at the endpoint visit. One child, who attended the last measurement, was removed from the completers’ analyses because she failed to attend 5 of the 12 sessions. Including this child in the analyses did not affect the results, and data are presented without her. In addition, two children reported high breakfast consumption at screening (everyday). One child, randomized to the control group, reported low breakfast consumption for 11 of the 12 wk of the study (<5 times/wk) and therefore was considered a habitual breakfast skipper and was retained in the analyses. The other child, randomized to the BF group, reported high breakfast consumption throughout the study (6-7times/wk). Data were similar when analyzed with or without this child and therefore he was kept in the final analyses.
Mixed models analysis of variance with group assignment and time as main effects and group assignment x time interaction were run for all outcome measures. These analyses were adjusted for age. Sex was not a significant covariate for any of the outcome variables and was therefore not included in the models. Differences in percent change in BMI and change in BMI z-score between groups were assessed using an unpaired t-test.
Change in intake of total fat, saturated fat, and calcium from baseline to week 12 were secondary endpoints that were analyzed by mixed models analysis of variance, controlling for body weight and energy intake. Time, group assignment, and time x group assignment interaction were included as independent variables in these models. Six children in the BF group and 5 in the control group provided food records at both baseline and endpoint. Data from all completed food records were analyzed.
Statistical Analysis Software version 9.2 was used to analyze the data (SAS Institute, Cary, NC). All data are presented as means±SEM. Data are reported as adjusted values unless otherwise noted. A P-value of<0.05 was considered significant.
Results
Demographics
Twenty-five children provided informed assent to participate in the study and 20 started the counseling sessions. Of those, 16 completed the study: 8 in BF and 8 in control. Of the completers, 3 children in the control group and 2 in the BF group did not complete 3-d food diaries. The majority of participants in the study were Hispanic (45%) or Black (35.0%, Table 1). Half of the children who entered the study reported eating breakfast 2-3 times/wk.
Table 1. Baseline characteristics for all participants enrolled in the study.| Breakfast | Control | |||
| All | Completers | All | Completers | |
| 11 | 8 | 9 | 8 | |
| Gender, M/F | 4/7 | 3/5 | 4/5 | 4/4 |
| Age* (years) | 7.8±0.3 | 7.6±0.2 | 8.2±0.2 | 8.3±0.3 |
| Baseline BMI* (kg/m2) | 25.5±0.7 | 25.0±0.7 | 22.6±0.6 | 22.3±0.6 |
| Days being physically active in past week (days)* | 3.0±0.5 | 3.2±0.7 | 2.3±0.4 | 2.3±0.5 |
| Race, Black/Hispanic/White/Asian-Pacific Islander/Other | 5/5/1/0/0 | 3/4/1/0/0 | 2/4/0/1/2 | 2/3/0/1/2 |
| Breakfast Consumption Prior to Start of Study (d/wk), 2-3 d/3-4 d/4-5 d/7 d | 5/2/3/1 | 3/2/2/1 | 5/0/3/1 | 4/0/3/1 |
| Servings of Sugar-Sweetened Beverage Consumption Prior to Start of Study (d/wk)<1 per wk/3-6 per wk/1-3 per day/>3 per day/no response | 1/3/6/1/0 | 1/2/5/0/0 | 1/7/0/0/1 | 1/6/0/0/1 |
Anthropometric Measures
There was a main effect of group on BMI z-score (P=0.02) but no main effect of time (P=0.16) or group-by-time interaction (P=0.81, Table 2). Children in the control group had lower BMI z-scores than children in the BF group at baseline (P=0.03) and follow-up (P=0.02). Children in the BF group displayed an overall decrease in BMI (-1.0±5.1%) whereas children in the control group had an overall increase in BMI (1.1±7.2%) from baseline to endpoint (P=0.52). Within-group changes in BMI were not statistically significant. Weight status and reported breakfast consumption throughout the study were not significantly correlated (P=0.3, Figure 1 andFigure 2).
Table 2. Body weight throughout the 12-week intervention in groups receiving healthy eating counseling alone (Control) or healthy eating counseling with an emphasis on breakfast consumption (BF).| Week | Body weight (kg) | BMI Z-score | BMI (kg/m2) | |||
| BF | Control | BF | Control | BF | Control | |
| 0 | 47.1±2.2 | 41.3±2.2* | 2.24±0.10 | 1.88±0.11* | 25.7±0.7 | 22.2±0.7* |
| 12 | 48.1±2.2† | 42.8±2.2† | 2.16±0.11 | 1.78±0.11* | 25.3±0.7 | 22.4±0.7* |
| Change, % | 2.5±1.1 | 3.3±2.3 | -3.6±2.1 | -6.5±7.0 | -1.0±1.8 | 0.3±2.5 |
Figure 1.Weight status and breakfast consumption throughout the 12-week study period.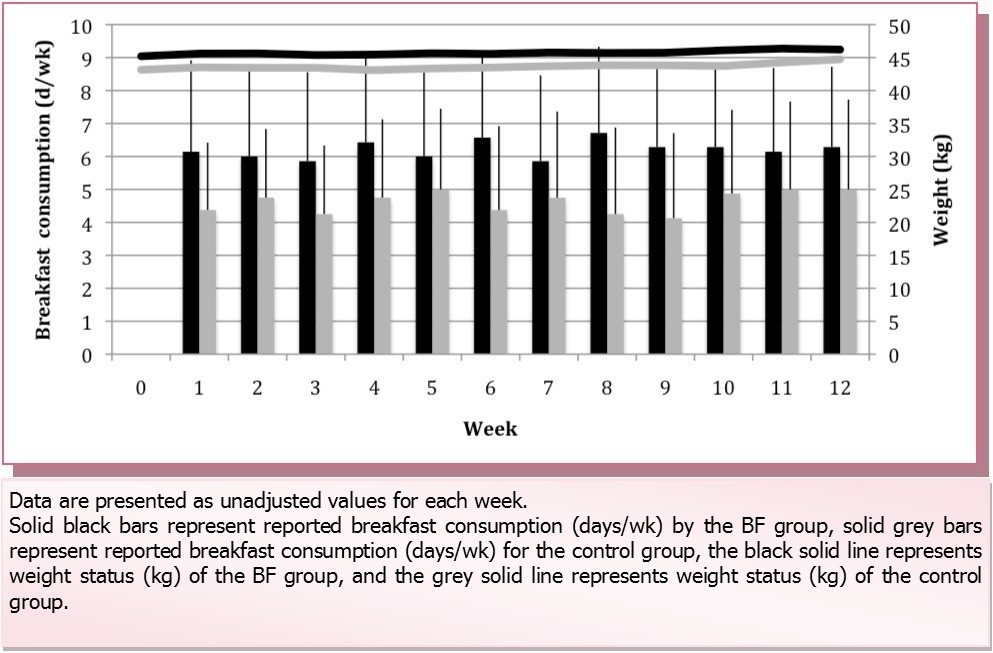
Figure 2.Correlation between percent change in body mass index and average breakfast consumption during the 12-wk study for all of the children who completed the study.
Food Intake and Lifestyle Habits Data
There was no group, time, or group x time interaction on energy, carbohydrate, and protein intakes (Table 3). There was a significant effect of time on fat intake (P=0.03). Group x time interactions were observed for various nutrients: total sugars (P=0.007), folate (P=0.05), vitamin B12 (P=0.03), sodium (P=0.05), niacin (P=0.009), vitamin B6 (P=0.023); and trends for many others: monounsaturated fatty acids (P=0.09), added sugars (P=0.05), riboflavin (P=0.08), and iron (P=0.06). With the exception of sodium, improvements were observed in children who were randomized to the BF group relative to the control group.
Table 3. Self-reported food intake at baseline and after 12 wkin groups receiving healthy eating counseling alone (Control) or healthy eating counseling with an emphasis on breakfast consumption (BF).| Nutrient | BF(n=6) | Control(n=5) | Difference between groups at endpoint | Group x Time interaction | ||
| Baseline | Endpoint | Baseline | Endpoint | P-value | P-value | |
| Energy, kcal | 1436.3±133.2 | 1439.7±131.7 | 1653.8±144.2 | 1415.4±146.9† | 0.90 | 0.20 |
| Carbohydrates, g | 176.8±10.4 | 181.6±10.3 | 183.3±11.8 | 183.6±11.5 | 0.90 | 0.81 |
| Protein, g | 62.1±4.5 | 65.2±4.5 | 63.5±5.1 | 57.3±5.0 | 0.25 | 0.32 |
| Fat, g | 59.5±2.9 | 56.0±2.9 | 59.0±3.3 | 47.1±3.2* | 0.053 | 0.20 |
| Saturated fat, g | 20.3±1.4 | 18.3±1.3 | 19.2±1.5 | 16.5±1.5 | 0.39 | 0.82 |
| Monounsaturated fat, g | 20.5±1.5 | 20.4±1.5 | 21.5±1.7 | 15.7±1.6* | 0.048 | 0.090 |
| Polyunsaturated fat, g | 13.5±1.2 | 12.7±1.1 | 13.3±1.3 | 10.5±1.3 | 0.21 | 0.41 |
| Total sugars, g | 78.2±8.8 | 72.0±8.7 | 66.5±9.9 | 102.8±9.8** | 0.038 | 0.0070 |
| Fiber, g | 10.2±1.3 | 12.2±1.3 | 11.3±1.4 | 10.6±1.4 | 0.41 | 0.33 |
| Vitamin A, IU | 4715.4±1651.7 | 7568.6±1638.5 | 2252.9±1864.7 | 2571.6±1821.9 | 0.058 | 0.48 |
| Vitamin D, μg | 4.3±0.7 | 5.5±0.7 | 4.1±0.7 | 3.3±0.7 | 0.036 | 0.15 |
| Niacin, mg | 18.8±1.5 | 22.3±1.5 | 20.7±1.7 | 14.9±1.6* | 0.0036 | 0.0087 |
| Riboflavin, mg | 1.5±0.1 | 1.8±1.1† | 1.6±0.1 | 1.4±0.1 | 0.036 | 0.077 |
| Folate, μg | 346.1±45.3 | 468.4±44.9† | 358.8±51.2 | 261.9±50.0 | 0.0073 | 0.049 |
| Pantothenic acid, mg | 3.2±0.4 | 4.3±0.4† | 3.5±0.5 | 3.9±0.5 | 0.55 | 0.50 |
| Vitamin B6, mg | 1.5±0.2 | 2.2±0.2* | 1.5±0.2 | 1.2±0.2 | 0.0025 | 0.027 |
| Vitamin B12, μg | 3.6±0.6 | 5.4±0.6 | 3.6±0.7 | 2.4±0.7 | 0.0028 | 0.025 |
| Iron, mg | 12.3±1.7 | 15.4±1.7 | 12.4±1.9 | 9.5±1.9 | 0.037 | 0.063 |
| Calcium, mg | 649.3±78.9 | 761.8±78.2 | 583.1±89.2 | 616.3±87.1 | 0.23 | 0.64 |
| Magnesium, mg | 163.7±13.2 | 183.3±13.1 | 175.7±14.9 | 167.1±14.6 | 0.42 | 0.33 |
| Sodium, mg | 2587.7±173.2 | 2828.6±171.0 | 2446.5±193.7 | 2190.0±191.4 | 0.031 | 0.047 |
By the end of the study (wk 12), there was a trend for more frequent breakfast consumption by children in the BF group compared to the control (6.3±1.0 d/wk vs. 5.0±0.6 d/wk, respectively, P=0.10) (Table 4). Screen time and treat food consumption were not different between groups.
Table 4. Lifestyle habits for completers in each Intervention group during the 12-week study period.| BF (n=7) | Control (n=8) | Endpoint group comparison | |||
| Week 1 | Week 12 | Week 1 | Week 12 | P-value | |
| Breakfast (d/wk) | 6.1±0.6 | 6.3±0.4 | 4.4±0.6 | 5.0±0.6 | 0.10 |
| Treat food (number/wk) | 8.4±1.9 | 8.3±3.1 | 9.6±1.9 | 9.0±1.3 | 0.82 |
| Screen time (hours/wk) | 14.9±3.3 | 16.7±3.3 | 12.4±2.4 | 14.0±3.8 | 0.60 |
Discussion
We found no significant change in weight status in response to an intervention that emphasized RTE cereal consumption for breakfast compared to usual weight loss education in overweight, habitual breakfast skipping children. Despite no statistically significant difference between groups, children in the BF group had an overall decrease in BMI from baseline, while children in the control group had the opposite response. However, children in the BF group reported significant improvements in diet quality and had lower reported intakes of sugars and higher reported intakes of vitamin A, vitamin D, riboflavin, niacin, folate, vitamin B6, vitamin B12, and iron at the end of the study compared to children in the control group. Children in the BF group also reported a significantly greater amount of physical activity at endpoint than children in the control group and they reported consuming breakfast almost daily. These data show that our healthy eating counseling sessions, emphasizing breakfast consumption and providing RTE cereal, were effective in improving the diet quality of obese, non-breakfast consumers compared to dietary counseling alone.
Studies suggest that breakfast consumption and childhood obesity are inversely associated. It was hypothesized that increasing breakfast consumption would reduce BMI. Despite the lack of statistical significance, weight status did move in the predicted direction over this short-term study. It is important to note that this study had a very small sample size. Rosado et al.10 performed an intervention study with 4 intervention groups: a group that received a serving of RTE cereal for breakfast, a group that received a serving of RTE cereal for breakfast and dinner, a group that received a serving of RTE cereal for breakfast and attended nutrition education sessions, and a control group, to test whether breakfast type influenced weight status in children ages 6-12 y. In contrast to the current study, Rosado et al.10 did not target breakfast skippers specifically. The results showed that, compared to the control group, only the consumption of RTE cereal for breakfast and attendance at nutrition education sessions led to a reduction in body weight and BMI. Rosado et al.10 had 147 participants in their study compared to 16 completers in the present study. This difference in sample size could explain the lack of group differences. A sample size analysis conducted at 80% power revealed that 174 participants would have been needed to detect a difference in BMI change with 95% confidence based on the data obtained in the present study. Due to challenges faced in recruitment and budgetary constraints, this sample size was not feasible for the current investigation and additional studies are needed. Additionally, future, larger studies, should assess changes in body fat content and include additional control groups without dietary counseling but with and without RTE cereal provision. However, the intent here was to educate children on good nutritional practices and determine whether providing breakfast cereal to encourage breakfast consumption would have an added benefit.
Children in the BF group reported greater intakes of vitamin D, riboflavin, niacin, folate, iron, vitamin B6, and vitamin B12 at endpoint than children in the control group. These improvements in dietary quality are likely due to the consumption of fortified RTE cereal provided in the study. Tucker et al.14 found that increased consumption of RTE cereal was associated with increased plasma folate concentrations, increased plasma vitamin B12 concentrations, and increased plasma vitamin B6 concentrations over a 14-wk period in older adults. Daily riboflavin intake levels were higher for children who consumed RTE cereal than those who did not.15 Also, the increase in vitamin D in the BF group could have been due to their consumption of RTE cereal with milk. A study by Hill et al.16 showed that RTE cereal was one of the top ten sources of vitamin D for Americans, mostly due to the associated milk intake. However, in this study, changes in calcium intakes were not different between groups
This study had several limitations, including a small sample size. Complete data were available for only 8 children in each group. Failure to start the study after randomization was particularly troublesome. Five children failed to attend the first session after being randomized. Also, many families had difficulty attending dietary counseling sessions regularly. For those in the BF group, this could have resulted in a reduced availability of RTE cereal since those were dispensed at counseling sessions, which could have impacted consistent breakfast consumption. It was also difficult to recruit low breakfast consumers of elementary school age. In New York City elementary public schools, breakfast is available free of charge to all students in schools before classes.
One item to consider in future breakfast intervention studies, besides a longer study period or follow-up measurements, is increased familial involvement. It is difficult to change habits in children without instilling a desire to adopt a healthy lifestyle in the parents as well. A review on this topic reported that randomized trials focusing on weight loss in children and adolescents showed more success when families were involved.17 In fact, when parents are the targets of health education, there is a greater reduction in childhood obesity than when children alone are targeted.18 Although our study allowed the parents to be present with their children for each lesson, this was not required and the lessons themselves were targeted at children. Perhaps adding a parental component would result in greater improvements in weight measures in the participating children.
Additionally, a review of childhood obesity interventions suggests that interventions aimed at weight loss in obese children are more effective when they combine dietary interventions with physical activity and behavior change components.19 The present study suggests that increasing healthy breakfast consumption among overweight or obese non-breakfast consumers has the potential to improve weight status. Perhaps, if this approach was combined with other intervention strategies, it could be even more effective. This should be considered in future studies.
Conclusion
In conclusion, this study found that nutrition counseling focusing on breakfast consumption, coupled with provision of RTE cereal, results in improvements in diet quality without affecting weight status. However, our small sample size limited our ability to detect significant differences in change in BMI and waist circumference between groups. Nevertheless, our data suggest that our intervention may lead to beneficial, albeit small effects on body composition. Further research is necessary to determine whether sustained improvements in breakfast consumption leads to lasting effects on diet quality and ultimately affect weight status in obese children.
Acknowledgements
MS and KK conceived experiments. MS and CB carried out experiments. All authors were involved in analyzing the data, writing the paper and had final approval of the submitted material.
This publication was supported by a Covidien pilot grant through The Obesity Society, the National Center for Advancing Translational Sciences, National Institutes of Health, through Grant Number UL1 TR000040, formerly the National Center for Research Resources, Grant Number UL1 RR024156, the New York Obesity Nutrition Research Center Grant Number P30-DK26687. General Mills provided cereal for the study.
Conflicts of Interest Statement
The authors have no conflicts of interest to report. None of the funding sources played any role in the study conduct and data interpretation.
References
- 1.Mathieu P, Poirier P, Pibarot P, Lemieux I, Despres J P. (2009) Visceral obesity: the link among inflammation, hypertension, and cardiovascular disease. , Hypertension 53, 577-584.
- 2.C L Ogden, Carroll Kit B K, K M Flegal. (2012) . Prevalence of Obesity and Trends in Body Mass Index Among US Children and Adolescents,1999-2010. JAMA 307, 483-490.
- 3.Must A, R S Strauss. (1999) Risks and consequences of childhood and adolescent obesity. , Obesity 23, 2-11.
- 4.P M Gleason, A H Dodd. (2009) School breakfast program but not school lunch program participation is associated with lower body mass index. , J. Am. Diet. Assoc 109, 118-128.
- 5.Baldinger N, Krebs A, Muller R, Aeberli I. (2012) Swiss children consuming breakfast regularly have better functional skills and are less overweight than breakfast skippers. , J. Am. Coll. Nutr 31, 87-93.
- 6.K E Alexander, Ventura E E, Spruijt-Metz D, M J Weigensberg, M I Goran. (2009) Association of breakfast skipping with visceral fat and insulin indices in overweight Latino youth. , Obesity (Silver Spring) 17, 1528-1533.
- 7.K J Smith, S L Gall, S A McNaughton, Blizzard L, Dwyer T. (2010) Skipping Breakfast: longitudinal associations with cardiometabolic risk factors in the Childhood Determinants of Adult Health Study. , Am. J. Clin. Nutr 92, 1316-1325.
- 8.P R Deshmukh-Taskar, T A Nicklas, C E O’Neil, D R Keast, J D Radcliffe. (2010) The Relationship of Breakfast skipping and Type of Breakfast Consumption with Nutrient Intake and Weight Status in Children and Adolescents: The National Health and Nutrition Examination Survey,1999-2006. , J. Am. Diet. Assoc 110, 869-878.
- 9.Balvin Frantzen L, Trevino R P, Echon R M, Garcia-Dominic O, DiMarco N. (2013) Association between Frequency of Ready-to-Eat Cereal Consumption, Nutrient Intakes, and Body Mass Index in Fourth- to Sixth-Grade Low-Income Minority Children. , J. Acad. Nutr. Diet 113, 511-519.
- 10.Rosado J L, M del R Arellano, Montemayor K, Garcia O P, Caamano Mdel C. (2008) An increase of cereal intake as an approach to weight reduction in children is effective only when accompanied by nutrition education: a randomized controlled trial. , Nutr. J 7, 28.
- 11.Achenbach T M. (1991) Manual for the Child Behavior Checklist/4-18 and Profile.Dept.ofPsychiatry,University of Vermont. , Burlington, VT
- 12.Wardle J, C A Guthrie, Sanderson S, Rapoport L. (2001) Development of the children’s eating behavior questionnaire. , J. Child. Psychol. Psyc 42, 963-970.
- 13.L H Epstein, Squires S. (1988) The Stoplight Diet for Children: An Eight-Week Program for Parents and Children, Little, Brown and Co. , Boston, MA
- 14.K L Tucker, Olson B, Bakun P, G E Dallal, Selhub J. (2004) Breakfast cereal fortified with folic acid, vitamin B-6, and vitamin B-12 increases vitamin concentrations and reduces homocysteine concentrations: a randomized trial. , Am. J. Clin. Nutr 79, 805-811.
- 15.J A Grieger, Cobiac L. (2012) Comparison of dietary intakes according to breakfast choice in Australian boys. , Eur. J. Clin. Nutr 66, 667-672.
- 16.Hill K M, Jonnalagadda S S, Albertson A M, Joshi N A, Weaver C M. (2012) Top food sources contributing to vitamin D intake and the association of ready-to-eat cereal and breakfast consumption habits to vitamin D intake in Canadians and United States Americans. , J Food Sci 77, 170-175.
- 17.B S Niemeier, J M Hektner, K B Enger. (2012) Parent participation in weight-related health interventions for children and adolescents: a systematic review and meta-analysis. , Prev. Med 55, 3-13.
Cited by (3)
- 1.Bohan Brown Michelle M., Milanes Jillian E., Allison David B., Brown Andrew W., 2020, Eating versus skipping breakfast has no discernible effect on obesity-related anthropometric outcomes: a systematic review and meta-analysis, F1000Research, 9(), 140, 10.12688/f1000research.22424.1
- 2.Bohan Brown Michelle M., Milanes Jillian E., Allison David B., Brown Andrew W., 2020, Eating versus skipping breakfast has no discernible effect on obesity-related anthropometric outcomes: a systematic review and meta-analysis, F1000Research, 9(), 140, 10.12688/f1000research.22424.2
- 3.Bohan Brown Michelle M., Milanes Jillian E., Allison David B., Brown Andrew W., 2021, Eating versus skipping breakfast has no discernible effect on obesity-related anthropometric outcomes: a systematic review and meta-analysis, F1000Research, 9(), 140, 10.12688/f1000research.22424.3
